(1)
Department of Endodontics, Nova Southeastern University College of Dental Medicine, Fort Lauderdale, FL, USA
Saving Traumatized and Diseased Immature Teeth
Adults who have root canal treatments to save fully mature permanent teeth with a diseased necrotic or irreversibly injured pulp can benefit from a success rate of over 90 % over 10 years [1]. Younger aged patients with developing immature permanent teeth present special problems to save their teeth following dental traumatic injury (DTI) or caries decay. The DTI of children’s immature teeth damages the pulp; in the case of luxation injuries, the trauma can rupture the neurovascular supply at the level of the apical foramen, whereas in a root fracture, the rupture can occur at the level of the fracture [2]. A disruption to the blood supply to teeth can cause tissue asphyxia, which will lead to necrosis and a loss of pulp vitality [3]. The traumatized pulp can suffer irreversible pulpitis, which will eventually lead to liquefaction necrosis [4]. After the pulp loses its vitality, the normal development of the teeth is stopped [5]. The immature teeth can have very thin fragile dentinal walls making them prone to fracture [6] after a conventional root canal treatment. The endodontic treatments for traumatized and immature teeth with a necrotic pulp can vary. Some dentists remove the necrotic tissues and obturate the root canal with gutta-percha (rubber) [7], composite resin, or mineral trioxide aggregate (MTA) [8]. The problem with all these obturation procedures is that they can halt the growth of the tooth at an immature stage of root development.
Diagnosing the Health of the Pulp in Traumatized and Diseased Teeth
Lack of toothache pain is not always a good indicator for pulp vitality in traumatized teeth. Pulp necrosis can be non-painful, whereas irreversible pulpitis can be associated with episodes of lingering toothache pain in response to hot or cold drinks and food, or even asymptomatic pain [9]. Teeth with a necrotic pulp are nonresponsive to cold and electric pulp sensibility testing. Teeth with irreversible pulpitis will have a greater lingering pain in response to cold sensibility testing and electric pulp sensibility testing compared to adjacent and contralateral teeth. Sometimes the results of the cold and electric pulp sensibility tests are difficult to interpret for diagnosing pulp vitality because there can be varying degrees of necrosis and inflammation within the teeth with multiple canals [10]. The interpretation of the pulp vitality or necrosis and pulpitis should include the SOAP framework [11]: subjective information, objective information, assessment, and a plan for treatment.
Treatments for Traumatic Injuries and Caries Decay to Immature Teeth
Endodontic treatments for traumatized immature permanent teeth with an exposed pulp can vary considerably among dentists. Periradicular inflammation and pulpitis following trauma can initiate the resorption of dentin and bone. Normally, an intact tooth is resistant to resorption, even if pulpitis and periradicular inflammation are present. However, when an injury damages the protective layer of cementum, pulpitis, or periodontium, it can allow root resorption to occur [12]. Resorption of the dentin surface by dentinoclast activity from the center to the periphery can occur. Most of these cases are asymptomatic, but over the long term, pink spots can be observed where advanced internal resorption has taken place. To prevent resorption and spread of necrosis and infection, some dentists will debride the necrotic pulp or tissues with irreversible pulpitis and obturate the root canal with gutta-percha [7], similar to the conventional treatment provided to fully mature adult teeth, whereas other dentists will obdurate the root canals with composite resin, calcium hydroxide [13], or mineral trioxide aggregate (MTA) [14]. These procedures can be successful to save immature teeth with thick dentin walls and with low levels of necrosis or infection, because these teeth do not need continued mineralization or disinfection for their survival. Most immature teeth with a necrotic pulp or irreversible pulpitis will benefit from stimulating mineralization within the apical root canal to close the apex and to help disinfect the root canal with calcium hydroxide and/or MTA using an apexification procedure [15–22]. The apexification procedure is the most common and highest standard of care for immature teeth with a necrotic pulp or irreversible pulpitis. However, the development of the teeth will cease at an immature stage of development; thus weak dentinal walls and short roots will remain. For teeth with very thin dentinal walls which are likely to fracture and need strengthening, a revascularization procedure can be used to disinfect the root canal with antibiotics and revitalize new tissue formation [22–33]. The revascularization procedure is so called because it accomplishes tissue formation within the root canal by blood revascularization from the periapical tissues through the open apex. Alternatively, the necrotic and irreversible pulpitis tissues can be debrided, the root canal disinfected, and a scaffold placed inside the root canal to promote tissue formation in a regenerative endodontic procedure [34–37]. The new tissue formation can mineralize the dentin and continue root development and maturation. The continued formation of dentin and development of the roots in weak immature teeth should help prevent the loss of these teeth to subsequent fracture. Very few endodontic revascularization procedures have been performed on severely traumatized teeth where resorption is expected. It is not yet clear if MTA apexification is more beneficial for severely injured teeth than a regenerative endodontic procedure.
