Vertical dimension control with fixed appliance mechanotherapy has always been a matter of concern in moderate to severe high-angle patients with severe proclination of the anterior teeth. Extrusion of the posterior teeth is an inevitable sequela of conventional mechanics in such patients, especially if they are adults. This article reports on 3 patients who were treated with mini-implants (diameter, 1.3 mm; length, 8 mm) placed between the roots of the second premolar and the first molar for en-masse retraction of the anterior teeth. The biomechanical force system that developed not only maintained absolute anchorage, but also provided effective control over the posterior dentoalveolar dimension so that dramatic improvement in facial esthetics could be achieved. Small but significant autorotation of the mandible was noted; this led to increased chin prominence in all 3 patients. With accurate diagnosis and treatment planning, mini-implant anchorage can be a possible alternative to orthognathic surgery in similar borderline patients.
Bialveolar dental protrusion is common in many ethnic groups. It is characterized by dentoalveolar flaring of the anterior teeth with resultant protrusion of the lips and convexity of the face. The treatment for bialveolar protrusion often involves extraction of the 4 first premolars, followed by anterior teeth retraction under maximum anchorage. However, malocclusions with severely proclined anterior teeth and a hyperdivergent facial pattern are often difficult to correct. This has been classically described as the long-face syndrome, characterized by a tendency toward a backward rotational growth pattern resulting in a relatively long lower facial height and a steep mandibular plane angle.
According to Klontz, if posttreatment facial balance must be obtained in average- to high-angle patients, these 3 treatment objectives should be achieved during orthodontic mechanotherapy: (1) mandibular incisors must be uprighted over their bony support, (2) maxillary anterior tooth positions must be controlled, and (3) adequate posterior vertical dimension control must be used to prevent extrusion of maxillary and mandibular posterior teeth. To control the vertical dimension, some clinicians recommend extraction treatment because premolar extractions have been associated with closure of the mandibular plane angle. This rationale for extraction is sometimes called the “wedge hypothesis,” which suggests that orthodontic forward movement of the posterior teeth after maxillary and mandibular premolar extraction leads to a reduction in the vertical dimension. However, in the treatment of bialveolar dental protrusion, minimum mesial movement of the posterior teeth is desired because any anchorage loss in the anteroposterior dimension can compromise maximum retraction of the anterior teeth, and this can have detrimental effects on the patient’s overall facial esthetics. In addition, recent evidence suggests that occlusal movement of the posterior teeth tends to keep pace with the increase in anterior facial height, thus maintaining the mandibular plane angle and nullifying any bite-closing effect of posterior protraction. In other words, even though the molar moves forward in premolar extraction patients, the vertical dimension of the face is maintained by extrusion of the posterior teeth. Therefore treatment of these patients requires excellent control over the posterior teeth in both the horizontal (sagittal) and vertical directions. This is perhaps more relevant in adults whose treatment options are limited, since growth modification with headgear, chincup, bite-block, and so on, is not an option.
Over the years, a combined surgical-orthodontic approach has been used to address this predicament. But with every invasive procedure, certain risks are involved, and postoperative complications after orthognathic surgery are also a matter of concern. Johnston reported that 10% of patients ultimately experience total condylar resorption after orthognathic surgery. In another study, patients treated with orthodontic camouflage reported fewer functional temporomandibular joint problems than did those treated with surgery. To put this issue in perspective, for some patients, the need for dramatic changes is so great that the risks involved with surgery make sense, but, for others with perhaps a lesser need, surgery’s capacity for greater change might not be worth the risk. Additionally, there are ranges of vertical excess; most patients do not have an extreme vertical facial pattern but, rather, a slight or moderate tendency toward it. Hence, there is a need to explore other alternatives, especially for patients at the orthodontic-surgical borderline.
In the past, some case reports and clinical studies have demonstrated that skeletal anchorage systems can widen the spectrum of orthodontics, allowing treatment previously considered impossible. The following case presentations highlight the efficacy of mini-implants for vertical control of the posterior teeth during implant-assisted en-masse retraction of anterior teeth in patients having a medium or high Frankfort mandibular plane angle (FMA) and severe bialveolar protrusion, requiring maximum anchorage.
