Successful intervention in a developing Class III malocclusion with facemask protraction therapy depends on a patient’s ability to adhere to the recommendations for duration of appliance wear. In this article, we report the introduction of a novel approach for tracking of the duration of application of a protraction facemask, with the incorporation of a “FaceMon” sensor (TheraMon, microelectronic system; MC Technology GmbH, Hargelsberg, Austria) to track wear time. A 9-year-old boy with a Class III malocclusion was successfully treated with a modified alternate rapid maxillary expansion and constriction protocol and intermittent application of a hybrid hyrax-protraction facemask combination. The average duration of wear of the facemask was measured at 10.8 hours per day. The use of an objective measuring device may have implications for the development of treatment strategies, since patient responses may be able to calibrated in relation to compliance.
Highlights
- •
Compliance is an important element in achieving successful treatment outcomes.
- •
Microelectronic recording devices can provide data on compliance.
- •
A TheraMon sensor was integrated into a facemask worn by a 9-year-old boy.
- •
Use of a sensor allows the treatment to be calibrated to the compliance.
Compliance in orthodontics refers to how reliably a patient adheres to the prescribed instructions of the orthodontist and is an important key to achieving a successful treatment outcome. Compliance is influenced by many factors including the personality of the patient, the comfort of wear of an appliance, and parental support.
The literature is replete with studies that have evaluated the effectiveness of interceptive Class III orthodontic treatment in adolescent patients. However, no study has evaluated the patient’s compliance objectively. The current literature shows that one cannot rely on subjective assessments of compliance; ie, patient reports or questionnaires. Objective compliance measurement using a sensor (TheraMon, microelectronic system; MC Technology GmbH, Hargelsberg, Austria) has only been described for intraoral appliances. The conventional approach to addressing a Class III malocclusion with maxillary retrognathia in an adolescent patient is with a protraction facemask in conjunction with a rapid maxillary expansion appliance. The corollary of this approach is an inevitable mesial migration of the dentition, resulting in the development of anterior crowding and increasing the possible need for subsequent extraction therapy.
The mesial migration of the molars, or loss of anchorage, can be mitigated using different kinds of additional anchorage protocols, such as intentionally ankylosed teeth, dental implants, or miniplates. Another advantage of these approaches is that orthopedic forces may be directly transferred to the nasomaxillary complex.
Wilmes et al and Ludwig et al introduced a hybrid hyrax appliance to minimize anchorage loss, involving a minimally surgically invasive procedure. Two mini-implants are inserted in the paramedian area of the anterior palate, serving to support the anchorage in the sagittal and transverse dimension. The maxillary molars can be stabilized in their position while orthopedically displacing the maxilla anteriorly. In the transverse plane, the mini-implants reduce the forces acting on the dentition during maxillary expansion, thereby possibly leading to less buccal tipping, root damage, and gingival dehiscence.
Protraction facemask therapy is often combined with orthopedic expansion of the maxilla. To increase the stimulatory effect of the midface sutures, Liou et al described a method of alternating expansion and constriction. In this protocol, protraction of the maxilla starts after 7 to 8 weeks of alternating expansion and constriction of 1 mm each day.
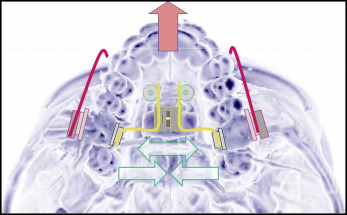
We modified the protocol in the way that we started maxillary protraction simultaneously with the alternating expansions and constrictions ( Fig 1 ).
For Class III correction, 2 intraoral elastics with a force of 400 g per side were applied, as measured with a Dynamometer (Correx, Köniz, Switzerland).
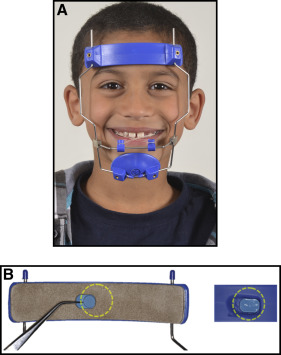
The recommended time duration for wear of the facemask varies with differing early Class III treatment protocols, ranging from 14 hours per day to full-time wear. However, none of these studies has reported the effective duration of wear time in subjects but rather has relied on self-reporting from patients and parents. In this case report, we used the TheraMon chip (TheraMon microelectronic system; MC Technology GmbH) integrated into a facemask to objectively document the compliance of our patient ( Fig 2 ). Schott et al showed that wear-time documentation is well accepted by patients and parents.
Diagnosis and etiology
A 9-year-old boy was referred to the Department of Orthodontics of the University of Düsseldorf in Germany by his general dental practitioner for treatment of his anterior crossbite. The extraoral examination showed a concave facial profile and a retrusive midface ( Fig 3 ).

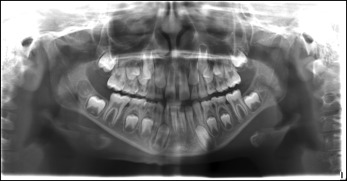
The intraoral examination showed an Angle Class III malocclusion characterized by molar and canine relations of a half unit mesial occlusion bilaterally. Overjet was −2.6 mm, and overbite was −0.5 mm. The patient had both anterior and posterior crossbites. Transverse measurements of the dental arch showed no discrepancy between the maxillary and mandibular arches. Thus, the posterior crossbite was due to the sagittal skeletal discrepancy. The dental midline was coincident with the facial midline. A maxillary midline diastema was present with retained deciduous lateral incisors. A retained hypoplastic deciduous lateral incisor was present in the mandibular arch. The panoramic radiograph showed agenesis of the mandibular right lateral incisor, developing mandibular third molars, an ectopically positioned mandibular right canine, pipette-like roots, and deep antegonial notching of the mandible ( Fig 4 ). The pretreatment lateral cephalometric analysis showed a distinct skeletal Class III malocclusion (Wits appraisal, −5.5 mm; ANB, −1.4°) with a retrognathic maxilla (SNA, 73.0°) and a slightly retrognathic mandible (SNB, 74.4°) with a vertical facial structure (ML/NL, 32.4°).
The functional analysis showed an anterior mandibular shift of 1 mm caused by premature interference of the mandibular deciduous canines. Additionally, the patient demonstrated an anterior tongue thrust habit.
Treatment objectives
The specific treatment objectives included (1) early treatment with maxillary protraction using the modified Alt-RAMEC protocol to correct the skeletal maxillary deficiency ( Fig 1 ), (2) correction of the anterior crossbite and elimination of the functional mandibular shift, (3) overcorrection into a dental Class II relationship and subsequent distalization of the maxillary first molars into a Class I occlusion, and (4) elimination of the tongue thrust habit.
The treatment plan did not yet include space management of the aplastic mandibular right lateral incisor.
Treatment objectives
The specific treatment objectives included (1) early treatment with maxillary protraction using the modified Alt-RAMEC protocol to correct the skeletal maxillary deficiency ( Fig 1 ), (2) correction of the anterior crossbite and elimination of the functional mandibular shift, (3) overcorrection into a dental Class II relationship and subsequent distalization of the maxillary first molars into a Class I occlusion, and (4) elimination of the tongue thrust habit.
The treatment plan did not yet include space management of the aplastic mandibular right lateral incisor.
Treatment alternatives
Orthopedic protraction of the maxilla can be achieved using either an extraoral appliance such as a protraction facemask or intraoral skeletal anchorage such as Bollard plates or a Mentoplate. The relative merits, shortcomings, and risks of each treatment modality were clearly explained to the patient and his parents. They made an informed decision to proceed with treatment using the protraction facemask, secondary to their underlying concerns about the associated surgical risks.
Other possible treatment alternatives included a functional appliance such as the Fränkel III, which is considered less invasive but perhaps also less effective in correcting a retrognathic maxilla, since its treatment effects are mainly dentoalveolar and due to downward and backward rotation of the mandible.
The degree of compliance could be assessed with self-reporting mechanisms: eg, patient and parent questionnaires rather than a microelectronic device. However, this approach is susceptible to recall bias, and compliance cannot be judged objectively.
Treatment protocol
Topical and local anesthesias were applied. Two mini-implants with exchangeable abutments (2 × 9 mm, Benefit System; PSM Medical Solutions, Tuttlingen, Germany) were inserted with a contra-angle screwdriver next to the midpalatal suture and adjacent to the third palatal rugae. Because of the low mineralization of the bones in young patients, predrilling was not necessary. Impression caps were fitted onto the implants, and a silicone impression was taken. Bands were not fitted to the molars because the hybrid hyrax distalizer, including the buccal extension arms, was cast in 1 piece. The appliance comprised a split palatal screw (hyrax; Dentaurum, Ispringen, Germany) with a thread pitch of 0.2 mm.
The appliance was placed 1 week later, with the appliance bonded with Fuji ORTHO BAND (GC Corporation, Tokyo, Japan). This patient was treated with the modified Alt-RAMEC protocol comprising 15 weeks of alternating expansions and constrictions of 1 mm per day for 7 days, and concomitant protraction of the maxilla by wearing the facemask ( Figs 1 and 2 , A ). The magnitude of force applied was 400 g per side with the 5/16-in, 16-oz elastics. The hybrid hyrax distalizer facilitates both orthopedic advancement of the maxilla and a simultaneous orthodontic distalization of the maxillary molars ( Fig 5 , A and B ). The elastics were attached from the hooks of the hybrid hyrax distalizer ( Fig 5 ) to the support bar of the facemask in a downward and forward direction of 30° relative to the occlusal plane to reduce the anterior rotation of the maxilla.




