Biology of Wound Repair
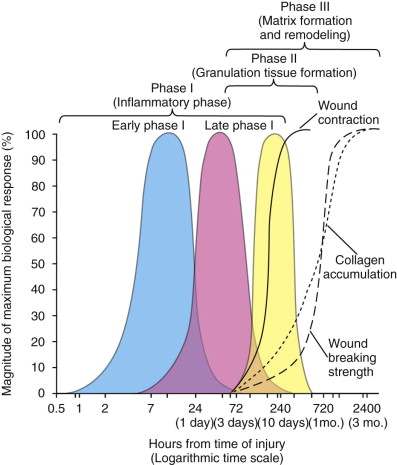
Wound healing is a complex cascade of highly integrated cellular and molecular events that drive the process of tissue restoration, which consists of several distinct but overlapping phases. These stages include hemostasis and inflammation, proliferation, and remodeling ( Fig. 2-1 ). Impaired healing in acute and chronic wounds generally occurs when there is a failure to progress through the normal stages of wound repair. Although rates and patterns of healing depend on the local, systemic, and surgical factors of the host, the phases of oral mucosal healing closely approximate those of cutaneous healing. In general, wounds in the oral cavity appear to heal faster than dermal wounds, and they have minimal or no scar formation.
Hemostasis and Inflammatory Phase
Severe tissue injury disrupts blood vessels and causes extravasations of blood constituents. Blood coagulation and platelet aggregation generate a fibrin clot within the vessel lumen and provide a provisional matrix for cell migration. Several pro-coagulant factors including fibrinogen, fibronectin, and thrombospondin are secreted by the injured cells and initiate the coagulation cascade. The clot and surrounding wound tissues release pro-inflammatory cytokines and growth factors, including platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), epidermal growth factor (EGF), and transforming growth factor-β (TGF-β). Once bleeding is controlled, inflammatory cells migrate into the wound (chemotaxis) and begin to remove apoptotic cells and bacteria from the injured area. Clinical signs include localized edema (swelling), pain (dolor), redness (rubor), and increased warmth (calor) at the wound site. Neutrophils are the predominant inflammatory cells during the early inflammatory phase, but they are rapidly outnumbered by macrophages, derived from mobilized monocytes, and T lymphocytes during the transition to the proliferative phase.
Proliferation Phase
The proliferation phase is characterized by epithelial proliferation and migration over the provisional matrix. In the reparative dermal tissue, fibroblasts and endothelial cells proliferate and contribute to capillary growth, collagen synthesis, and granulation tissue formation. Fibroblasts are the major cells responsible for the production of collagen, glycoaminoglycans, and proteoglycans, which are major components of the extracellular matrix. Concurrent with these events is the process of angiogenesis, whereby new blood vessels are formed and lymphatics are recanalized in the healing tissues. This essential process reestablishes proper transport of nutrients and oxygen to the local injured sites. Epithelial cells originating from the bulge of hair follicles, sebaceous glands, and the basal layer of the epidermal margins of the wound edges proliferate and resurface the wound. In contrast to skin, the process of reepithelialization progresses more rapidly in an oral mucosal wound. The oral epithelial cells migrate directly onto the moist, exposed surface of the fibrin clot instead of under the dry exudate (scab) of a dermal wound.
Maturation and Remodeling Phase
The remodeling phase is the final stage of tissue repair and is distinguished by a continual turnover of collagen fibers. The tensile strength of the wound is gradually restored as the collagen fibers are realigned and increasingly cross-linked in a well-organized pattern. The maximal tensile strength of a healed wound is reached in 6 to 12 months post-injury, depending on host factors, but it never reaches the initial strength of unwounded tissue. Eventually, active collagen synthesis achieves equilibrium with collagenolysis. The homeostasis can be delayed by disruptive processes such as poor oxygen perfusion, lack of nutrients, and wound infection, which favor collagen breakdown and wound dehiscence.
Principles of Wound Care
From a surgical viewpoint the nature of the healing process is determined by several factors, including the nature of the injury, the anatomic site, the type of tissue, the timing of the repair, and orientation of the wound margins. Early primary closure with adequate apposition of the wound margins usually results in healing by primary or first intention, with minimal scar formation. In the presence of wound infection, severe tissue loss, or poor apposition of the wound margins, the healing process is prolonged, with excess granulation and connective tissue formation, also known as healing by second intention. In infected wounds with purulent drainage or in contaminated traumatic wounds, the surgeon may attempt healing by third intention, whereby the wounds are allowed to initially granulate and heal by second intention, followed by delayed primary closure.
Wound Closure
Wound closure is particularly important in the head and neck region, where the treatment goals are a mechanically sound wound closure and a cosmetically acceptable scar. Most simple wounds, generated by surgical incisions or clean lacerations, heal rapidly by primary intention. Complex wounds, such as burns, avulsions, and infected or contaminated injuries, usually heal more slowly by secondary intention, and may require skin grafts or flaps. Current wound management focuses on eliminating causative factors, providing systemic support to enhance tissue repair, and maintaining a physiologic local wound environment amenable to optimal healing. All wounds should be as clean as possible, and debrided of non-viable tissues or foreign bodies. Ragged wound margins must be revised and undermined to achieve a tension-free closure as appropriate. Depending on the nature of the wound, sutures, suction drains, or pressure dressings may be applied.
Proper suture technique should incorporate three major principles including proper distribution of tension to the deeper layers, atraumatic handling of tissues, and eversion of wound margins. Where appropriate, closure of the cutaneous wound should be layered. Deep sutures are usually placed in strong, fibrous tissue, such as fascia or dermis, rather than muscle or fat. Wound tensile strength depends on suture integrity in the first few weeks until strong collagen fiber is formed. Hence polyglycolic acid (PGA) sutures are suitable for this purpose. Non-resorbable sutures may be indicated to close wounds under tension. Closure of the dermal (subcutaneous) layer is fundamental for esthetic wound closure. Dermal sutures should be inverted to avoid extrusion of the knots. If the deeper portion of the suture is wider than the portion that crosses the surface, there will be some eversion of the wound margins. Mucosa can be closed with either permanent or resorbable sutures. Skin can be closed with permanent sutures or staples. Depending on the individual wound, simple sutures, horizontal or vertical mattress sutures, half-buried mattress sutures, or running sutures can be used.
Partial Thickness Wounds
Partial thickness injuries are caused by abrasions or the harvest of skin or mucosal grafts. Such injuries heal primarily by reepithelialization. In the moist environment of the mucosa, similar wounds form a fibrinous pseudomembrane. Dressings may aid in wound epithelialization; increase patient comfort and compliance; and decrease the risk of infection and overall healing time. Gauze dressings impregnated with various antibacterial compounds and occlusive dressing films are often used for this purpose. Wet-to-dry dressings are effective in debriding partial thickness wounds that have become infected. Systemic antibiotics do not work well in this situation and should be used only if there is cellulitis in the surrounding tissues.
Full Thickness Wounds
Full thickness injuries imply a complete loss of the epithelial layer and its appendages leading to the exposure of the subcutaneous (submucosal) tissues. Full thickness wounds can be caused by tumor excision, trauma, burns, infection, radiation, or vascular compromise. These wounds will heal gradually by granulation and epithelialization. The healing process is slow and can be uncomfortable, with high risk of infection until the protective epithelium is fully restored. Healing of the full thickness wounds can be enhanced by grafting the wound bed with an epithelial layer. If the wound bed is clean and well vascularized, a full or partial thickness skin graft can be placed. Depending on the location, a vascularized flap may also be a better choice. Frequent dressing changes and topical antibacterial agents are useful in reducing the risk of infection.