Traumatized or caries-affected immature teeth with a vital pulp which does not have irreversible pulpitis or necrosis can continue their root development and dentinal wall thickening after the removal of damaged coronal pulp tissue in a procedure known as apexogenesis [38, 39] or where 2 mm of coronal pulp tissue is removed in a Cvek partial pulpotomy procedure [40–43].
A flow chart of the suggested protocols for endodontic regeneration treatments according to the status of the pulp and the need to save the teeth are shown in Fig. 3.1.
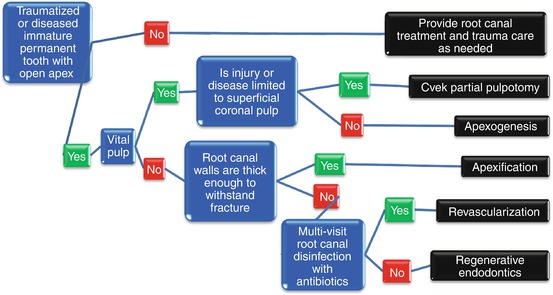
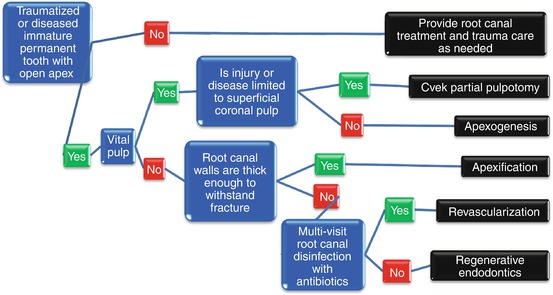
Fig. 3.1
Flow chart of treatments for traumatized or diseased immature teeth
Endodontic Terminology for Treatments for Immature Teeth
The terminologies for the endodontic treatments for immature teeth are:
-
Necrotic pulp—Death of the cells of the dental pulp.
-
Irreversible pulpitis—Chronic inflammation of the dental pulp which cannot be reversed to heal the damaged tissues, thus the prognosis is that the pulp will become necrotic.
-
Apexogenesis—A vital pulp procedure which debrides the coronal injured pulp from a root canal. The removal of the superficial injured pulp will allow the remaining vital pulp to continue the maturation and physiological development of the roots.
-
Cvek partial pulpotomy—A vital pulp procedure which debrides 2 mm of coronal injured pulp from a root canal. The removal of the superficial injured pulp will allow the remaining vital pulp to continue the maturation and physiological development of the roots.
-
Apexification—A necrotic pulp and irreversible pulpitis procedure which debrides, disinfects, and obturates the root canal of immature teeth. The obturation of the root canal with calcium hydroxide or mineral trioxide aggregate (MTA) will induce a calcified barrier to help save the tooth.
-
Revascularization—A necrotic pulp and irreversible pulpitis procedure which disinfects the root canal with antibiotics or/and antimicrobial agents. The periapical tissues are instrumented through the open root apical foramen to cause bleeding into the canal to revascularize it, thereby promoting tissue formation within the root canal for the continued deposition of mineral to strengthen dentin and grow the roots of immature teeth.
-
Regenerative endodontics—A necrotic pulp and irreversible pulpitis procedure which debrides the tissues from the root canal, disinfects the root canal, and instruments the periapical tissues through the open root apical foramen to cause bleeding into the canal to revascularize it. In addition to adding a scaffold or biological procedure within the root canal to promote vital tissue formation which will continue the deposition of mineral to strengthen dentin and grow the roots of immature teeth.
-
Root canal treatment—A necrotic pulp and irreversible pulpitis procedure for mature teeth which debrides the tissues and disinfects the root canal by cleaning and shaping.
