Chapter 11
Soft Tissue Surgery Around Dental Implants
Aim
This chapter aims to provide a broad overview of the soft tissue surgical procedures that can be undertaken around dental implants and at what stage in the implant treatment they may be performed.
Outcome
Having read this chapter the reader will be aware of the factors influencing peri-implant soft tissues and will understand the use of techniques designed to improve the quality and distribution of peri-implant soft tissue as well as the timings of such procedures.
Introduction
Dental implants are now well established as part of the dental surgeon’s armamentarium for the management of missing teeth and are frequently the most suitable long-term replacement. Whilst there are many different designs of dental implants in terms of surface geometry, surface topography and prosthetic connections, the process of osseointegration is predictable and most implant systems demonstrate high levels of success in well-planned cases. There has been a shift, therefore, in recent years away from osseointegration per se towards soft tissue integration and improvements especially in aesthetic areas, although many clinicians are also realising the importance of robust peri-implant soft tissues in non-aesthetic areas.
Peri-implant Soft Tissue Characteristics
The soft tissues surrounding dental implants vary in thickness and level of keratinisation. This in turn affects their appearance and their resistance to oral hygiene measures, and may also affect their long-termpositional stability. An implant surrounded by thick keratinised immobile soft tissue is illustrated in Fig 11-1a, whereas Fig 11-1b shows an implant surrounded mainly by thin mobile inflamed non-keratinised mucosa. There is evidence to suggest that non-keratinised mobile tissue around implants has a greater potential for inflammation and this may be one of several factors that contribute to the long-term success or failure of such implants, particularly in the edentulous setting. Patient comfort during oral hygiene procedures can also be affected by the quality of the surrounding soft tissue and may be a reason for surgical intervention to make the tissue more robust.

Fig 11-1a Implant surrounded by immobile keratinised mucosa with no evidence of inflammation.
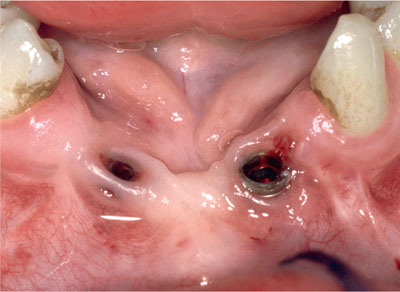
Fig 11-1b An implant with inflamed mobile labial alveolar mucosa.
Implants Do Not Have a Periodontal Ligament
There are subtle differences between the periodontal gingival soft tissues and those surrounding restored implants. Fundamentally, implants lack a periodontal ligament and the associated blood supply, and this affects the delicate “bundle bone” that lines the coronal part of the socket. The lack of a periodontal blood supply also means that the soft tissues around restored implants have a reduced blood supply compared with natural teeth. This has implications for peri-implant surgical techniques, and the need for meticulous surgical technique is thus paramount. In addition, “late” mucogingival techniques around implants to correct resulting soft tissue problems can be more difficult to undertake successfully than techniques undertaken prior to the final restoration of the implant. Every effort should be made to ensure that the quality/quantity of soft tissues is considered at the time of initial implant treatment and that any soft tissue surgery is planned as thoroughly as any bone surgery undertaken to allow successful implant placement.
Circular fibres predominate around implants, with no evidence of the horizontal inserting fibres that are found in abundance around teeth. This results in a very elastic “cuff” of tissue around the implant, although there is evidence of hemi-desmosomal attachment to some implant abutment surfaces.
Implant Components Affect Soft Tissue Behaviour
The components used to restore implants have effects on the peri-implant soft tissues. Every time a healing abutment is removed and replaced, micro-ulceration occurs and bleeding is generated on removal. Epithelial remnants on the surface of the abutment, if not removed prior to its repositioning, prevent re-attachment of the soft tissues via hemidesmosomes and this results in the epithelialisation of the inner layer of the peri-implant soft tissues. It is also clear that repeated removal and replacement of components at the fixture head level result in the development of inflammation, which can trigger crestal bone loss. The peri-implant soft tissues prefer materials such as titanium, ceramics and zirconium and seem to be able to form a good attachment to them. In contrast, cast gold alloys and plastic materials are not as biocompatible.
Soft Tissue Quality
High quality peri-implant tissues have the following characteristics:
-
immobile
-
keratinised with good height and width
-
good colour match to the surrounding tissues
-
absence of inflammation.
The quality of the surrounding soft tissues is dependent on a number of factors but is largely defined by the pre-existing state of the soft tissues at implant placement. This is mainly genetically determined and is referred to as the gingival biotype. Box 11-1 lists some of the factors that may influence peri-implant soft tissue quality.
Box 11-1 Factors affecting peri-implant soft tissue quality
Hereditary gingival biotype
Number of teeth missing
Time since extraction
Previous periodontal inflammation at the site
Previous flap surgery to the tooth prior to removal
Gingivectomy
Periradicular surgery
Surgery to address resorptive root lesions
Pre-implant bone grafting procedures
Implant surgery
Whilst the hereditary gingival biotype is an important factor in predetermining the thickness, degree of keratinisation and scalloping, previous flap surgery related to teeth as well as implant-related surgeries (such as buccal advancement flaps to cover autogenous pre-implant bone grafts or localised GBR, will all tend to reduce the quality of the soft tissues at the implant site.
Previous surgery often produces a degree of fibrous scarring, reduces the blood supply to the marginal tissues and may result in the coronal advancement of the mucogingival line towards the crest of the alveolus, bringing non-keratinised mobile alveolar mucosa with it.
There is also a tendency, several years after tooth extraction, for the gingival remnant to reduce with time to a very thin strip of keratinised tissue over the crest of the ridge, and in some cases this keratinised tissue can disappear altogether.
Mucogingival Procedures Around Implants
The requirement for mucogingival surgery at any given implant site will vary depending on the pre-existing soft tissue status and the requirements of the clinical situation to improve the soft tissue profile for patient comfort or for aesthetic reasons. Essentially, surgery is undertaken for one or more of the following reasons:
-
To facilitate the exposure of a two-stage implant.
-
To improve the quality of peri-implant mucosa from a thin mobile non-keratinised type to a more keratinised and immobile mucosa.
-
To increase the depth of the labial sulcus to improve access for oral hygiene measures.
-
To improve the quantity/thickness of peri-implant mucosa in order to correct a thin gingival biotype and as a result achieve a potentially more stable and aesthetic peri-implant mucosa.
In many cases the soft tissue procedure may address more than one of the above, and this is certainly true in the anterior maxilla where peri-implant bone grafting has been undertaken in conjunction with a submerged implant placement, especially in a patient with a thin biotype and a high lip-line. Soft tissue surgery is not, however, a substitute for adequate hard tissue management around dental implants; generally, soft tissues will only be stable if adequately supported by bone.
Types of Peri-implant Surgical Procedures
Many of the peri-implant techniques have been adapted from the mucogingival techniques used around teeth (see Chapter 9). The techniques used can be broadly classified into three groups:
-
Free soft tissue grafts:
-
epithelialised graft (free gingival graft)
-
connective tissue graft.
-
-
Local peri-implant soft tissue pedicled flap procedures.
-
A combination of free soft tissue graft and local peri-implant pedicled flap technique.
Timing of Surgical Procedures Around Implants
Whilst implant treatment can often be accomplished in a single surgical stage with good results, more complex clinical situations often require a staged approach to treatment with multiple surgical steps.
Peri-implant soft tissue procedures can be undertaken:
-
prior to implant placement
-
at the time of implant placement
-
prior to second stage implant surgery
-
at second stage implant surgery
-
around restored implants with problems (late procedures).
A number of/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


