Histology and Embryology
General Histology
Cells
A Smallest structures and functionally self-contained units in the body; they vary in size, shape, and surface, depending on functional specialization (Figure 2-1)
B Cells possess similar common physiologic properties that permit:
a. Cells must have the ability to form substances that produce products to aid in the body’s function
b. Example—glands synthesize and secrete products to aid bodily functions
C The building blocks of tissues in the body are attached to each other and to noncellular surfaces by cell junctions; the structures of various types of cell junctions depend on location and function; the types of junctions are:
1. Desmosomes—cell-to-cell attachments; this type of attachment is found between ameloblasts (enamel-forming cells) and cells of the stratified squamous epithelium that lines the oral cavity
2. Tight junctions—cells attach to each other by fusion of their cell membranes; adjacent odontoblasts (dentin-forming cells) form tight junctions that prevent substances in the pulp from passing into the dentin
3. Gap junctions—contain a channel that runs between cells for communication of cell electrical impulses and passage of molecules; this type of junction is present among some odontoblasts, allowing them to coordinate their activity
4. Hemidesmosome—the attachment of a cell to a noncellular surface; the basal layer cells of stratified squamous epithelium attach to the basement membrane by hemidesmosomes; this attachment mechanism is present in the epithelial attachment to the tooth; the epithelial attachment refers to the basal lamina and hemidesmosomes that connect the junctional epithelium of the soft tissue to the tooth surface
D Cells are surrounded by a cell membrane that separates them from the extracellular environment; cell membrane encloses all components of the cell:
Specialization
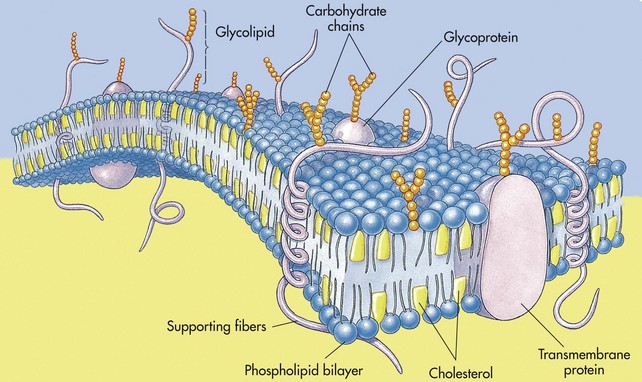
Cell Membrane
A Referred to as plasma membrane or plasmalemma; usually too thin to be seen with a light microscope; average width is approximately 7 nanometers (nm); considered selectively permeable because it controls passage of materials in and out of the cell
1. It surrounds the cell and is semi-permeable, allowing some substances to pass through it and others to be excluded
2. Its permeability may vary selectively by porous openings
3. Selective permeability characteristics:
a. Protecting cell from external environment
b. Permitting entrance and exit of selected substrates
c. Using active transport, passive transport, or facilitated diffusion
4. Its composition is a 3 : 2 ratio of proteins to lipids; lipids and proteins are the major components
5. Its structure is trilaminar, with a bipolar membrane and a central core of lipids between two layers of protein
6. The 0.8 nm pores in the surface allow diffusion of small lipid-insoluble substances
B Trilaminar structure composed of two facing layers of lipid molecules, into which large globular proteins are inserted (Figure 2-2)
Cytoplasm
A Translucent, aqueous, homogeneous gel enclosed in the cell by the cell membrane; organelles and inclusions are suspended in the cytoplasmic gel
B All metabolic activities of the cell occur in the cytoplasm, including:
Nucleus
A Controls the two major functions of the cell
B Genetic information stored in chromosomes for cell duplication; chromosomal deoxyribonucleic acid (DNA); the human nucleus contains 46 chromosomes
C Chromosomes are visible only during cell division, when they become long, coiled strands; at other times, chromosomal material is dispersed in granular clumps of material called chromatin
D Each nucleus contains one or more round, dense structures referred to as the nucleolus (plural, nucleoli); these produce ribosomal ribonucleic acid (RNA)—protein plus RNA; the nucleus also is surrounded by a nuclear membrane and contains nuclear matrix with chromosomes
Synthesis Activities
A Three types of RNA are necessary for protein synthesis
1. Messenger RNA (mRNA)—copies of short segments of deoxyribonucleic acid (DNA), the genetic code
a. mRNA can be compared with a tape that contains all the genetic information of proteins, but it must pass through the ribosomes attached to the endoplasmic reticulum (ER)
b. As the tape passes through the ribosomes, transfer RNA (tRNA) adds the exact amino acid to the newly forming proteins (Figure 2-3)
2. tRNA—carrier of specific amino acids (building blocks of proteins)
3. Ribosomal RNA—found floating freely in the cytoplasm (polyribosomes) or attached to the ER
B Protein synthesis also can occur on polyribosomes floating freely in the cytoplasm; proteins synthesized on the free polyribosomes are used in cellular metabolic processes; proteins synthesized on the ribosomes attached to the ER are transported out of the cell
Inclusions
A Transitory, nonliving metabolic byproducts found in the cytoplasm of the cell
B May appear as lipid droplets, carbohydrate accumulations (such as mucopolysaccharides), or engulfed foreign substances
Lysosomes
A Membrane-bound organelles responsible for the breakdown of foreign substances that are engulfed by the cell by the process of phagocytosis or pinocytosis
B Produced by a budding process from the Golgi complex, lysosomes form spherical vesicles containing powerful degradative or hydrolytic enzymes; enzymes are first produced by the ER and then transported to the Golgi complex
C During phagocytosis, lysosomes fuse with engulfed substances to form a secondary vesicle; the vesicle with digestive materials may remain in the cell as a residual body or be discharged outside of the cell
D Vitamins A and E and zinc are important stabilizers for the lysosome’s membrane
Golgi Complex
A The structure consists of stacks of closely spaced membranous sacs, in which newly formed proteins are concentrated and prepared for export out of the cell (Figure 2-4)
1. Small membrane-bound vesicles pinch off from the Golgi complex and form secretory granules (newly formed proteins)
2. Secretory granules attach to the inside of the cell membrane and are then discharged outside of the cell
B Responsible for secreting to the external environment a variety of proteins synthesized on the ER
C Major site of membrane formation and recycling
D Storage site for newly synthesized proteins
E Site for packaging and transporting many cell products (e.g., polysaccharides, proteins, and lipids)
F Synthesis site for lysosomes
G Also involved in the production of large carbohydrate molecules and lysosomes
Mitochondria
A Membranous structure bounded by inner and outer cell membranes; the membranes contain enzyme complexes in a particular array (e.g., tricarboxylic acid cycle enzymes); the inner part is formed into folds (cristae) that extend, like shelves, inside the mitochondria to provide an additional work surface area for the organelle; usually more than one mitochondria are present in a cell; the number depends on the amount of energy required by the cell
B Provides the chief source of energy for the cell (“powerhouse of the cell” by oxidation of nutrients) by enzymatic breakdown of fats, amino acids, and carbohydrates; transforms the chemical energy bond of nutrients into the high-energy phosphate bonds of adenosine triphosphate (ATP)
C A single cell may contain 50 to 2500 mitochondria, depending on the cell’s energy needs (Figure 2-5)
Endoplasmic Reticulum
A Extensive membranous system found throughout the cytoplasm of the cell; composed of lipoprotein membranes existing in the form of connecting tubules and broad, flattened sacs (cisternae); the outer membrane may or may not be covered with ribosomes. The two types are:
1. Granular or rough-surfaced endoplasmic reticulum (RER)
2. Agranular or smooth-surfaced endoplasmic reticulum (SER)
3. The membrane system functions to synthesize, circulate, and package intracellular and extracellular materials
B Proteins are synthesized on ribosomes attached to the ER and are transported to the Golgi complex for packaging
C The system contains enzymes involved in a variety of metabolic activities (e.g., lipogenesis and glycogenesis)
D SER has a number of diverse roles and is found in a variety of cell types
Filaments and Tubules
A Thread-like structures approximately 7 to 10 nm thick; thicker filaments are the same as those seen in muscle (protein myosin strands) and have been associated with contractility in cells
B Microfilaments act as a support system for the cell cytoskeleton
C Bundles of microfilaments form tonofibrils and become part of the attachment apparatus (desmosomes) between cells (see Figure 2-21, B).