Apex Size and Stage of Tooth Maturity
When the pulps of fully mature adult teeth with a closed apex become traumatized and necrotic or have irreversible pulpitis, their debridement followed by root canal obturation with gutta-percha is an extremely successful procedure [1]. In immature teeth with an open apex, the apexification procedure removes the necrotic pulp, which is often successful in alleviating toothache pain and for preventing the spread of necrosis and infection into periapical tissues [15–22]. Nonsurgical endodontic treatment is not ideal, because instrumentation could further weaken the thin walls of immature teeth and make them more prone to fracture. Traumatized immature teeth with a necrotic pulp could benefit from revascularization [22–33] and regenerative endodontic procedures [34–37], whereas traumatized immature teeth with a mostly vital pulp could benefit from Cvek partial pulpotomy [40–43] and apexogenesis [34, 36–40] to promote the continued maturation and root development of the teeth. The size of the root apical foramen is a critical factor to consider when deciding which endodontic procedure will be the most beneficial to save the tooth. In teeth that are almost fully mature, a small apical foramen will limit blood flow into the root canal. Teeth with a restricted blood flow are not likely to revascularize and regenerate, because it is not sufficient for new tissue development inside the root canal. It has been found that an apical foramen diameter of 1.1 mm or wider is needed to successfully accomplish revascularization of tissues within the root canal space [44]. The formation of tissues inside the root canal following revascularization is believed to occur by the delivery of mesenchymal stem cells [45] which form new vital tissues. If the apical foramen is less than 1.1 mm, it is not recommended to attempt root canal revascularization or pulp regenerative endodontic procedures. It is also not recommended to attempt to instrument the apical foramen to make it wider for the purpose of revascularization or regeneration, since this could weaken the roots of the immature teeth and make them more susceptible to fracture.
Age, Health Status, and Compliance of Patients
The endodontic treatments for immature teeth with vital pulps and necrotic pulps have been mostly limited to children and adolescents, between the ages of 6 and 17 years. There have been some patients who were 44 years of age at the time of pulp revascularization [46]. After 18 years of age, all the teeth of patients, except third molars, can be expected to be fully mature with long roots, thick dentinal walls, and a closed apical foramen. In some rare instances, the teeth in older aged patients can still have a wide-open apical foramen because of developmental anomalies or because of past trauma or a caries infection which halted the development of the teeth.
Regenerative endodontic procedures should never be used to preserve deciduous (baby) teeth. If deciduous teeth become traumatized or injured, they should be maintained by restoration. If restoration is not a suitable treatment, the deciduous teeth should be extracted. The reason for not using regenerative procedures to preserve deciduous teeth is because of the risk of retaining these teeth and disrupting the eruption of the permanent adult teeth. Given these age restrictions, it is not advisable to deliver regenerative endodontic procedures to patients younger than 8 years or older than 16 years of age.
There have been no studies of patients who had genetic diseases, severe medical conditions, or a compromised immune system, which could impair the dental revascularization and regeneration responses. Until evidence becomes available, it can be assumed that patients who have a compromised ability to heal will not be good candidates for regenerative endodontic procedures. This is because the success of regenerative endodontic procedures is dependent on the ability of the tissues to heal in the root canal [34]. If the ability of patients to heal is doubtful because of their medical history, endodontic procedures which do not rely on regeneration should be provided, such as apexification instead of regenerative endodontics to save traumatized or caries-affected teeth.
A retrospective study of 30 endodontic regeneration cases found only two cases (6.7 %) with minor complications restricted to discomfort or discoloration. The complications were minor and restricted to discomfort or discoloration [48]. However, there have been cases were regenerative endodontic treatments have failed, and the teeth had to be saved using an apexification procedure. The reasons why some cases have failed are still under investigation, but patient compliance is a factor. There have been some patients where the regenerative endodontic procedure was initiated but was not completed because the patients failed to attend recall visits to complete the treatment. If a patient has a poor record of attending appointments, it is not recommended in the delivery of a multiple-appointment endodontic treatment which is unlikely to be completed, because the patient will fail to return to complete the treatment.