Use of Skin Substitutes
Immediate wound coverage is critical for the acceleration of wound healing and prevention of infection. When the surface area is relatively large, the wound can be covered by synthetic and natural dressings aside from the native skin grafts. The commercially available human skin substitutes are grouped into three major types and serve as excellent alternatives to autografts. The first type consists of grafts of cultured epidermal cells with no dermal components (Epicel, Genzyme Biosurgery, Cambridge, Mass.). The second type has only dermal components (AlloDerm, LifeCell Corp., Woodlands, Texas; Dermagraft, Advanced Biohealing, Inc., La Jolla, Calif.). The third type consists of a bilayer of both dermal and epidermal elements (Apligraf, Organogenesis Inc., Canton, Mass.; Integra; Johnson & Johnson Medical LifeSciences Corp., Plainsboro, NJ). The chief effect of most skin substitutes is to promote wound healing by stimulating the recipient host to produce a variety of wound-healing cytokines and chemokines. The use of cultured skin to cover wounds is particularly attractive, inasmuch as the living cells already can produce the necessary level of growth factors at the appropriate time.
Principles of Scar Treatment
Revision of excessive scars resulting from aberrant wound healing is among the most challenging endeavors for the surgeon, particularly in the head and neck region where cosmesis is paramount. There is no single treatment option that stands alone as the best practice model. As a result, a combination of approaches is the best remedy for this challenging problem.
Scar Analysis and Timing of Scar Revision
In scar revision, the opportune time for the best outcomes may be lost at the initial wound repair if the assessment and surgical technique are shoddily performed. Therefore attention to the details of primary repair is the key to minimizing unsightly scar formation. Initial management requires a full analysis of location, color, height, thickness, and direction of the scar. In general, the more conspicuous the scar, the greater the challenge the surgeon faces to improve its esthetics. This weighs heavily on the analysis and planning at the beginning of wound management.
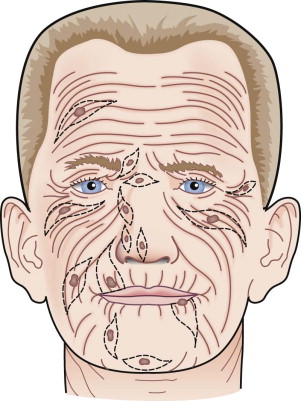
The morphology of scars varies among a wide variation of colors, sizes, and shapes. They may be raised, flattened, wide, or narrow, with straight or corrugated borders. Altered sensation such as pruritus, numbness, and even frank pain may accompany scar formation. The location of the scar should be carefully documented with an assessment of the adjoining structures or units of face or neck that may be influenced by its repair. Color matches should be considered if nearby tissues will be used to facilitate repair. The full three-dimensional configuration of the scar should be documented in units of measure such as millimeters. Also important are the directional tendencies and vector forces influencing the scar, especially with respect to the relaxed skin tension lines of the face and neck ( Fig. 2-2 ).
The timing of scar revision is influenced by a variety of factors. These include the type and location of injury and psychological state of the patient, including his or her realistic expectations of the potential outcomes of revision surgery. Depending on the treatment techniques employed, the timing of revision may vary. In general, scar revision should not be performed until the scar is considered mature. This usually is in the range of 6 to 12 months, though some techniques such as dermabrasion may be performed earlier.
Treatment and Reconstructive Goals
The reconstructive goal in most situations would be to create a scar that more closely resembles the surrounding tissues, rather than to remove the scar, which may be unrealistic. Other specific reconstructive goals include creating a scar that (1) is flat and level with the surrounding skin, (2) has an appropriate color match, (3) is narrow, (4) is parallel to the favorable skin lines, and (5) avoids straight and unbroken lines. Attention to the details of wound management in its primary repair phase is critical for preventing excessive scarring. The surgeon should remain steadfast to current accepted treatment and reconstructive goals and their realistic expectations of the potential outcomes of revision surgery. An analysis of the scar’s psychological impact on the patient and his or her expectation of the outcome of revision is also of utmost importance. Furthermore, the patient should be aware that several secondary procedures may be necessary to achieve optimal results.
Specific Treatment and Techniques
A variety of scar modifying techniques may be selected based on the scar analysis, treatment timing, and reconstructive goals. These techniques can be subdivided into three broad categories: excisional, irregularization, and epithelial abrasion techniques. Multiple techniques combined with appropriate staging usually offer the best outcomes. The patient must be informed that scars cannot be removed, but their unsightly nature can be modified to become more acceptable esthetically and functionally through adroit scar analysis and meticulous techniques.
Excisional Techniques
Fusiform Excision
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