Microtubules
A Delicate tubes, 20 to 27 nm wide, found in cells that are undergoing mitosis and alterations in cell shape (cell morphology)
B They have an internal support function, particularly in long cellular processes such as neurites or odontoblastic processes
C They have the capacity to direct intracellular transport through the cytoplasm
Internal Environment and Homeostasis
Transport Through the Cell Membrane
1. Definition—continuous movement of molecules among one another in liquids or gases
2. Molecules may move across a membrane
3. Direction of diffusion of a substance is from a region of high concentration to a region of low concentration, which is the diffusion gradient
4. If equal amounts of a substance are placed at either end of a chamber such as a cell, they diffuse toward each other, and the net rate of diffusion equals zero
5. Factors that affect the diffusion rate are as follows:
a. The greater the concentration difference, the greater is the diffusion rate
b. The greater the cross-sectional area of the chamber, the greater is the diffusion rate
c. The higher the temperature, the greater is the reaction rate
d. The lesser the square root of the molecular weight, the greater is the reaction rate
e. The shorter the distance traveled through the cell membrane, the greater is the reaction rate
6. How rapidly a substance can diffuse through the lipid matrix of the cell membrane is determined by the substance’s solubility in lipids
a. Oxygen, carbon dioxide, and alcohol can diffuse rapidly through the cell membrane because they are lipid soluble
b. Water is not lipid soluble and therefore must depend on another mechanism to diffuse through the cell membrane
7. Facilitated diffusion involves the use of a carrier substance to transport a non–lipid-soluble substance across the cell membrane
1. Definition—process of net diffusion of water through a semi-permeable membrane caused by a concentration difference
2. Osmotic pressure—pressure that develops in a solution as a result of the net osmosis into that solution; pressure is affected by the number of dissolved particles per unit volume of fluid
3. Isotonic solution—when placed on the outside of a cell, will not cause osmosis (e.g., 0.9% sodium chloride)
4. Hypertonic solution—when placed on the outside of a cell, will cause osmosis out of the cell (e.g., greater than 0.9% sodium chloride) and lead to crenation (shrinking) of the cell
5. Hypotonic solution—when placed on the outside of a cell, will cause osmosis into the cell (e.g., less than 0.9% sodium chloride) and lead to cell lysis
1. Process used by a cell when large quantities of a substance are needed inside of the cell and only a small amount of the substance is present in the extracellular fluid
2. Involves pumping the substance against its concentration gradient
3. Uses a carrier system and energy (ATP)
4. Keeps sodium extracellularly (sodium pump) and potassium intracellularly; important for the transmission of nerve impulses
5. Almost all monosaccharides are actively transported into the body
D Phagocytosis—movement of a solid particle into the cell
1. Cell wall invaginates around the particle
2. Pinches off from the rest of the membrane and floats inward
E Pinocytosis—movement of fluid into a cell; similar to phagocytosis, except that the cell invaginates around fluid
Cell Replication
A Mitosis—process of cell replication (Figure 2-6)
a. The genetic material of each chromosome replicates
b. Chromosomes are dispersed as chromatin material in the nucleus
a. Chromosomes coil and contract; each chromosome consists of a pair of strands called chromatids, which are held together by a centromere
b. The nuclear envelope disappears
c. The centriole divides, and the two centrioles move to opposite poles of the cell
Concepts Relating to Dental Tissues
A All calcified dental tissues are produced by secretory cells that require a great amount of energy in producing their organic matrices, which become calcified; organelles such as mitochondria play an important role in providing energy
B Mitochondria have been associated with the calcification (mineralization) process that occurs in dental tissues
C Cell organelles help maintain tissues after the initial formation by the cell; fibroblasts (i.e., connective tissue cells that are present in all tooth tissues except enamel) contain increased numbers of cell organelles; these additional organelles aid fibroblasts in their synthesizing and secretory functions
Basic Tissues
A At the beginning of human development, individual cells multiply and differentiate to perform specialized functions; groups of cells with similar morphologic characteristics and functions come together and form tissues
2. Intercellular substance—a product of living cells; a medium for the passage of nutrients and waste within the tissue; the amount of substance varies with different tissues
3. Tissue fluid—blood plasma that diffuses through capillary walls; the fluid carries nutrients to the intercellular substance and waste materials to capillaries