The degree of trauma and extent of caries decay must be checked prior to initiating endodontic treatment that the tooth damage is within restorable limits to use a crown or dental materials to restore the tooth. Some complicated crown fractures and root fractures may be restorable using revascularization and regenerative therapies. However, if the fracture is complicated and involves the crown and root, that tooth is not acceptable for revascularization and regenerative therapies because of the high risk of microleakage through the fracture. If the tooth has greater than normal mobility, the damage to the tooth-supporting structures may cause the tooth to be lost. Revascularization and regenerative therapies should only be delivered to the teeth which have a healthy periodontal ligament to retain the tooth. A summary of the patient and case selection criteria that need to be considered prior to delivering endodontic therapies are shown in Fig. 3.2.
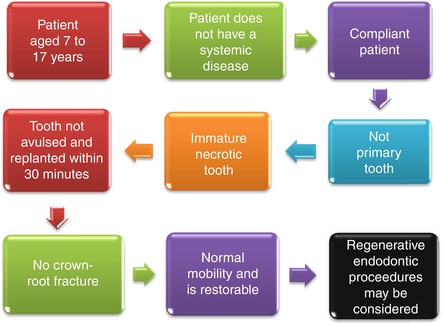
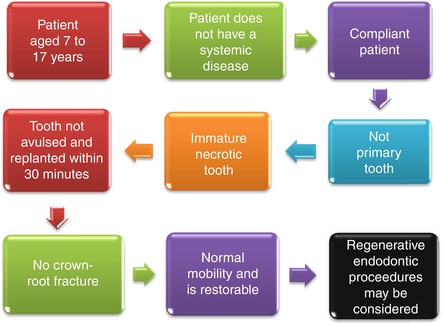
Fig. 3.2
Case selection criteria for regenerative endodontic procedures
Root Canal Disinfection
Sodium hypochlorite is the most commonly used endodontic disinfectant and irrigating solution [48]. Sodium hypochlorite is highly toxic, and it can kill dental pulp stem cells and prevent them from attaching to the surfaces of root canals [49]. The survival of stem cells within the root canals is an essential step to accomplish tissue regeneration; if the cells are destroyed by a toxic root canal environment, they will not form tissues. In addition, because of the wide-open apical foramen, there is no barrier to prevent sodium hypochlorite from leaking out from the root canal space and injuring the periapical tissues. To reduce the level of intracanal toxicity to optimize cell vitality and risk of harm to patients by sodium hypochlorite leakage, sodium hypochlorite must be diluted for use as an endodontic irrigant in the root canals of immature teeth; spillage of the sodium hypochlorite will then cause less injury. Sodium thiosulfate can be used to help neutralize the toxicity of sodium hypochlorite within root canals and reduce any lingering toxicity. Some alternative endodontic irrigating solutions have been developed for reduced toxicity; these include Aquatine EC and noni juice. Alternative irrigating solutions to sodium hypochlorite have not proved popular because of their high cost and lack of evidence for their effectiveness. At the present time, it is recommended to dilute the sodium hypochlorite to 1.25 % for use in regenerative procedures in vital teeth with a wide-open apical foramen.
Dental Materials in Contact with Vital Pulp and Tissues
The regeneration of tissues is sensitive to the environmental conditions within the root canal. The intracanal environment must be sufficiently biocompatible to allow cell survival, cell attachment [49], and new tissue formation. Adhesives, conditioning agents, and acids are toxic to vital tissues and must never be allowed to be in contact with vital pulp, because they can cause tissue necrosis [50]. Most restorative dental biomaterials are not formulated for direct contact with pulp tissues, blood clots, or developing vital tissues. Consequently, restorative dental biomaterials should only be used to restore teeth after a thin protective liner of mineral trioxide aggregate (MTA), Biodentine, or calcium hydroxide [51] has been placed in contact with the coronal pulp tissue, root canal blood clot, or regenerating tissues. The placement of MTA will also help prevent the microleakage of bacteria into the root canal. The presence of intracanal bacteria can cause necrosis of pulp tissue and treatment failure.
Endodontic Sealers in Contact with Vital Pulp and Tissues
Endodontic sealers are needed to obturate root canals after cleaning and shaping to prevent the microleakage of bacteria through the root canal system. Endodontic sealers must never be used as part of regenerative endodontic procedures because they are highly toxic to cells [52] and were never formulated to be biocompatible to soft tissues. The toxicity of endodontic sealers will impede cell survival and tissue regeneration in the root canals and is not suitable to be used in conjunction with regenerative endodontic procedures.