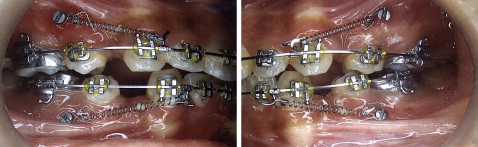
The patients were treated with the preadjusted edgewise appliance system (Roth prescription; slot size, 0.022 × 0.028 in). After initial leveling and aligning, 0.017 × 0.025-in stainless steel archwires with hooks distal to the lateral incisors were placed in both arches. Titanium mini-implants (diameter, 1.3 mm; length, 8 mm) were placed between the roots of the first molar and the second premolar in all 4 quadrants. The surgical procedure involved preparing a hole with a pilot drill under constant irrigation with a coolant and placing the mini-implants with a driver. The implants were immediately loaded with precalibirated nickel-titanium closed-coil springs (150 g; Ultimate Wireforms, Bristol, Conn) extending from the implant head to the crimpable hooks for en-masse retraction of the maxillary and mandibular anterior teeth. The directions of the applied force were upward and backward for the maxillary arch, and downward and backward for the mandibular arch. The nickel-titanium coil springs in the maxillary arch were left in place for at least 2 or 3 months after complete space closure to obtain a tight overjet and close any residual spaces.
Case 1
This patient was a 24-year-old woman with chief complaints of forwardly placed maxillary and mandibular front teeth and an unesthetic smile. She had a symmetric face with a convex profile because of the severe dentoalveolar protrusion and retrognathic mandible. Intraorally, Class I molar and canine relationships were evident, and overjet and overbite were 3 and 1 mm, respectively. She had a steep mandibular plane with severe labioversion of the anterior teeth ( Fig 1 ). The treatment plan called for extraction of the maxillary and mandibular first premolars, with high anchorage in both the anteroposterior and vertical directions to facilitate complete retraction of the anterior teeth into the extraction spaces.
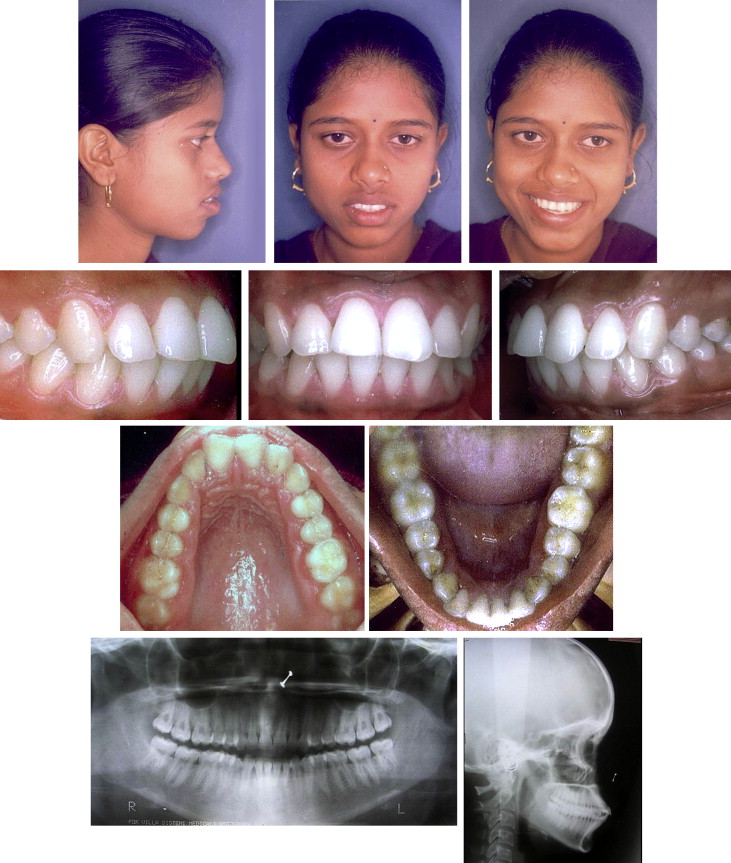
All 4 first premolars were extracted, and, in the same appointment, mini-implants were placed in all quadrants. Initial leveling and alignment were achieved with 0.016-in and 0.016 × 0.022-in nickel-titanium archwires. The archwires were cinched to avoid proclining the incisors. En-masse retraction of the maxillary and mandibular anterior teeth was carried out with 0.017 × 0.025-in stainless steel archwires by using implant-based anchorage and nickel-titanium coil springs ( Fig 2 ).

