Aesthetic Alteration of the Chin
Evaluation and Surgery
Hugo Obwegeser introduced the intraoral approach to completing an osseous genioplasty in 1957.74 More than half a century later, this relatively simple technique still remains underused when surgeons are asked to make cosmetic changes to the chins of their patients.
Anatomy of the Chin
The word chin describes a region of the face that includes both soft tissue and bone.79,125 The soft-tissue portion encompasses the labial mental fold superiorly, the oral commissures laterally (just anterior to the jowls), and the submental–cervical crease inferiorly. The bony portion of the chin encompasses the mandibular symphyseal region. It includes the region inferior to the root apices of the anterior teeth and the area in front of and below the mental foramen on each side. Within the soft tissues of the chin are found a series of paired muscles that include the mentalis, the quadratis labii inferioris, the triangularis, and the superior portions of the platysma that extend over the symphysis region.22 Attached to the genial tubercle of the chin posteriorly are the tendinous attachments of the geniohyoid and genioglossus muscles.66 The anterior bellies of the digastric muscles are attached to the posterior portion of the inferior border of the symphysis. The sensory innervation to the cutaneous chin, the lower lip, and the inner vestibule is derived from the mental nerve on each side. The motor innervation to the muscles within the soft tissues of the chin occurs through the marginal mandibular and cervical branches of the facial nerve.
Aesthetics of the Chin
In Western society, a “weak” or deficient chin is associated with timidity, indecision, femininity, a lack of athleticism, and shy behavior. Conversely, a “strong” or forwardly projecting chin is associated with athleticism, aggressiveness, decisiveness, and bold behavior. The fact that an average adult from any number of ethnic backgrounds and nationalities from around the world will frequently characterize a chin as either “weak” or “strong” demonstrates the subliminal messages communicated about the character of a person as a result of the presenting chin morphology. When people speak about chin contour, emphasis is generally placed on the profile view (Fig. 37-1).2,13,90,91 Although it is true that a retrusive pogonion is a frequently mentioned concern, the chin may also be asymmetric or out of the normal range in more than one dimension.

Figure 37-1 A 29-year-old woman arrived to discuss her chin aesthetics. During the mixed dentition, she was recognized as having mandibular deficiency and a constricted maxillary arch width. At that time, she underwent growth-modification techniques, including the use of headgear. She also underwent rapid palatal expansion followed by compensatory orthodontic mechanics to neutralize the occlusion, but this resulted in proclination of the incisors. A retrusive profile and a dual bite remained. She recently underwent the placement of an extended silastic chin implant but without fixation by another surgeon. Aesthetic modification of the anterior maxillary dentition was also completed by a restorative dentist. She is displeased with the cosmetic facial results of a deepened labiomental fold, a mobile chin implant, and a “button” appearance during lip closure. There is a dual bite with Class II malocclusion in centric relation. A, Oblique and frontal facial views after chin implant placement. B, Profile facial view and lateral cephalometric radiograph 6 months after chin implant placement.
When it is taken with the patient in the natural head position, with the lips relaxed (i.e., in repose) and with the lower jaw at rest (i.e., the condyles seated in the fossa and with a normal freeway space between the teeth), a lateral cephalometric radiograph provides an accurate image of the facial skeleton and the overlying soft tissues from which to judge profile aesthetics.28,30,31,43,44,83,105,112 When viewing either a full-face lateral photograph or a soft-tissue lateral cephalometric radiograph taken in this way, a vertical line (i.e., perpendicular to the floor with the patient in the natural head position) can be drawn through the subnasal region to assess the relative prominence of the nose, lips, and chin.36 Ideally, the chin should lie on this line, with the lips slightly anterior (Figs. 37-2 through 37-5).9 It is also true that there are many complex interrelationships among the facial structures that should be taken into consideration.1–3,51,52,60,69,95,118 Critical decisions with regard to where to position the chin through osseous genioplasty are made when viewing the patient “face to face” from varying perspectives in repose and during broad smile in the clinic setting.4,16,124,126
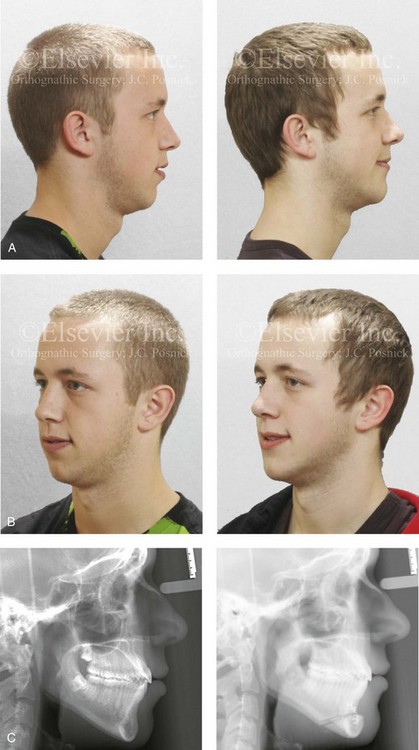
Figure 37-2 A 17-year-old boy arrived with his father for the evaluation of a “weak chin” and requested chin augmentation. He had undergone orthodontic treatment with the establishment of a satisfactory occlusion that required minimal dental compensation. He agreed to undergo osseous genioplasty (horizontal advancement) to resolve the chief complaint. A, Profile views before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Lateral cephalometric radiographs before and after reconstruction.