Apexogenesis and Cvek Partial Pulpotomy
Apexogenesis and Cvek partial pulpotomy procedures are similar and so are discussed together. The continued root maturation and development of the teeth following superficial coronal trauma, where the pulps are still vital, are suitable candidates for a Cvek partial pulpotomy procedure [40–43]; if the degree of pulp injury exceeds 2 mm from the pulp horn, an apexogenesis procedure [38, 39] is more suitable. Both these procedures remove the coronal pulp to prevent pulpitis and injury from spreading and affecting the whole pulp. Most of the pulp and root canal surface are not touched as part of these procedures, because the intention is to allow the natural maturation and development of the tooth using the remaining vital pulp tissues. Prior to MTA becoming available, calcium hydroxide powder was used to fill the root canal space, and some dentists still use calcium hydroxide mainly because it is less expensive. The space formerly occupied by the injured or diseased pulp tissue is obturated with MTA or a similar biocompatible material. The steps to accomplish apexogenesis and Cvek partial pulpotomy are shown in Table 3.1
Table 3.1
Steps to accomplish apexogenesis and Cvek partial pulpotomy
|
Case selection for root revascularization treatment
|
|
|
1
|
The traumatized or caries-infected teeth must have a vital pulp that responds normally to cold sensibility testing and is not suitable for other endodontic treatments
|
|
2
|
The tooth must have thin walls that will benefit from a continued development of the root, so that it can become stronger and less prone to failure in later life
|
|
3
|
The patient must be aged 7–16 years and have parents/guardians willing to take them to attend multiple appointments
|
|
First treatment visit
|
|
|
4
|
Check the patient’s health history and that they are healthy enough for endodontic treatment
|
|
5
|
Take a pretreatment radiograph and conduct a radiographic examination of the tooth and surrounding tissues
|
|
6
|
Check for swelling and lesions. Probe around the tooth margins to locate defects or tracks; if any are identified, they must be restored to seal access to the root canals
|
|
7
|
Check tooth sensibility using cold sensibility testing and electric pulp testing. If the tooth has abnormal sensibility and is injured, the treatment plan will have to change to an apexification. If the tooth responds normally to sensibility testing indicating good pulp vitality, continue to the next step
|
|
8
|
Use a local anesthetic block to anesthetize the involved teeth
|
|
9
|
Isolate the involved tooth with a rubber dam
|
|
10
|
Prepare the access opening. It is important that the opening be in the correct proportion to the canal size to allow for canal instrumentation and filling procedures
|
|
11
|
Use a cervical pulpotomy technique to remove the coronal 2 mm of injured or diseased pulp tissue with a file for the Cvek partial pulpotomy procedure. Remove more pulp tissue that appears injured or diseased until healthy bleeding is observed for the apexogenesis procedure
|
|
12
|
Disinfect the coronal root canal space by flushing it with sodium hypochlorite diluted to 1.25 %. The sodium hypochlorite is diluted to 1.25 % reduce its toxicity. The sodium hypochlorite is delivered and immediately suctioned to minimize extrusion through the vital pulp tissues
|
|
13
|
Do not instrument the coronal dentin because it will weaken the tooth
|
|
14
|
Place white MTA to fill the empty root canal space. It is optional to place a moist cotton pellet above the MTA for 1 week to ensure that it sets. If you do not have MTA, you can use calcium hydroxide
|
|
15
|
An endodontic sealer is not biocompatible for apexogenesis or Cvek partial pulpotomy and should not be used
|
|
16
|
Overlay the white MTA with a temporary material such as Cavit or glass ionomer cement
|
|
17
|
Take a postoperative radiograph
|
|
Second treatment visit
|
|
|
18
|
Check the patient’s health history and that they are healthy enough for endodontic treatment
|
|
19
|
Take a radiograph and check for any changes since the previous visit. If a periapical radiolucency has appeared or increased in size, oral antibiotics may need to be given. The tooth may need an apexification procedure if the tooth has become painful
|
|
20
|
Check for swelling and lesions. Probe around the tooth margins to locate defects or tracks; if any are identified, they must be restored to seal access to the root canals
|
|
21
|
Do not waste time checking tooth sensibility
|
|
22
|
Use a local anesthetic block to anesthetize the involved teeth
|
|
23
|
Isolate the involved tooth with a rubber dam
|
|
24
|
