The edentulous maxillae have a unique anatomic presentation, which limits the number and the distribution of implants within the alveolar ridge. The maxillary sinuses bilaterally and the position of the nasal floor in the premaxillary region may limit the vertical volume of alveolar bone available for placement of implants in the maxilla for a fixed, implant-supported prosthesis. The palatal and posterior resorption pattern of the edentulous maxillae may also limit the horizontal bony volume necessary to house endosseous implants. Therefore, in review of the literature, the recommended treatment for the edentulous maxilla has been the tissue-supported, overdenture appliance. To establish support for a fixed prosthesis, reconstruction of the maxilla with various bone grafting techniques has been designed to recreate the alveolar volume and topography needed for stabilization of dental implants. If the sinuses are pneumatized, sinus grafting or tilted implants have also been recommended.
For patients with significant anterior extension of their maxillary sinuses, extending forward into the bicuspid region, the zygomatic implant is recommended. The zygomatic implant allows for establishing posterior maxillary support by using the limited crestal alveolar bone in the bicuspid region and the os zygomaticum for establishing initial stability of the implant. The use of the zygomatic implant and its success rate have been studied internationally, with a success rate between 94% and 100% as reported by the authors.
The 94% survival, as reported by Branemark et al., represents three failures out of 52 zygoma fixtures placed in their initial study. The first failure was due to enveloping of muscle tissue around the zygoma fixture. The second involved the inadequate centering of the implant within the zygomatic bone. The third failure occurred in a patient with Paget’s disease who had loosely textured and low density bone. Overall, this highly predictable implant allows establishing posterior maxillary support for reconstruction with a fixed prosthesis without the need for bone grafting.
▪
HISTORICAL PERSPECTIVE
The treatment of the moderately to severely resorbed maxillae presents a challenge for the implant surgical-restorative team. The typically large pneumatized sinuses in this group of patients require extensive bone grafting if conventional implant placement is envisioned. Various procedures have been available for treatment of the resorbed maxillae. Adell, Breine, and Branemark used composite grafts to provide a tooth anchorage system. Le Fort I osteotomy and iliac block graft have also been used to reestablish bony volume for placement of implants. To create bone mass in the posterior maxillae, sinus-lift grafting procedures have been performed. Survival of implants in sinus-lift procedures was studied in the sinus consensus conference. The conclusion reached was similar to Tolman’s report in 1995: The material was so “multivariate and multifactorial that it was difficult to draw definitive conclusions; these must await controlled prospective studies.” Grafting of the maxillae with delayed implant placement has been described in the literature. Rasmusson presented success with autogenous grafting to establish favorable topography of the resorbed maxillae for implant placement using inlay, onlay, and/or Le Fort I procedures. A success rate of 80% was reported for grafting with delayed implant placement and 77% for grafting with simultaneous implant placement. The success rate of implants placed in nongrafted bone was only 89% in the group studied. Keller and Tolman, who used inlay grafts in their report on the reconstruction of the compromised maxillae, reported an 87% implant survival rate and a prosthetic survival of 95%. The somewhat limited success with these adjunctive procedures has deterred patients from seeking reconstruction of their resorbed maxillae. An alternative for the treatment of this group of patients is the zygomatic implant, which was introduced by Professor Branemark in 1988.