C Tissues in the human body can be classified into four types:
D Each of the four basic tissues may be further subdivided into several variations
Epithelial Tissue
B The epithelium consists exclusively of cells held together by specialized cell junctions (little intercellular material is present between cells); cells rest on an underlying connective tissue, the basement membrane
C Epithelial cells (keratinocytes) form continuous sheets (tissues) and perform the following functions:
1. Protection—covering all outer surfaces of the body (e.g., skin)
2. Absorption—forming the lining of all inner surfaces of the body (e.g., digestive tract)
D Epithelial tissue varies, depending on function—it may have surface specializations on its free surfaces
Surface Epithelia
A The epithelium is classified according to:
B Combined characteristics allow for six different types of epithelia (Figure 2-7) and locations:
1. Simple squamous—found in the walls of vessels
2. Simple cuboidal—lines the ovaries
3. Simple columnar—lines the intestines and the cervix of the uterus
4. Stratified squamous—lines the oral cavity
5. Stratified cuboidal and stratified columnar—line the large ducts of the major salivary glands
C Other intermediate forms of epithelium:
1. Pseudo-stratified columnar (e.g., trachea)—appears stratified but is, in fact, only one layer
2. Transitional (e.g., urinary tract)—resembles both stratified squamous and stratified cuboidal epithelia
D Other cell types found in the epithelium:
1. Melanocytes—produce melanin (pigmentation); intensity of brown skin color is not caused by the difference in the number of melanocytes present but by the difference in the rate of melanin production, the size of pigment granules, and the length of time of their preservation
2. Inflammatory cells—transient cells usually associated with inflammation
E The epithelium lining the oral cavity (oral mucosa) and the skin (dermis) is an example of stratified squamous epithelium
Connective Tissue
Connective Tissue Proper
A All connective tissue proper develops from the embryonic mesenchyme; contains large amounts and various types of intercellular material and few cells; highly vascular; has two main functions:
1. Provides mechanical and biologic support (supports organs and other structures)
2. Provides pathways for metabolic substances and thus aids in the distribution of nutrients
1. Bone—hard and calcified; serves supportive and protective functions
2. Cartilage—firm but flexible; serves a supportive function
3. Reticular—network of branching fibers; acts as a filter; loose and elastic; provides a connection between structures
4. Bone marrow—site where blood cells are manufactured
5. Lymphoid tissue (tonsils and lymph nodes)
6. Fat or adipose (special type of connective tissue composed of fat cells)—located under the skin; provides insulation
C Types of connective tissues—differ in composition of cell products and proportions of products present:
1. Dense connective tissue—consists predominantly of heavy, tightly packed collagen fibers; main function is to resist tension; this dense collagenous connective tissue is present in the gingiva
2. Loose connective tissue—collagen and reticulin fibers extending in all directions; the main function is to provide biologic support and fill the spaces between organs and tissues
Connective Tissue Components
1. Types of cells normally present:
a. Fibroblasts—produce the fibrous matrix and ground substance of connective tissue
b. Macrophages—capable of digestive activity
c. Mast cells—contain vesicles filled with heparin and histamine
d. Mesenchymal cells—primitive cells with the capability of differentiating into various connective tissue cells; they play a key role in the replacement of connective tissue lost as a result of injury or disease
2. Cells that are normally in the bloodstream but move in and out of the blood vessels into surrounding connective tissue when needed (wandering cells):
1. Matrix of connective tissue composed of some or all of the following fibers:
a. Collagen fibers—consist of three long polypeptide chains coiled in a left-handed helix to form a tropocollagen unit, which is assembled in a “quarter-stagger” model outside of the cell; fibers are highly resistant to tension and are part of the anchoring mechanism by which the connective tissue attaches the basement membrane (see Figure 2-20, B); the most abundant fibers found in connective tissue
b. Reticulin fibers—comparable with collagen fibers in their protein composition; usually found in the border areas between connective tissue and other tissues
c. Elastic fibers—consist of long fibrous proteins that differ in composition from collagen; are the branching fibers responsible for recoiling tissues when they are stretched
d. Oxytalan fibers—resemble elastic fibers in morphology and chemical composition; are believed to be immature elastic fibers
Types (Cartilage and Bone)
Cartilage
A Cartilage and bone are sister tissues, both highly specialized forms of connective tissue, whose intercellular substances have assumed particular properties that allow them to perform support functions