Remove the cotton pellet and restore the teeth with a resin-modified glass ionomer to help prevent microleakage, with a composite resin overlay restoration, or full-crown replacement depending on the severity of crown damage
|
|
Follow-up visits
|
|
|
25
|
If the patient is reporting pain and/or a tissue swelling flare-up is observed, an apexification treatment or other endodontic treatment must be considered
|
|
26
|
The quickest that radiographic changes to root thickening, root lengthening and the resolution of periapical lesions can be observed is 6–12 months
|
|
27
|
Recall the patient every 6 and 12 months for at least 5 years
|
Apexification
The closure of the open apical foramen of an incompletely developed tooth has traditionally been accomplished through an apexification procedure. Apexification is a method of inducing a calcified apical barrier or continued apical development of an incompletely formed root in which the pulp is necrotic [15–22]. Apexification can involve a single [22] or multiple monthly appointments to place calcium hydroxide (100 % powder) inside the root canal to eliminate the intraradicular infection and to stimulate calcification to close the apex. After monthly appointments, the tooth should be stronger to allow the root canals to be obturated with gutta-percha [18]. A problem with calcium hydroxide is that it can alter the mechanical properties of dentin and render these teeth more susceptible to root fracture [17]. The traditional use of calcium hydroxide to accomplish apexification is gradually being replaced by MTA as a one-step technique [19]. The MTA can be placed as an apical plug with calcium hydroxide [53, 54] or even as a root canal obturation material [55]. Although effective, the obturation of whole root canals with MTA is expensive. A developing consensus approach to accomplish apexification is to instrument root canals to remove the necrotic tissue and to place MTA in the root canal apex, with the remainder of the canal obturated with gutta-percha [21, 56, 57].
Some long-term studies of apexification with MTA have reported root apexification and periapical healing [21, 56, 57]. The apexification failure rate of an MTA apical plug with a single placement of calcium hydroxide for immature permanent teeth was 7.1 % over 2 years [22]. Over the longer term, the rate of apexification failures is difficult to predict. Among 200 case reports, some variable success rates have been reported for apexification with calcium hydroxide with evidence lacking about its adverse events or long-term effects [18]. Apexification with calcium hydroxide has not always been successful in completing the root formation of immature teeth or for healing persistent periradicular inflammation and tenderness to percussion [19], avoiding root resorption [53], and there is no clinical evidence that its use may help avoid root fracture. Apical MTA plugs are more effective for accomplishing apexification [56] and for strengthening the roots of traumatized immature permanent anterior teeth [58], but it is not clear whether these MTA apexification procedures are as effective as regenerative endodontic procedures.
Some dentists place calcium hydroxide in the root canal to promote calcification and apexification [17], but calcium hydroxide can also weaken the tooth structure and lower its fracture resistance [17], again making the tooth prone to fracture even after treatment. Ideally, the immature tooth should have a treatment procedure which will promote the continued development of its root, resulting in a stronger tooth which is less prone to fail in later life. A root fracture can affect up to 7 % of permanent teeth, and the weakest teeth are the most prone to fracture [59]. The use of calcium hydroxide to accomplish the apexification of an immature tooth of a 10-year-old boy with a necrotic pulp is shown in Fig. 3.3.
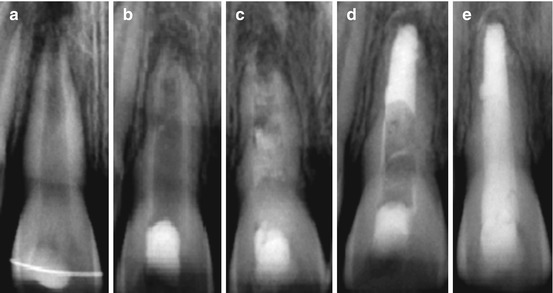
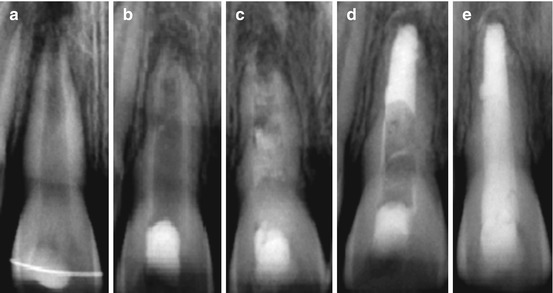
Fig. 3.3
Radiographs of an apexification treatment case in a 10-year-old boy with a necrotic pulp. (a) Non-vital pulp diagnosed. (b) +1 month calcium hydroxide. (c) +1 month calcium hydroxide. (d) +1 week MTA cotton pellet. (e) +3.5 months obturation with MTA
Mineral trioxide aggregate (MTA) is used after calcium hydroxide, or instead of calcium hydroxide as a root canal obturation material in immature teeth following positive treatment outcomes [33]. The most current approach to accomplish apexification is to instrument root canals to remove the necrotic tissue and to place MTA in the root canal apex, with the remainder of the canal obturated with gutta-percha [60, 61]. There have been few long-term studies of apexification with MTA, but the few studies that have been published have reported pulp and periapical healing [60, 61]. The steps to accomplish MTA apexification are shown in Table 3.2.