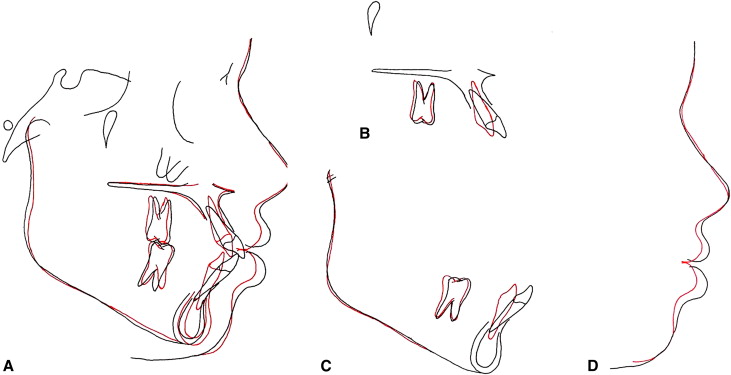
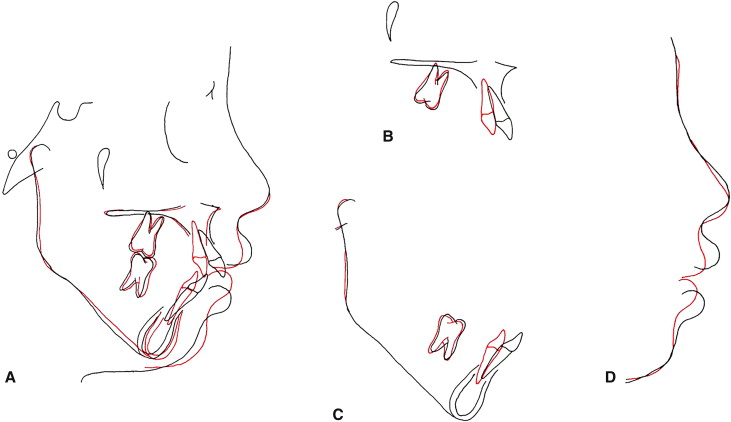
After 22 months of active orthodontic treatment, a dramatic improvement in the facial profile was obtained. The upper and lower lips were retracted by 4 and 5 mm, respectively, and the mentalis strain was eliminated. The maxillary and mandibular superimpositions showed significant intrusion of the upper and lower incisors with more than 8 mm of retraction. Distalization of the molars was also noted. There was excellent control over the posterior vertical dimension as shown by the intrusion of the molars. Consequently, in the overall superimposition, the FMA decreased by 3°, with a forward displacement of the chin by 2 mm ( Figs 3 and 4 ; Table I ).

| Measurement | Normal | Pretreatment | Posttreatment | Difference ∗ |
|---|---|---|---|---|
| SNA (°) | 82 ± 2 | 84 | 84 | 0 |
| SNB (°) | 80 ± 2 | 81 | 84 | 3 |
| ANB (°) | 2 | 3 | 0 | –3 |
| NPg-FH (°) | 89 ± 3.9 | 91.5 | 93 | 1.5 |
| FMA (°) | 25 | 25 | 22 | –3 |
| SN-GoGn (°) | 32 | 35 | 32 | –3 |
| U1-SN (°) | 102 ± 2 | 124 | 108 | –16 |
| IMPA (°) | 90 | 102 | 87 | –15 |
| U1-L1 (°) | 130 ± 5 | 102 | 136 | 34 |
| E-line: U (mm) | –4 | 1.5 | –2.5 | –4 |
| E-line: L (mm) | –2 | 6 | 1 | –5 |
| G-Sn-Pg′ (°) | 12 ± 3 | 18.5 | 15 | –3.5 |
Case 2
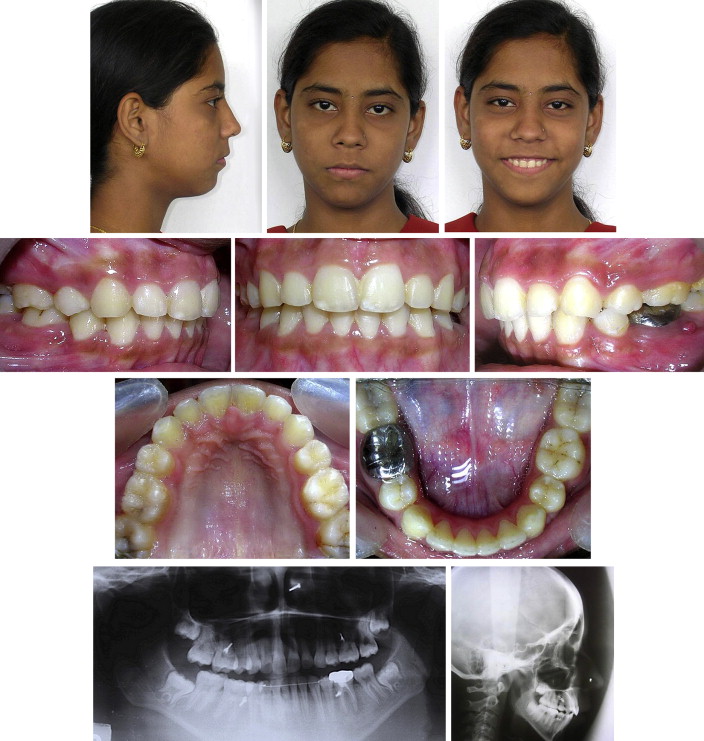
This patient, 17 years 5 months of age, had a chief complaint of proclined maxillary and mandibular front teeth. She had a leptoprosopic facial form with an exaggerated FMA (41°) and an ANB angle of 8° (SNB, 72.5°), suggesting a skeletal Class II malocclusion. The upper and lower lips were protruded, with an increased interlabial gap at rest and excessive gingival display on smiling.
The clear-cut hyperdivergent skeletal pattern and the need for anterior tooth retraction made it necessary to remove the maxillary and mandibular first premolars. The mandibular incisors had to be overly upright, even though they were at 93° (IMPA) relative to the mandibular base, if facial esthetic improvement was to be realized for this patient ( Fig 5 ).

Two treatment options were presented. The first option was orthognathic surgery involving maxillary impaction and mandibular advancement. This would have been an ideal treatment for correcting the underlying skeletal discrepancy and improving the overall facial esthetics, if had the patient agreed. The second option consisted of camouflaging the underlying skeletal discrepancy by extracting the first premolars and retracting the anterior teeth with implant-supported anchorage ( Fig 6 ). The patient readily agreed to this option. It took 11.5 months to close the extraction spaces. The extraction spaces in the mandible closed first, but those in the maxilla took several more months.
Mini-implant–supported retraction produced considerable improvement in her overall facial esthetics, with notable changes in lip posture and balance, especially the lower lip. The gummy smile decreased, with less exposure of the gingival tissue on smiling. The skeletal Class II relationship drastically improved by a 4° reduction in the ANB angle; the SNA angle decreased by 1.5°, and the SNB angle increased by 2.5°. Anterior rotation of the mandible led to improved chin prominence ( Figs 7 and 8 ; Table II ). Cephalometeric superimpositions showed that significant retraction and intrusion of the maxillary and mandibular incisors was obtained. The posterior teeth also appeared to be intruded by approximately 1.5 mm. Overall, facial convexity was reduced by 3.5°, with over 5 mm of retraction of the upper and lower lips. The lips were completely competent, with a harmonious mentalis muscle posture.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