1. Very “bouncy,” resilient tissue that is specialized to resist compression; has a gel-like matrix in which the ground substance predominates over the intercellular matrix
2. Relatively avascular tissue
3. In humans, most of the embryonic skeleton is preformed as hyaline cartilage that is eventually replaced by bone (during endochondral ossification); depending on the location and loading pattern imposed on the cartilage, it may specialize to form fibrous or elastic cartilage
4. All mature cartilage is surrounded by the perichondrium, a fibrous connective tissue, which serves a biomechanical function; it acts as an attachment site for muscles and tendons
B Cartilage, like all types of connective tissue, has three components:
1. Cells—chondroblasts and chondrocytes
2. Fibrous matrix—type II collagen fibers and, in some cases, elastic fibers
3. Ground substance—proteoglycans, which have a protein core with side chains of chondroitin sulfate and keratan sulfate (glycosaminoglycans); because of the chemical nature and organization of proteoglycans, the ground substance can readily bind and hold water, which allows the tissue to assume a gelatinous nature that can resist compression and also permit some degree of diffusion through the matrix
b. Most abundant type of cartilage; forms the embryonic skeleton in humans; is best suited to resist compression; appears as a homogeneous, translucent tissue because its intercellular matrix dominates its collagenous fibers; the major type of fiber in collagen
2. Fibrous cartilage (fibrocartilage)
a. Has a very sparse amount of intercellular substance dominated by collagen fibers, which are in such proportion that they are visible through a light microscope and are seen running between the chondrocytic cells in the cartilage
b. Resembles tendons except for the presence of the chondrocytes enclosed in lacunae
c. Usually found in areas that are subjected to both compression and tension, as in:
a. In areas that are in need of elastic recoil, hyaline cartilage becomes highly specialized, and elastic fibers are added to its intercellular matrix, as in:
b. Elastic fibers are highly branched and form a delicate fibrous matrix, often obscuring the intercellular substance; fibers can be seen only through a light microscope when stained with a specific elastic stain
Bone
A A specialized vascular connective tissue composed of a mineralized organic matrix; the inorganic component of bone is hydroxyapatite:
1. Provides skeletal support and protection of soft tissues
2. Acts as a reservoir for calcium and phosphorus ions; when these two ions drop below a critical level in the blood (100 mg of calcium per 100 mL of blood, and 600 mg of phosphorus per/100 mL of blood), they can be withdrawn from the bone
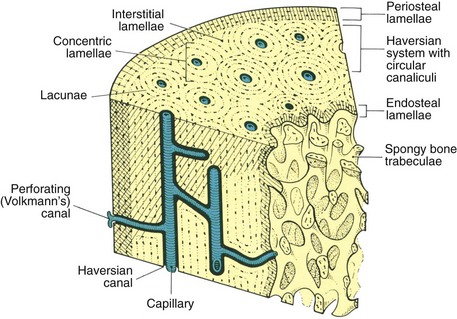
1. Compact bone—dense bone that appears as a continuous solid mass
2. Trabecular (cancellous or spongy) bone—composed of a central medullary cavity filled with either red or yellow marrow and with intervening spicules of bone (trabeculae); these trabeculae act to reinforce bone by increasing in number with increased function
1. Bone-forming cells (osteoblasts) are produced from undifferentiated mesenchymal cells of the periosteum, the endosteum, and the periodontal ligament
a. The periosteum is the connective tissue that covers the outer aspects of bone
b. The endosteum is a more delicate connective tissue lining the inner aspects of bone, the trabeculae, and Volkmann’s canals (canals of the bone containing blood vessels)
c. The periodontal ligament is specialized periosteum because it covers the outer aspects of the alveolar bone; it is also capable of forming bone and of forming cells that produce cementum (cementoblasts)
2. Osteoblasts become incorporated into bone during their formation; they occupy a space called lacuna (plural, lacunae)
3. Lacunae are connected to each other by means of a system of canals named canaliculi; these canals house the cytoplasmic extension of the osteocytes and provide a means for the transport of vascular components
4. Both compact and trabecular mature bones are formed in layers, or lamellae. Lamellae are found in three distinct types of arrangements present in all mature human bones (Figure 2-8):
a. Concentric, or haversian system, bone makes up the bulk of compact bone; it consists of lamellae arranged in concentric circles around a blood vessel (haversian canal) to form an osteon. An osteon, which consists of this concentrically arranged bone and haversian canal, is the basic metabolic unit of bone
b. Interstitial lamellae fill the space between the concentric circles of the haversian system bone
c. Lamellar bone is not arranged in concentric circles and is found on the surfaces of most bones. This bone is further defined by its location. When found on the outer aspects or the circumference of the bone underneath the periosteum, it is referred to as circumferential, or (sub)periosteal, bone; when found on the surfaces of trabeculae or the inner aspect of compact bone, it is referred to as (sub)endosteal bone
