Gingival and Dentogingival Junctional Tissue
Learning Objectives
• Define and pronounce the key terms in this chapter.
• List and describe each of the types of gingival tissue.
• Describe the histological features of the different types of gingival tissue.
• Describe the composition and discuss the development of the dentogingival junctional tissue.
New Key Terms
Basal lamina (bay-sal lam-i-nah): external, internal
Col (kohl)
Dentogingival junction (den-to-jin-ji-val), junctional tissue (jungk-shun-al)
Epithelial attachment (ep-ee-thee-lee-al)
Epithelium (ep-ee-thee-lee-um): junctional (jungk-shun-al), pocket, sulcular (sul-ku-lar)
Free gingival crest (jin-ji-vah), groove
Gingival crevicular fluid (jin-ji-val kre-vik-koo-ler), hyperplasia (hi-per-play-ze-ah), recession (re-sesh-un)
Gingivitis (jin-ji-vie-tis)
Periodontal pocket (pare-e-oh-don-tie-tis)
Periodontitis (pare-e-oh-don-tie-tis)
Gingival Tissue
Gingival tissue in the oral cavity is the most important tissue of the orofacial region for dental professionals to know and understand, and the most interesting as well. All the periodontal therapy performed, and homecare instruction given, are for the purpose of creating a healthy environment for the gingival tissue. Even with restorative care, the impact on the gingival tissue must be considered. When healthy, it presents an effective barrier to the barrage of periodontal insults to deeper tissue. Thus, the dental professional must have a clear understanding of the histology of the healthy, normal gingival tissue. This helps in understanding the pathological changes that occur during the disease states involving the gingival tissue. Overall, the clinical appearance of the tissue reflects the underlying histology, both in health and disease.
When the gingival tissue is not healthy, it can provide a gateway for periodontal disease to advance into the deeper tissue of the periodontium, leading to a poorer prognosis for long-term retention of the teeth. Thus, both the type of periodontal therapy and homecare instructions given to patients by dental professionals and restorative care are based on the clinical conditions of the tissue.
Anatomy of Gingival Tissue
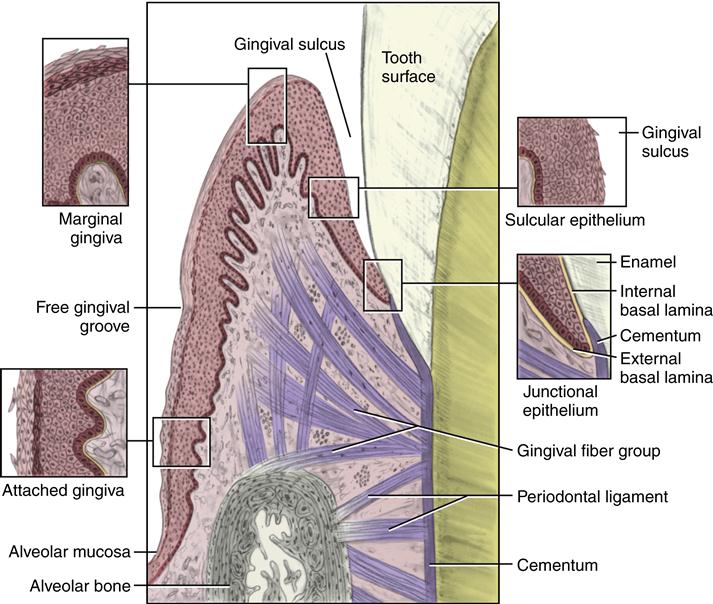
Surrounding the maxillary and mandibular teeth in the alveoli and covering the alveolar processes is gingival tissue (Figure 10-1). When looking at the gingival tissue in a clinical setting, different types are noted in the oral cavity. The gingival tissue that tightly adheres to the bone around the roots of the teeth is the attached gingiva. The gingival tissue between adjacent teeth is an extension of attached gingiva and is the interdental gingiva, forming the interdental papillae.
The attached gingiva is a masticatory mucosa (see Chapter 9). Healthy attached gingiva is pink in color, with some areas of melanin pigmentation possible (see Figures 2-10 and 9-22). The tissue when dried is dull, firm, and immobile, with varying amounts of stippling. The width of the attached gingiva varies according to its location. However, certain levels of attached gingiva may be necessary for the stability of the underlying root of the tooth.
The interdental papillae fill in the area between the teeth apical to their contact areas to prevent food impaction. The interdental papillae assume a conical shape for the anterior teeth and a blunted shape buccolingually for the posterior teeth.
At the gingival margin of each tooth is the free gingiva, or marginal gingiva, which is continuous with the attached gingiva. The gingival tissue that faces the tooth, the dentogingival junctional tissue, is discussed later.
Both the attached gingiva and the marginal gingiva are easily seen in the oral cavity, whether the gingival tissue is healthy or not. The gingival margin, or free gingival crest, at the most superficial part of the marginal gingiva, is also easily seen clinically, and its location should be recorded on a patient’s chart.
A free gingival groove separates the attached gingiva from the marginal gingiva. This slight depression on the outer surface of the gingiva does not correspond to the depth of the gingival sulcus but instead to the apical border of the junctional epithelium. This outer groove varies in depth according to the area of the oral cavity; the groove is very prominent on mandibular anteriors and premolars.