Figure 37-3 A 16-year-old girl arrived with her mother and requested a cosmetic rhinoplasty to reduce the dorsal hump and to improve the drooped nasal tip seen in profile. She also had a lifelong history of nasal obstruction. Evaluation confirmed the aesthetic nasal needs as well as sagittal deficiency of the chin. She agreed to undergo septorhinoplasty and osseous genioplasty. The rhinoplasty included nasal osteotomies (in-fracture); dorsal reduction (bone and cartilage) and tip maneuvers (modification of lower lateral cartilages and septal cartilage caudal strut grafting); septoplasty; and the reduction of the inferior turbinates. Osseous genioplasty included horizontal advancement. A, Profile facial views before and after reconstruction. B, Oblique facial views before and after reconstruction.

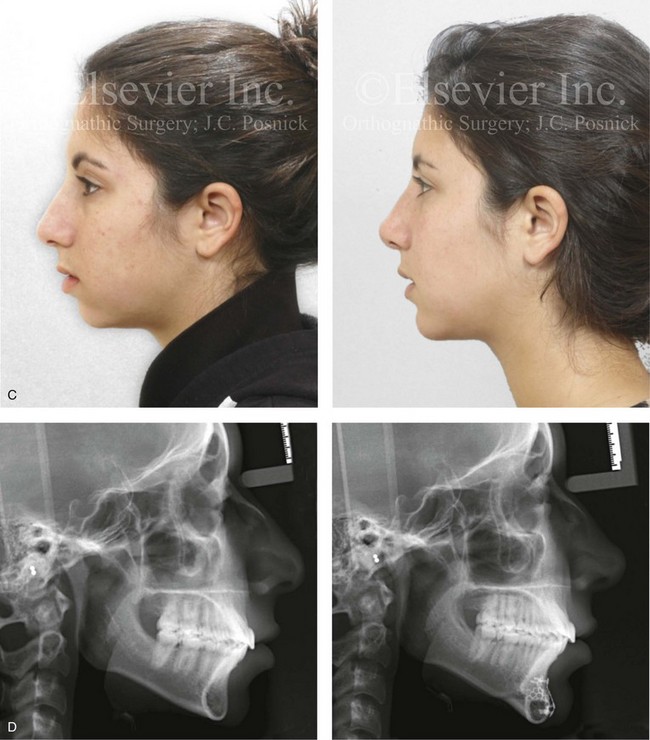
Figure 37-4 A 17-year-old girl arrived with her mother and requested a cosmetic rhinoplasty to reduce the dorsal hump and to improve the drooped nasal tip seen in profile. She also had a lifelong history of nasal obstruction. Evaluation confirmed the aesthetic nasal needs as well as sagittal and vertical deficiency of the chin. She agreed to undergo septorhinoplasty and osseous genioplasty. The rhinoplasty include nasal osteotomies (in-fracture); dorsal reduction (bone and cartilage) and tip maneuvers (modification of lower lateral cartilages and septal cartilage caudal strut grafting); septoplasty; and the reduction of the inferior turbinates. Osseous genioplasty included horizontal advancement and vertical lengthening with interpositional grafting (bloc hydroxyapatite). A, Frontal views in repose before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Profile facial views before and after reconstruction. D, Lateral cephalometric radiographs before and after surgery.


Figure 37-5 An 18-year-old girl arrived with her parents and requested a cosmetic rhinoplasty and a chin implant. She hoped for a smaller nose, a reduction of the dorsal hump, and a stronger profile. She also had a history of nasal obstruction after a sports injury earlier during her life. Examination confirmed mild sagittal deficiency of the mandible but with a functional occlusion and minimal dental compensation after earlier orthodontic treatment. She agreed to undergo septorhinoplasty and osseous genioplasty. The patient’s nasal procedures included nasal osteotomies (in-fracture); dorsal reduction (bone and cartilage); tip maneuvers (modification of lower lateral cartilages and septal cartilage caudal strut grafting); septoplasty; the reduction of the inferior turbinates; and osseous genioplasty with horizontal advancement. A, Frontal views in repose before and 8 years after reconstruction. B, Oblique facial views before and 8 years after reconstruction. C, Profile views before and 8 years after reconstruction. D, Lateral cephalometric radiographs before and 8 years after reconstruction.