1. Bone, like all connective tissues, has three main components:
(1) Osteoblasts—bone-forming cells
(2) Osteoclasts—bone-resorbing cells
(3) Osteocytes—osteoblasts that are embedded in the lacunae of bone matrix and that maintain bone tissue
b. Fibrous matrix—collagen fibers (type I), which are the dominant component of bone matrix
c. Ground substance—proteoglycans containing chondroitin sulfates and seeded with the mineral salt hydroxyapatite
2. Bone is formed by osteoblasts developed in one of two ways:
a. Intramembranous ossification—mesenchymal cells move closer together (condensation), differentiate into osteoblasts, and begin to deposit bone matrix; this is how the maxilla and the mandible are formed
b. Endochondral ossification—future bone is preformed in a cartilage model that is eventually resorbed and replaced by new bone formed by osteoblasts (Figure 2-9)
F Structure of long bones (macroscopic)
1. The typical long bone is composed of:
a. Diaphysis (shaft)—thick compact bone forming a hollow cylinder with a central marrow cavity; this is the primary center of ossification in a long bone
b. Epiphyses (ends)—spongy bone covered by a thin layer of compact bone; these are the secondary growth centers
c. Metaphysis—transitional region between the epiphyses and the diaphysis, where the cartilage growth plate is located
d. All articular surfaces of long bones are covered by articular cartilage
2. While active, the epiphyseal growth plate usually has four zones, proceeding from first to last:
Blood and Lymph
1. Develops embryonically from mesenchymal cells that come together and form delicate tubular structures composed of endothelial cells
2. Consists of the heart, blood vessels, and lymphatics
a. Is a closed system that runs from the heart to the organs of the body and back to the heart
b. Between the heart and the organs, the blood vessels branch progressively into finer and finer vessels and finally enter the organs
(1) Here a delicate network of capillaries forms, called the capillary bed—the most essential part of the vascular system
(2) Exchanges of gases and substances occur in this capillary bed
c. Blood is then carried back to the heart via larger vessels, the veins
B Lymph vessels empty into filtering organs (nodes) and generally flow toward larger lymph vessels, the thoracic duct, and the right lymphatic duct; lymph enters the venous branches of the circulatory system
Blood Vessels
A Arteries—the largest of the blood vessels; walls are composed of:
1. A thick layer of smooth muscle cells
2. Elastic tissue—the largest amount is found in the large arteries close to the heart
B Veins—usually accompany arteries but carry blood in the opposite direction
2. Veins contain about 70% of total blood volume of the body at any given time
C Capillaries—the simplest of the blood vessels in the structure
1. Walls consist of a simple layer of endothelial cells and a basal lamina
2. Usually, the diameter of a capillary lumen is so small that only one blood cell at a time can pass through it
3. Capillaries form a barrier between blood and tissues
4. Transport of substances occurs at the capillary level through:
Microvasculature
A Composed of the smallest arteries and veins located in the capillary bed
1. At the end of the arterioles is a preferential channel that has several side branches entering the capillary bed
2. Blood passes through the capillary bed from the arterial side to the venous side
B Selective openings and closings of the capillary bed occur in the microvasculature to ensure regulation of the amount of blood throughout the body at any given time
Blood Components
Functions of Blood Cells
A Red blood cells (erythrocytes) contain hemoglobin, which carries oxygen from lungs to tissues
B White blood cells (leukocytes) function chiefly to fight infection, to scavenge foreign invaders, and to repair injured tissue
Lymphatic System
A Made up of a series of vessels that carry excess tissue fluid from the capillaries to filtering organs such as lymph nodes on the return to the bloodstream
B Lymph nodes are found along the lymphatic pathway
1. Consist of masses of lymph tissue that serve as a filtering system for the body
2. The tonsils and the spleen are both filtering organs for the body
3. Swollen and palpable lymph nodes may indicate that an infection is present somewhere in the body
C The function of lymph is to protect and maintain the internal fluid environment of the body
Nerve Tissue
A Main functions of the nervous system
1. Directs and maintains the complex internal environment of the body
2. Integrates and interprets incoming stimuli and directs appropriate responses at a conscious or unconscious level
B The nervous system can be classified as follows:
C Afferent nerves transmit impulses (sensations) from the periphery to the CNS (sensory input); efferent nerves transmit impulses (commands) from the CNS to muscles and other organs (motor output) (Figure 2-10)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses