As described in this article, there are many advances in topical and local anesthesia. Topical and local anesthetics have played a great role in dentistry in alleviating the fears of patients, eliminating pain, and providing pain control. Many invasive procedures would not be performed without the use and advances of topical/local anesthetics. The modern-day dentist has the responsibility of knowing the variety of products on the market and should have at least references to access before, during, and after treatment. This practice ensures proper care with topical and local anesthetics for the masses of patients entering dental offices worldwide.
Key points
- •
Fear and anxiety are the main reasons patients do not go to or follow up with the dentist.
- •
The modern-day dentist has the responsibility of educating fearful patients on the many advances to minimize pain.
- •
Educating patients of the advances in anesthesia practiced in dentistry can alleviate psychogenic pain.
- •
Depending on the procedure, it is imperative that the clinician choose the best anesthesia for the job at hand.
- •
Clinicians who provide care to toddlers should be aware of the low safety margin in children that can lead to local anesthetic overdose.
Topical and local anesthetics (LAs) are the unsung heroes in modern-day dentistry. There are times when older patients sit in a dental chair and share the experiences they endured as a child or stories they heard of dentistry being performed with not enough or without any LA. The experiences are often described as torturous or barbaric. These stories of bad experiences over time have allowed fear to set into the minds of many patients. Fear and anxiety (usually involving the needle or the injection) are the main reasons patients do not go to or follow up with a dentist. Although in contrast, pain is the reason a fearful patient will present to the dental office.
Dentistry has evolved to a point where we can now focus on preventive treatment to avoid dental caries, which oftentimes contribute to a host of painful experiences (ie, injections, abscess, and so forth). This will involve the Dentist educating the “fearful” patients of the many advances in dentistry to minimize pain and to improve the overall oral hygiene, which will lessen the likelihood of discomfort in future visits. Educating patients of the advances in anesthesia practiced in dentistry can oftentimes alleviate psychogenic anxiety. Trust is also an important factor; if patients trust their doctor, they may be more willing to try procedures with multiple visits in order to save as opposed to extracting a tooth or a group of teeth. The experienced clinician will more likely have a variety of techniques learned over the years that can help build a trusting relationship with patients.
Pain is defined as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage” by the International Association for the Study of Pain. Acute pain is caused by a noxious stimulation (trauma, abnormal function of a muscle, or a disease) that lasts less than or cured within 6 months’ duration. Chronic pain often lasts longer than 6 months and can be associated with a disease and possibly have psychological effects. “Pain initiated or caused by a primary lesion or dysfunction in the nervous system” is known as Neuropathic pain. Nasri-Heir and colleagues went further to state “chronic pain disorders, such as neuralgias, chronic musculoskelatal disorders, and various forms of neurovascular pain, may produce equivalent pain but usually are not secondary to tissue damaging events.”
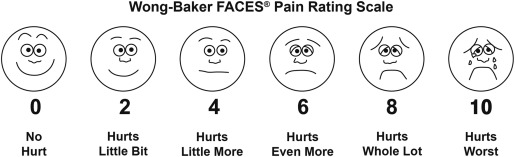
There are 2 common methods to evaluate pain management: the visual analog scale (VAS) and the McGill Pain Questionnaire (MPQ). The latter (MPQ) involves a checklist of words describing symptoms and a scoring system related to the quality of pain from head to toe. This tool is quite lengthy (not recommended for private practice or high-volume dental clinics) and is used in the management of pain syndromes. Now the VAS is basic, simple, and can be used to determine the intensity of pain from children to the elderly ( Fig. 1 ). Essentially it is a horizontal line numbered from 0 to 10, with 0 representing no pain and 10 as the worst possible pain. Gomella and Haist state that it is called the “fifth vital sign” and is commonly used in the hospital setting.
An experienced and oftentimes skilled clinician will give serious thought to the type of topical anesthesia and LA administered before, during (if needed), and after the procedure (if needed). Depending on the procedure (minimally invasive, invasive, minor, or major surgery), it is imperative that the clinician choose the best anesthesia for the job at hand. Malamed offers a rational approach to selecting an appropriate LA:
- 1.
The length of time for which pain control is necessary
- 2.
The requirement for pain control after treatment (postoperative pain control)
- 3.
The requirement for hemostasis during the procedure
- 4.
Any contraindications involving a selected or specific group of anesthetics (ie, true documented reproducible allergy)
Clinician’s who provide care to toddlers and children should be aware of the low safety margin in children that can lead to LA overdose. Hersh and colleagues mention that “the cardiovascular effects of local anesthetic overdosage include vasodilation, which in turn can lead to a drop in systemic blood pressure… Death can occur due to either respiratory depression or cardiac arrest.” The modern-day dentist should be knowledgeable of the number of LA–induced toxicities involving children and the administration of 2% plain lidocaine and 3% mepivacaine (ie, Carbocaine, Polocaine, Scandonest). Yagiella stated “it is advisable to use a preparation containing a vasoconstrictor, if not doing so would result in more total drug being administered.”
Isolated systolic hypertension is commonly seen in middle-aged and elderly patients, with blood pressure (BP) greater than 160 mm Hg/less than 90 mm Hg; dental care is commonly treated under appropriate LA and compliance of medications (along with follow-up visits by their primary care physician). Any patient with a systolic BP of 180/100 should not be seen or treated with elective dental care (ie, LA with or without epinephrine) but should be given a medical consult, only to return after the BP is controlled and patients have written clearance from their physician and/or cardiologist. In cases with a BP >180/120 is Malignant Hypertension, is considered a medical emergency.
Today, the most popular treatment in dentistry involves the planning, placement, and restoration of implants. Steinberg and Kelly state that “when placing mandibular implants, it is not necessary to administer an inferior alveolar block injection for adequate local anesthesia… Local infiltration provides sufficient anesthesia to place an implant with either flap or flapless techniques.” They explained further that the primary advantage of not giving a block injection for implant placement in the mandible “is so the patient has some awareness and perception around the inferior alveolar nerve (IAN).” Paresthesia is defined as persistent anesthesia or altered sensation well beyond the expected duration of anesthesia, which involves sensations of numbness, swelling, tingling, and itching. Malamed went further to state that “…paresthesia is one of the most frequent causes of dental malpractice litigation.” The dentist must be well aware of this term as it relates to
- 1.
The administration of certain LAs and the various techniques
- 2.
Extraction of third molars (wisdom teeth)
- 3.
Surgical incisions/flaps injuring the lingual or mental nerve (neurotmesis)
- 4.
Drilling an osteotomy and/or implant placement in which the regional nerve is crushed (neuropraxia, axonotmesis) and so forth
Hillerup and Jensen recommended in 2006 that “articaine should not be used by inferior alveolar nerve block… it had a greater propensity for paresthesia.”
A complete Blood Count (CBC) and differential, if needed, should be obtained on medically compromised patients suspected of bleeding and thrombotic disorders. It is imperative for the dentist to avoid the administration of local anesthesia to a patient with < 50,000 Platelets. Any invasive treatment without platelet replacement therapy will lead to excess bleeding.
One advancement in modern-day dentistry is the use of LAs as diagnostic nerve blocks when trying to rule out a local versus a central cause of pain.
It is each clinician’s responsibility to know about the classification, potency, toxicity, metabolism, excretion, pregnancy classification, contraindications, and manufacturer’s recommended dosage (MRD) for the use of LAs according to the patients’ body weight (children, elderly, or adults).
Multiple sources of reference (especially evidenced-based studies) should be used to eliminate biased opinions related to LAs.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