Biologic Foundation of Osseous Genioplasty
When carrying out an osseous genioplasty, a horizontal osteotomy below the roots of the anterior teeth and the mental foramen on either side is completed. After osteotomy, the distal segment of the chin remains attached to a musculoperiosteal pedicle. Healing is optimal when the circulation of blood to bone and its enveloping soft tissue is continuously maintained. In 1988, Bell and colleagues completed microangiographic and histologic studies in adult rhesus monkeys that indicated that an intraoral pedicled flap that involved an osteotomy of the inferior mandibular border maintains circulation and osseous viability after manipulation and repositioning of the chin segment.106 According to Bell’s experimental work, circulation to the dental pulp should not be discernibly affected during the process.
Frequent Patterns of Chin Deformities
Horizontal Chin Deficiency with or without Vertical Discrepancy
Contemporary maxillofacial surgeons now recognize that individuals who are seeking a “stronger chin” (i.e., horizontal projection) frequently also have disproportions in the vertical dimension of their face.23,33,45,59,61,77,88,89,92,116,120,123,127,131 Studies suggest that approximately 40% of individuals with horizontal (sagittal) chin deficiency have a decreased lower anterior facial height (i.e., short face growth pattern) (Figs. 37-4, 37-6, and 37-7). It is also known that another 25% of these will have the other extreme of an increased lower anterior facial height (i.e., long face growth pattern) (Figs. 37-8 through 37-11). In either case, the bony chin dysmorphology will also result in soft-tissue abnormalities (distortions) of the labiomental fold. This often includes a deep labiomental angle in those with a short face growth pattern and a flat labiomental fold in those with a long face growth pattern. Fifty percent of individuals with a horizontally deficient chin will have an Angle class II malocclusion, which is indicative of mandibular retrusion. Forty percent will have previously undergone orthodontic camouflage treatment in an attempt to mask their micrognathia (see Fig. 37-1). Incisor flaring will have resulted from the orthodontic camouflage approach that attempted to neutralize a Class II excess overjet malocclusion as an alternative to a more biologic correction of the mandibular deficiency through orthognathic surgery. Some of these individuals will have also undergone chin implant augmentation, often with a suboptimal result (see Fig. 37-1, 37-7, and 37-9).

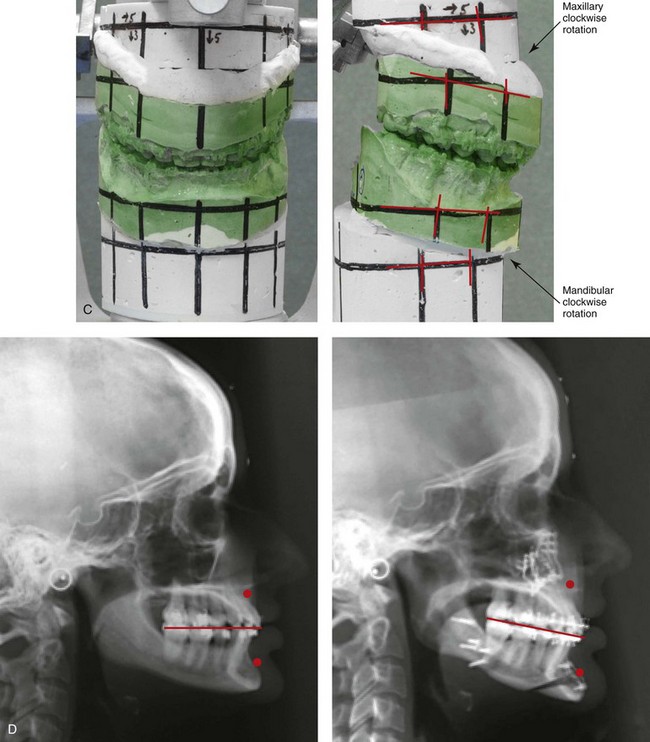
Figure 37-6 A 24-year-old woman arrived for evaluation. She had previously undergone four bicuspid extractions and orthodontics to neutralize her occlusion during her high school years. Analysis confirmed a short face growth pattern that accounted for her apparent large nose, weak profile, obtuse neck chin angle, and edentulous look. She agreed to a combined orthodontic and surgical approach. The patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation) with interpositional grafting; sagittal split ramus osteotomies (horizontal advancement and clockwise rotation); and osseous genioplasty (vertical lengthening and minimal horizontal advancement) with interpositional grafting. Minimal change in the occlusion was required (see Fig 23-3). A, Frontal views in repose before and after treatment. B, Oblique facial views before and after treatment. C, Articulated dental casts that indicate analytic surgical planning. D, Lateral cephalometric radiographs before and after treatment.

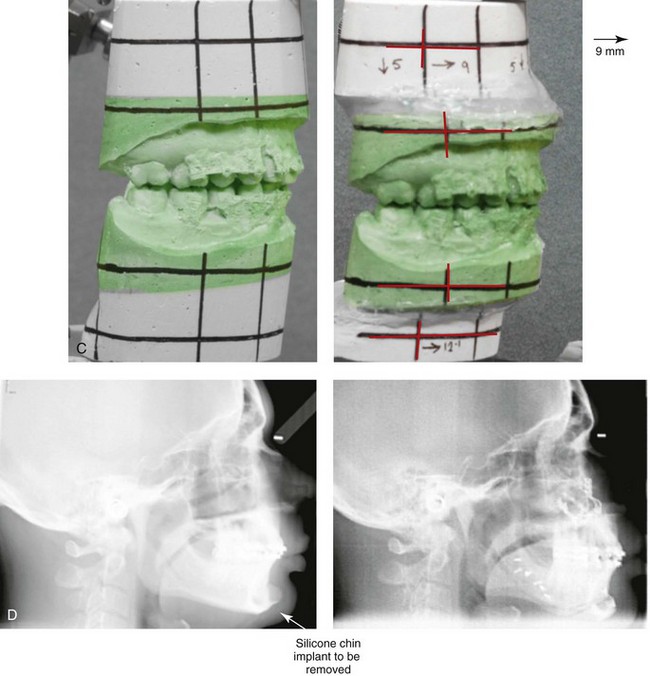
Figure 37-7 A 37-year-old man was referred with a request to have a chin implant removed because he was displeased with the aesthetic results. When he was 20 years old, he underwent chin augmentation with a silicone implant in an attempt to camouflage his small lower jaw profile. Ten years later, he underwent four bicuspid extractions and orthodontic alignment to improve his occlusion. He had also undergone a septorhinoplasty procedure, but he was still experiencing continued difficulty breathing through the nose. During evaluation by this surgeon, he was recognized as having a short face growth pattern with decreased lower anterior facial height and limited facial projection. There was an accentuated labiomental lip curl and a “button” appearance to the chin. It became clear during a discussion that the patient suffered with snoring, restless sleeping, and excessive daytime fatigue. An attended polysomnogram confirmed a respiratory disturbance index of 16 events/hr, with desaturations of up to 89%. A titration study confirmed the need for 12 cm of water pressure to reduce the respiratory disturbance index to 3 events/hr. The use of continuous positive airway pressure was attempted but found to be uncomfortable and difficult for the patient to use. A, Frontal views with smile before and after surgery. B, Profile views before and after surgery. Consultations with a sleep specialist, an otolaryngologist, and an orthodontist confirmed the advantage of an intranasal and orthognathic surgical approach. The patient agreed to perioperative orthodontics and surgery to improve the airway and facial appearance. His procedures included maxillary Le Fort I osteotomy (horizontal advancement +9 mm, vertical lengthening +5 mm), with interpositional grafting; bilateral sagittal split osteotomies of the mandible (horizontal advancement +12 mm); removal of the chin implant; osseous genioplasty (horizontal advancement and vertical lengthening) with interpositional grafting; reduction of the inferior turbinates; redo septoplasty; and an anterior approach to the neck (cervical flap elevation, defatting, and vertical platysma muscle plication). As a result of the procedures, the patient experienced relief of his snoring, improved quality of sleep, diminished daytime fatigue, and improved breathing during the day. Six months after surgery, he underwent an attended polysomnogram that indicated a normal sleep study with no snoring or apnea events (see Fig. 26-10). C, Articulated dental casts that indicate analytic surgical planning. D, Lateral cephalometric radiographs before and after surgery (note the preoperative chin implant).

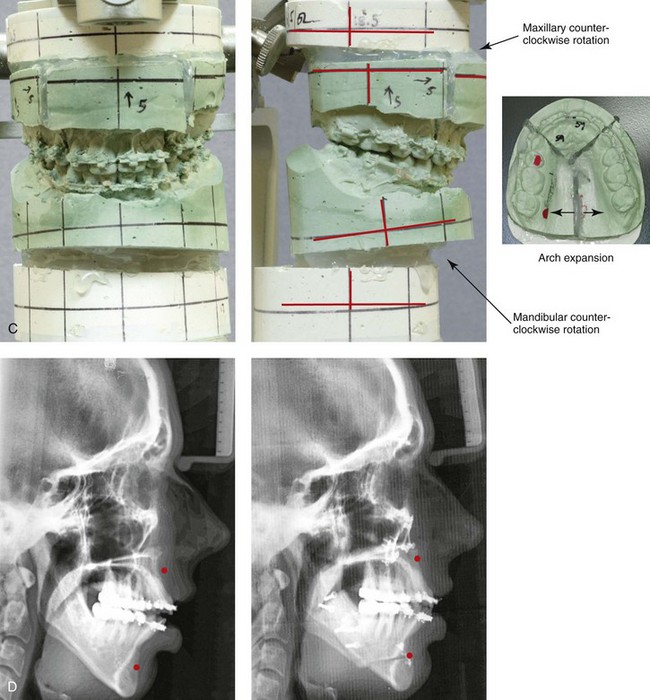
Figure 37-8 A 21-year-old college graduate arrived for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction, lip incompetence, difficulty chewing, and frequent speech articulation errors. Facial aesthetic concerns include a weak chin, a gummy smile, lip strain, and the impression of having a “big nose.” The patient had been under an orthodontist’s care since the mixed dentition and through her high school years. Growth modification attempts followed by rapid palatal expansion and full bracketing with four bicuspid extractions were unsuccessful to close the anterior open bite. Early periodontal and dental deteriorization were evident. Further evaluations were carried out by a speech pathologist, an otolaryngologist, and a periodontist; in addition, a fresh look was taken at this patient’s orthodontic needs. Orthodontic dental decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures that were carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, counterclockwise rotation, arch expansion, and correction of the curve of Spee); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring (see Fig. 21-5). A, Frontal views in repose before and after reconstruction. B, Profile views before and after reconstruction. C, Articulated dental casts that indicate analytic model planning. D, Lateral cephalometric radiographs before and after surgery.


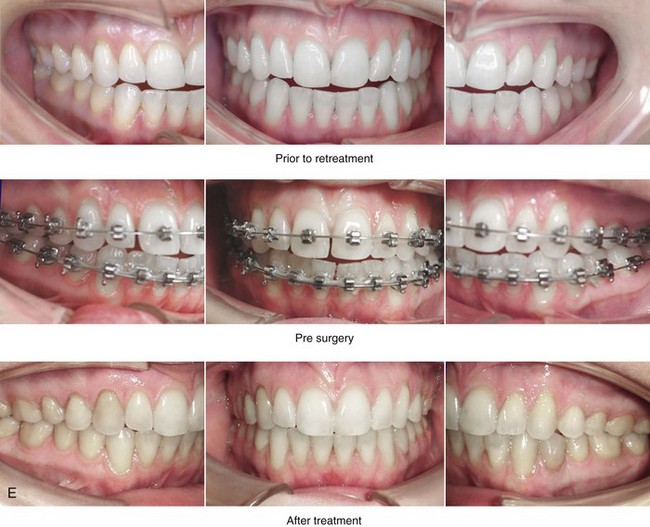
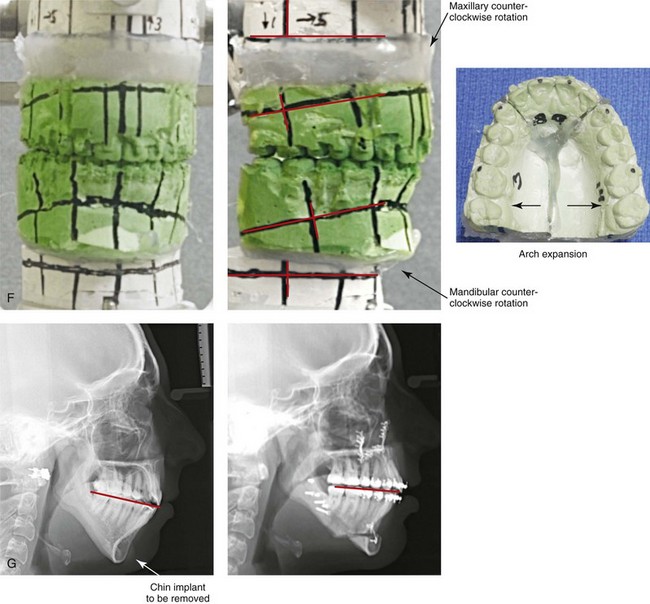
Figure 37-9 A 21-year-old college graduate arrived for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction, heavy snoring, lip incompetence, difficulty chewing, and frequent speech articulation errors. Facial aesthetic concerns included a weak chin, a gummy smile, and the impression of having a “big nose.” She had been under an orthodontist’s care from the mixed dentition through her high school years. Growth modification followed by rapid palatal expansion and full bracketing with attempted closure of the anterior open bite were attempted, without success. She had undergone a chin implant in an attempt to improve the profile, but this was also suboptimal. Further evaluations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at this patient’s occlusal/dental needs. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures that were carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, counterclockwise rotation, arch expansion, and correction of the curve of Spee); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); removal of the chin implant; osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before retreatment, with orthodontic decompensation in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery. Note that the chin implant was inadequate to improve the profile. An osseous genioplasty in addition to an orthognathic correction achieved the chosen objectives.

Figure 37-10 Intraoperative views of four silicon/Silastic chin implants removed from four separate patients who had suffered complications and suboptimal results and who had requested chin implant removal.

Figure 37-11 A woman in her early 50s with facial aging concerns. She had a mild long face growth pattern and a satisfactory occlusion. The lower anterior facial height was increased, which resulted in mild lip incompetence and mentalis strain as well as deep perioral creases. She agreed to blepharoplasty (elliptical excision of upper lid skin and redraping of lower lid tissue); osseous genioplasty (vertical reduction and horizontal advancement); and a face lift (see Fig. 40-9). A, Frontal views before and after surgery. B, Profile views before and after surgery. Note the relief of the perioral folds and mentalis strain as a result of vertical reduction and advancement genioplasty.
A pleasing labiomental fold is an essential component of optimal lower face aesthetics. A strong correlation exists between the lower anterior facial height and the labiomental fold morphology. Individuals with decreased lower anterior facial height in combination with a retrusive-appearing chin tend to have an exaggerated and excessively deep labiomental fold with acute angulation between the lower lip and the soft-tissue chin pad (i.e. primary mandibular deficiency or maxillomandibular deficiency; see Figs. 37-4, 37-6, and 37-7). Individuals with increased lower anterior facial height in combination with a horizontally deficient chin are likely to have a labiomental fold that is flattened and effaced, with poor fold definition, excess mentalis strain, and difficult lip closure (i.e., long face growth pattern). The long face growth pattern classically consists of vertical excess of the maxillary and mandibular alveolar regions. This is combined with mandibular retrognathia and an anterior open-bite Class II malocclusion (see Figs. 37-8 and 37-9).
Rosen and others have pointed out that many individuals with mandibular deficiency and decreased lower anterior facial height who have a functional occlusion are unwilling to undergo an orthognathic correction and may opt for a compromise approach to at least achieve some aesthetic advantage (Figs. 37-12 through 37-17).88–93An osseous genioplasty to simultaneously vertically lengthen and horizontally advance the chin will generally achieve a degree of improved lower facial height and chin projection while reducing the deep labiomental fold. When this compromise is undertaken, no improvement in any baseline malocclusion or any significant opening of the airway should be expected. From an aesthetic perspective, it is essential to prevent an operated look when choosing a chin-only approach. This aesthetic error can be limited by avoiding the temptation to fully correct a moderate to severe mandibular deficiency through an isolated chin procedure (see Figs. 37-13 and 37-15).
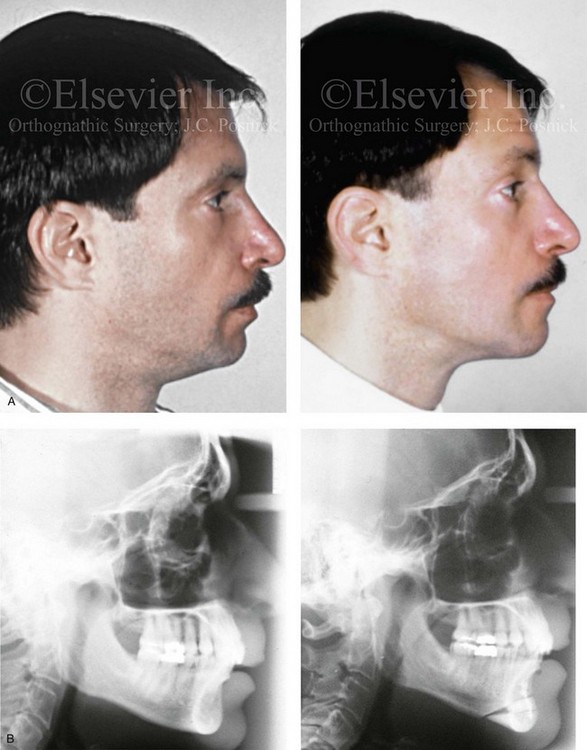
Figure 37-12 A Caucasian man in his 30s arrived for the evaluation a “weak chin” and requested aesthetic improvement. Examination confirmed a mild developmental mandibular deficiency (see Chapter 19). Successful orthodontics had been carried out during his teenage years, with only mild flaring of the mandibular incisors. An osseous genioplasty was agreed to that included significant vertical lengthening and limited horizontal advancement with interpositional bloc hydroxyapatite grafting. A, Profile views before and after reconstruction. B, Lateral cephalometric radiographs before and after reconstruction.

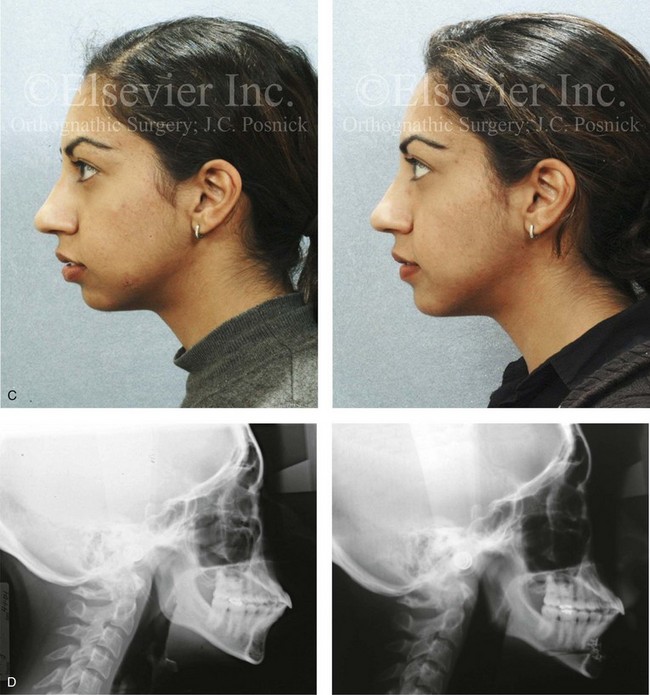
Figure 37-13 A 27-year-old Indian woman arrived and requested of a reduction rhinoplasty and a chin implant to treat her perceived “big nose” and “small chin.” Analysis confirmed maxillomandibular sagittal deficiency that was treated during her teenage years with compensatory orthodontics to neutralize the occlusion. There was marked procumbency of the maxillary and mandibular anterior dentition but with adequate tooth and gingival show, without lip incompetence and with good to the periodontium. The nasal aesthetic unit had thick skin but satisfactory proportions. The patient lacked lower anterior facial height and facial projection, especially at the pogonion. She was treated with an osseous genioplasty (vertical lengthening and limited horizontal advancement) and interpositional bloc hydroxyapatite grafting. A, Frontal views before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Profile views before and after reconstruction. D, Lateral cephalometric radiographs before and after reconstruction.


Figure 37-14 A woman in her early 20s arrived for the evaluation of her facial aesthetics. She had a developmental jaw deformity that was characterized primarily by mandibular deficiency and a lifelong history of obstructed nasal breathing. During her teenage years, she underwent an orthodontic camouflage approach that included maxillary bicuspid extractions with anterior dentition retraction to achieve an improved occlusion. She perceived a “big nose” and a “small chin” and requested reduction rhinoplasty and a chin implant. She refused redo orthodontics and an orthognathic correction (see Chapter 19). A compromise was agreed to that included open rhinoplasty and osseous genioplasty. The patient’s rhinoplasty included nasal osteotomies (in-fracture and straightening); dorsal reduction (bone and cartilage); and tip maneuvers (modification of lower lateral cartilages and septal cartilage caudal strut grafting). Osseous genioplasty included vertical lengthening with interpositional bloc hydroxyapatite grafting and minimal horizontal advancement. A, Frontal views with smile before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Profile views before and after reconstruction. D, Lateral cephalometric radiographs before and after reconstruction.



Figure 37-15 A woman in her mid 20s arrived for the evaluation of her facial aesthetics. She had a short face growth pattern (i.e., maxillomandibular deficiency) that was treated during her teenage years with compensatory orthodontic alignment only. An orthognathic correction to improve her horizontal facial projection and to increase the lower anterior facial height was recommended (see Chapter 23). She was unwilling to undergo further orthodontics and refused an orthognathic approach. A compromise was agreed to that included open rhinoplasty and osseous genioplasty. The patient’s rhinoplasty included nasal osteotomies (in-fracture and straightening); dorsal reduction (bone and cartilage); and tip maneuvers (modification of lower lateral cartilages and septal cartilage caudal strut grafting). Osseous genioplasty included vertical lengthening and minimal horizontal advancement with interpositional bloc hydroxyapatite grafting. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Lateral cephalometric radiographs before and after reconstruction.