▪
PATIENT SELECTION
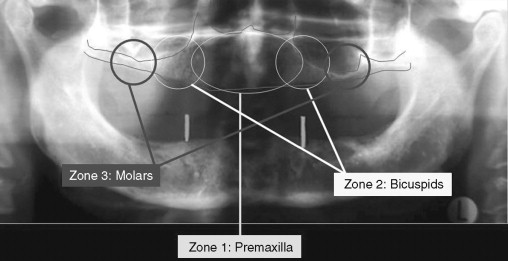
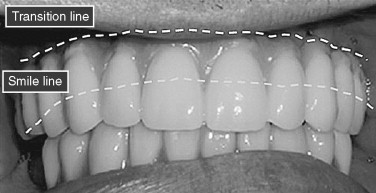
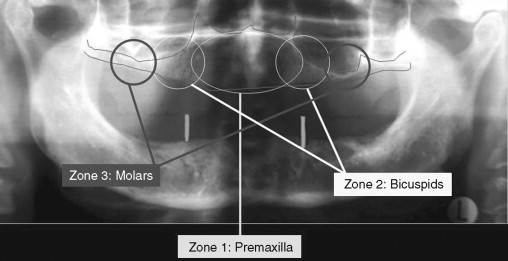
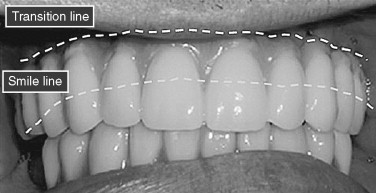
A systematic preoperative evaluation of the patient is required before the surgical treatment. Both surgical and prosthetic needs must be considered before initiation of the surgical treatment to allow for a predictable outcome. The preoperative evaluation protocol takes into consideration the available alveolar bone in the different zones of the maxilla ( Figure 29-1 ). It also determines whether the final prosthesis is a ceramometal bridge or profile prosthesis. The determination is based on the lack or the presence of composite defect. Evaluation of the aesthetics of the final prosthesis is made by recognizing the transition line between the prosthesis and the residual edentulous crestal soft tissues ( Figure 29-2 ). The zygomatic implant is considered in the group of patients who demonstrate bone in zone 1 only. In patients who also have limited horizontal alveolar width in zone 1, veneer grafting before placement of the conventional implants for the anterior support is considered. A separate group of patients with advanced maxillary alveolar atrophy present with complete lack of the alveolus. This group may be candidates for the quad zygoma treatment concept ( Figure 29-3 ). The surgical procedure may be performed in the hospital setting using general anesthesia or in the office under IV sedation and local anesthesia. The surgical candidate should be free of any sinus disease before consideration for this treatment concept.

▪
PATIENT SELECTION
A systematic preoperative evaluation of the patient is required before the surgical treatment. Both surgical and prosthetic needs must be considered before initiation of the surgical treatment to allow for a predictable outcome. The preoperative evaluation protocol takes into consideration the available alveolar bone in the different zones of the maxilla ( Figure 29-1 ). It also determines whether the final prosthesis is a ceramometal bridge or profile prosthesis. The determination is based on the lack or the presence of composite defect. Evaluation of the aesthetics of the final prosthesis is made by recognizing the transition line between the prosthesis and the residual edentulous crestal soft tissues ( Figure 29-2 ). The zygomatic implant is considered in the group of patients who demonstrate bone in zone 1 only. In patients who also have limited horizontal alveolar width in zone 1, veneer grafting before placement of the conventional implants for the anterior support is considered. A separate group of patients with advanced maxillary alveolar atrophy present with complete lack of the alveolus. This group may be candidates for the quad zygoma treatment concept ( Figure 29-3 ). The surgical procedure may be performed in the hospital setting using general anesthesia or in the office under IV sedation and local anesthesia. The surgical candidate should be free of any sinus disease before consideration for this treatment concept.

▪
RADIOGRAPHIC EVALUATION
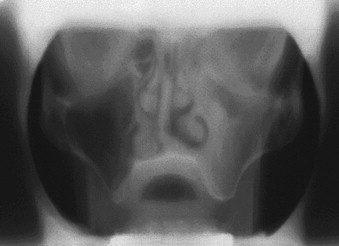
Although computerized and conventional tomography can be used, the Panorex radiograph is critical in the initial evaluation of the patient. The presence of alveolar bone in the premaxilla (zone 1) and the lack of bone in the bicuspid and the molar regions, zones 2 and 3 respectively, are the indications for considering the zygomatic concept. Axial CT scans can be obtained to further evaluate the maxillary sinus. The width of the residual alveolar bone and the width and height of the zygomatic body can be visualized in frontal reformatted sections of the axial CT scans.
Further evaluation of the zygomatic bone has also been described. Although not absolutely necessary, the reformatted frontal images in 2 to 3 mm cuts afford the less experienced operator more information for planning the surgery ( Figure 29-4 ). The presence of sinus pathologic conditions, including, but not limited to, thickening of the schneiderian membrane and air fluid levels, may be ruled out in both the Panorex and tomographic studies.
▪
OS-ZYGOMATICUM: REGIONAL ANATOMY
The quantity and the quality of the zygomatic bone have been studied and reported by Nkenke et al. The morphology and the microstructure of the os zygomaticum were assessed by quantitative computer tomography and histomorphometry. Bone mineral density of 30 human zygomatic bone specimens was studied. The trabecular bone mineral density, the trabecular bone volume, and the trabecular bone pattern factor were correlated with each other. The conclusion reached suggested that the trabecular bone of the os zygomaticum was not a favorable site for implant placement. However, Nkenke further suggests that the success seen with the zygomatic implant is due to the engagement of four cortices during the placement of the implant. The lingual cortex of the maxillary alveolus along with the cortical floor of the maxillary sinus provide for bicortical stabilization at the crestal portion of the implant. The superior-lateral portion of the roof of the maxillary sinus is formed by the inferior portion of the zygomatic bone. This portion of the zygoma along with its lateral superior cortical covering form the bicortical stabilization at the apical portion of the zygomatic implant.
To quantify the dimensions of cortical and trabecular bone of the os zygomaticum, morphometric analysis of the zygomatic bone was consistent with the following results: mediolateral dimension of 7.6 mm in males and 8.0 mm in females. The anterior-posterior dimension of the zygoma body was 25.4 mm in males and 24.9 mm in females. The lateral cortical thickness was 1.75 mm in males and 1.71 mm in females. The length of the zygomatic implant within the zygomatic bone was 16.5 mm in males and 14 mm in females. Zygomatic implants placed following ablative surgery have been reported by Weingart et al. The implant survival rate was 65% to 75%. However, with the increased popularity of the zygomatic implant used in the atrophic maxilla, implant survival has increased to 97% to 100%.
▪
PREOPERATIVE CONSIDERATIONS
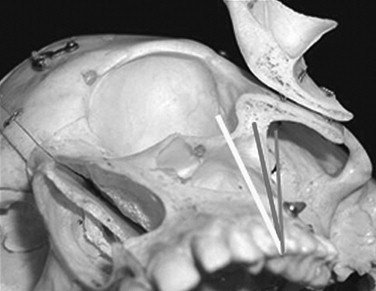
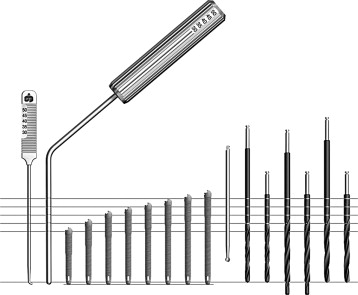
The surgical procedure is usually performed in the office setting under IV sedation. All patients are premedicated 1 hour before the surgical procedure. The proper administration of sufficient local anesthesia is critical in the management of these patients under IV sedation. The various infiltrations and nerve blocks include circumvestibular infiltration of the maxilla, greater palatine blocks, and bilateral transcutaneous infiltration of the temporal areas over the zygomatic body. Bilateral inferior alveolar nerve blocks are considered to allow retraction of the lower jaw during the surgery without undo stimulation of the sedated patient. It is recommended that direct visualization of the path of the implant from the premolar area to the base of the zygoma be visualized whenever possible. Direct visualization of the base of the zygomatic body has also been advocated in clinicians who have used computer-assisted treatment planning and surgical templates for placement of the zygomatic implant. Having a clear view of the path of the instruments needed in establishing the osteotomy and visualizing the path of the implant during its insertion prevent disorientation and potential complications associated with placement of the zygomatic implant. Generally, three potential axes of insertion are possible. The proper axis is a path extending from the bicuspid region through the maxillary sinus, entering the midportion of the zygomatic body. If the entry point in the zygomatic body is more anterior to this line axis, potential for penetration into the orbit exists. However, if the line axis is posterior to this line, the potential for entering the pterygomaxillary space, leading to soft tissue enveloping and the subsequent lack of osseointegration of the implant among the potential for unexpected hemorrhage, exists ( Figure 29-5 ). The zygomatic implant has a unique design. The diameter of the apical two thirds of the implant is 4.0 mm, yet the alveolar one third widens to a diameter of 5.0 mm. The zygomatic implants are available in lengths ranging from 30 to 52.5 mm. A specialized series of long zygoma drills are used to prepare the osteotomy ( Figure 29-6 ).
▪
SURGICAL OPTIONS
In reconstruction of the edentulous maxilla with the zygomatic implant, the traditional two-stage protocol or the immediate-load protocol may be considered. The two-stage protocol requires the immediate cross arch splinting of the zygoma implants at the time of the uncovering procedure. This can be accomplished efficiently by using the Cal technique ( Figure 29-7 ) for the fabrication of a passive bar before the uncovering procedure. However, the alternative immediate-load technique cross arch splints the zygomatic implant with each other by conversion of the patient’s existing denture into a fixed provisional bridge. The immediate loading of the zygomatic implants has been reported in the literature with favorable results.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