Table 3.2
Steps to accomplish to accomplish MTA apexification
|
Case selection for root revascularization treatment
|
|
|
1
|
The traumatized or caries-infected teeth must have a nonvital pulp that responds abnormally to cold sensibility testing and is not suitable for other endodontic treatments
|
|
2
|
The tooth must be permanent and immature with a wide-open apical foramen. The tooth must have thick walls that do not need strengthening to avoid fracture
|
|
3
|
The patient must be aged 7–16 years and have parents/guardians willing to take them to attend multiple appointments
|
|
First treatment visit
|
|
|
4
|
Check the patient’s health history and that they are healthy enough for endodontic treatment
|
|
5
|
Take a pretreatment radiograph and conduct a radiographic examination of the tooth and surrounding tissues
|
|
6
|
Check for swelling and lesions. Probe around the tooth margins to locate defects or tracks; if any are identified, they must be restored to seal access to the root canals
|
|
7
|
Check tooth sensibility using cold sensibility testing and electric pulp testing. If the tooth has normal sensibility but is injured, the treatment plan will have to change to an apexogenesis. If the tooth responds abnormally to sensibility testing, continue to the next step
|
|
8
|
Use a local anesthetic block to anesthetize the involved teeth
|
|
9
|
Isolate the involved tooth with a rubber dam
|
|
10
|
Prepare the access opening. It is important that the opening be in the correct proportion to the canal size to allow for canal instrumentation and filling procedures
|
|
11
|
Disinfect the entire root canal with 10 ml of sodium hypochlorite diluted to 1.25 % for 1 min. The sodium hypochlorite is diluted to 1.25 % reduce its toxicity. The sodium hypochlorite is delivered and immediately suctioned to minimize extrusion through the open apical foramen
|
|
12
|
Dry the canals with paper points
|
|
13
|
Measure the working length of the canals with a file inside the canal using a radiograph
|
|
14
|
Do not rely on an apex locator to measure the root canal working length of immature teeth; it is not reliable in teeth with a blunderbuss apex
|
|
15
|
Instrument the root canal to remove necrotic pulp, but avoid weakening the root canal dentin by excessive instrumentation
|
|
16
|
Dry the canals with paper points
|
|
17
|
Etch the root canal walls with 17 % EDTA for 1 min
|
|
18
|
Dry the canals with paper points
|
|
19
|
Flush EDTA from the root canals with sodium hypochlorite diluted to 1.25 % for 30 s
|
|
20
|
Dry the canals with paper points
|
|
21
|
Use white MTA to fill the empty root canal space. It is optional to place a moist cotton pellet above the MTA for 1 week to ensure that it sets. If you do not have MTA, you can use calcium hydroxide. If the root canal was obturated with calcium hydroxide, it will need to be changed each month, for up to three months
|
|
22
|
An endodontic sealer is not needed because the MTA has sealed the root canal
|
|
23
|
Overlay the white MTA with a temporary material such as Cavit or glass ionomer cement
|
|
24
|
Take a postoperative radiograph
|
|
Second treatment visit
|
|
|
25
|
Check the patient’s health history and that they are healthy enough for endodontic treatment
|
|
26
|
Take a preoperative radiograph and check for any changes since the previous visit. If a periapical radiolucency has appeared or increased in size, oral antibiotics may need to be given. The root canal will have to be disinfected again and/or have more calcium hydroxide placed in the canal for another month
|
|
27
|
Check for swelling and lesions. Probe around the tooth margins to locate defects or tracks; if any are identified they must be restored to seal access to the root canals
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