Figure 37-16 A woman in her early 50s requested an evaluation of a “weak chin,” deep perioral creases, mild ptosis of the brow and upper eyelids, and unfavorable nasal aesthetics. Examination confirmed mild drooping of the brow and mild excess skin of the upper eyelids. A developmental mandibular deficiency was unchanged over the years, and she had a functional occlusion. She agreed to a limited incision brow lift, but as a result of dryness of the eyes, decided against the removal of the skin of the upper lid. She also agreed to an osseous genioplasty that included vertical lengthening and horizontal advancement with interpositional bloc hydroxyapatite grafting. Her rhinoplasty included nasal osteotomies (in-fracture); dorsal reduction (bone and cartilage); and tip maneuvers (modification of lower lateral cartilages and septal cartilage caudal strut grafting). All procedures were carried out simultaneously. A, Oblique facial views before and after surgery. B, Profile views before and after surgery.
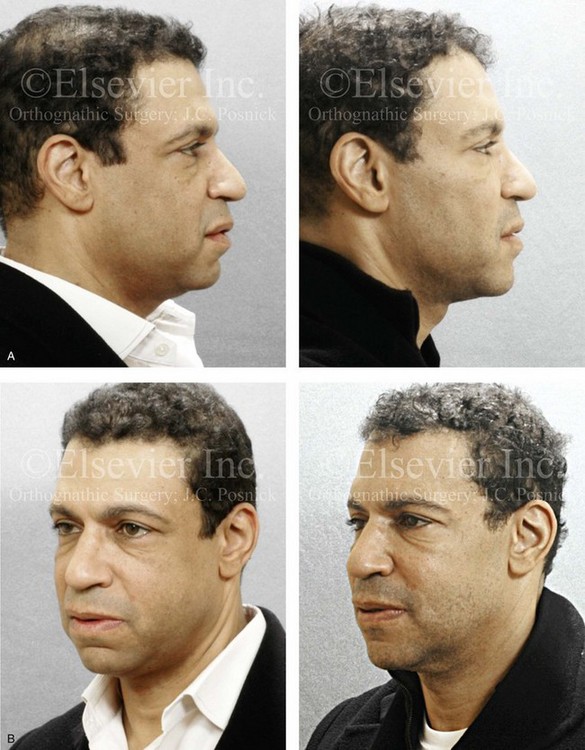
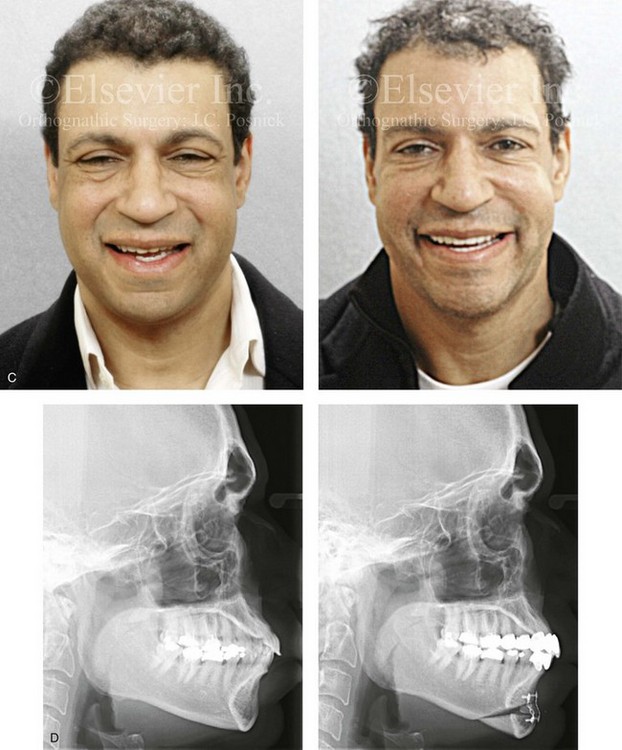
Figure 37-17 An African-American man in his early 40s underwent evaluation for a “weak chin” and laxity of the neck soft tissues. There was a degree of procumbency to the maxillary and mandibular dentition but with a stable occlusion. He also planned to undergo cosmetic modification of the anterior dentition. A treatment plan was agreed to that included osseous genioplasty (vertical lengthening with interpositional grafting and minimal horizontal advancement) and an anterior approach to the soft tissues of the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication). A, Profile views before and after surgery. B, Oblique facial views before and after surgery. C, Frontal views before and after surgery. D, Lateral cephalometric radiographs before and after surgery.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