The marginal gingiva varies in width from 0.5 to 2.0 mm from the free gingival crest to the attached gingiva. The marginal gingiva follows the scalloped pattern established by the contour of the cementoenamel junction (CEJ) of the teeth. The marginal gingiva has a more translucent appearance than the attached gingiva, yet has a similar clinical appearance, including pinkness, dullness, and firmness. In contrast, the marginal gingiva lacks the presence of stippling, and the tissue is mobile or free from the underlying tooth surface, as can be demonstrated with a periodontal probe.
Apical to the contact area, the interdental gingiva assumes a nonvisible concave shape between the facial and lingual gingival surfaces forming the gingival col. The col varies in depth and width, depending on the expanse of the contacting tooth surfaces. The epithelium covering the col consists of the marginal gingiva of the adjacent teeth, except that it is nonkeratinized. It is mainly present in the broad interdental gingiva of the posterior teeth, and generally is not present with those interproximal tissue associated with anterior teeth because the latter tissue is narrower. In the absence of contact between adjacent teeth, the attached gingiva extends uninterrupted from the facial to the lingual aspect. The col may be important in the formation of periodontal disease but is visible clinically only when teeth are extracted.
Histology of Gingival Tissue
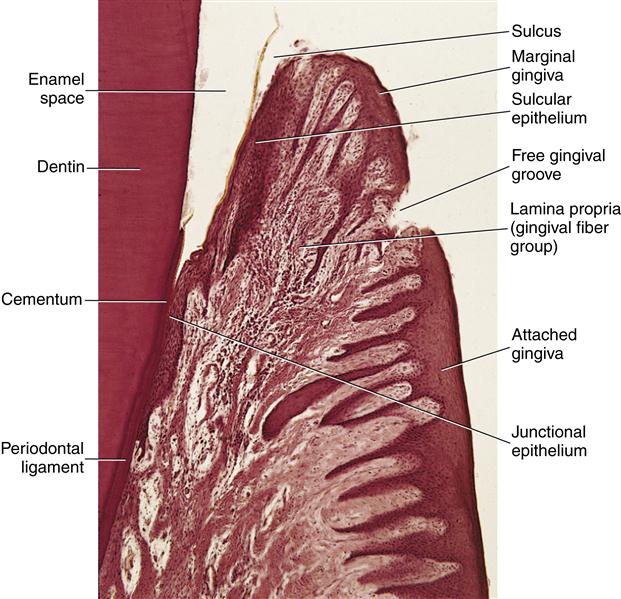
The attached gingiva and the marginal gingiva have some similar histology, yet each has features specific to the tissue (Figure 10-2). The attached gingiva has a thick layer of mainly parakeratinized stratified squamous epithelium, which obscures its extensive vascular supply in the lamina propria, making the tissue pinkish (see Figure 9-11). The lamina propria also has tall, narrow connective tissue papillae and rete ridges, giving the tissue its varying amounts of stippling. Thus, the interface between the epithelium and lamina propria is highly interdigitated. The lamina propria is directly attached to the underlying jaws, making the attached gingiva firm and immobile, and thus serves as a mucoperiosteum.
Similar to the attached gingiva, the marginal gingiva is a masticatory mucosa but mainly has a surface layer of orthokeratinized stratified squamous epithelium. The associated lamina propria also has tall, narrow papillae, but this lamina propria is continuous with the lamina propria of the gingival tissue that faces the tooth. Unlike the attached gingiva, the marginal gingiva is not attached to the underlying jaws, making this tissue firm but mobile.
Note that the gingival fiber group is found in the lamina propria of the marginal gingiva (see Figure 14-32). Some histologists consider the gingival fiber group part of the periodontal ligament, but this fiber group supports only the gingival tissue and not the tooth in relationship to the jaws. The lamina propria of the marginal gingiva is also continuous with the adjacent connective tissue, which includes the lamina propria of the attached gingiva, as well as the periodontal ligament.
Dentogingival Junctional Tissue
The dentogingival junction is the junction between the tooth surface and the gingival tissue. Together, the sulcular epithelium and junctional epithelium form the dentogingival junctional tissue. Both the sulcular epithelium and junctional epithelium are difficult to see in clinical examination of healthy gingival tissue.
The crevicular epithelium, or sulcular epithelium, stands away from the tooth, creating a gingival sulcus, or space that is filled with gingival crevicular fluid (GCF) (see Figure 10-1). The depth of the healthy gingival sulcus varies from 0.5 to 3 mm, with an average of 1.8 mm. A normal GCF flow rate is quite slow and has been calculated at 1 to 2 microliters per tooth per hour. Thus, the amount of GCF is minimal in the healthy state.
The GCF seeps between the epithelial cells and into the gingival sulcus. It allows the components of the blood to reach the tooth surface through the junctional epithelium from the blood vessels of the adjacent lamina propria. The GCF contains both the immunological components and cells of the blood, although in lower amounts and in different proportions. It also contains sticky plasma proteins in the sulcus that serve as adhesive for its lining tissue, keeping it intact.
The GCF also includes white blood cells (WBCs), especially the polymorphonuclear leukocytes (PMNs), as well as the immunoglobulins of IgG, IgM, and serum IgA from plasma cells, which all have a role in the specific defense mechanism against disease. Thus, any immunological reactions in the blood are directly relevant to those found in the GCF and />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses