(1)
Department of Endodontics, Nova Southeastern University College of Dental Medicine, Fort Lauderdale, FL, USA
The success of endodontic treatment is dependent on the obturation of the root canal with gutta-percha and sealers which can seal the entire root canal, thereby preventing microleakage and the reinfection of the root canal. Over time, sealers and gutta-percha have become the standard approach to obturating root canals. Sealers are needed to seal the gutta-percha core material and prevent microleakage. In the absence of sealer, gutta-percha cannot adequately seal root canals and prevent microleakage and reinfection. Gutta-percha is most commonly used to obturate the root canal because it can be placed relatively easily and also be removed relatively easily if the tooth requires retreatment. The quality of root canal obturation can be seen in radiographs and a poor quality of obturation can increase the risk of a flare-up and treatment failure.
Root Canal Sealers
Root canal sealers are needed to adequately seal the root canal space to prevent microleakage. The sealer fills voids and irregularities of the root canal space left unfilled by the obturation core material [1]. Adequate sealing of the obturation material inside the root canal is important to the success of endodontic treatment, because up to 60 % of endodontic treatment failures are caused by the incomplete obturation of the root canal [2]. Root canal may leak and become exposed to periradicular tissue sealers; however, they are generally not very biocompatible [3–6]. Root canal sealers can vary greatly in composition and contain zinc oxide eugenol, calcium hydroxide, glass ionomer, composite resin, silipoint, urethane methacrylate, formaldehyde, and bisphenol A [7, 8]. The sealers are typically delivered by auto-mix syringes to reduce the risk of operator mixing errors. The most widely used sealers are AH Plus, Sealapex, RealSeal, BC Sealer, Apexit, and Pulpdent; the composition of these sealers is shown in Table 8.1.
Table 8.1
Composition of endodontic sealers
|
Group #
|
Product and manufacturer
|
Component A
|
Component B
|
|---|---|---|---|
|
1
|
AH Plus
(Dentsply De Trey, Konstanz, Germany)
|
Epoxy resin
|
Adamantane amine
|
|
Calcium tungstate
|
N,N-dibenzyl-5-oxanonane
|
||
|
Zirconium oxide
|
TCD-diamine, calcium tungstate, zirconium oxide, Aerosil, silipoint oil
|
||
|
Aerosil, iron oxide
|
|||
|
2
|
Apexit
(Vivadent, Schaan, FL)
|
Calcium hydroxide
|
Trimethylhexanedioldisalicylate, bismuth carbonate
|
|
Hydrogenized colophony
|
Bismuth oxide, silicon dioxide, 1,3-butanedioldisalicylate, hydrogenized colophony, tricalcium phosphate, zinc stearate
|
||
|
Silicon dioxide, paraffin oil
|
|||
|
Zinc oxide, calcium oxide
|
|||
|
Polydimethylsiloxane
|
|||
|
Zinc stearate, pigments
|
|||
|
3
|
Endomethasone
(Septodont, Saint-Maur, France)
|
Zinc oxide, Dijodthymol
|
Eugenol and peppermint oil
|
|
Barium sulfate
|
|||
|
Hydrocortisone acetate
|
|||
|
4
|
Pulpdent
(Pulpdent Corp., Watertown, MA)
|
Zinc oxide, calcium phosphate, zinc stearate, and barium sulfate
|
Eugenol and Canada balsam
|
|
5
|
Ketac-Endo
(3M ESPE, Seefeld, Germany)
|
Calcium-lanthane-sodium
|
Polyacrylic acid
|
|
Fluorophosphor-aluminum-silicate
|
|||
|
6
|
N2
(Ghimas, Bologna, Italy)
|
Bismuth nitrate, bismuth carbonate, paraformaldehyde titanium dioxide, zinc stearate, zinc acetate, iron oxide
|
Eugenol
|
|
Peanut oil
|
|||
|
Rose oil
|
|||
|
Lavender oil
|
|||
|
7
|
EndoREZ
(Ultradent Products Inc., South Jordan, UT)
|
TEGDMA, diurethane dimethacrylate, bisglycerol dimethacrylate phosphate; bismuth oxychloride, calcium lactate pentahydrate, silica; benzoyl peroxide
|
TEGDMA, diurethane dimethacrylate, bisglycerol dimethacrylate phosphate; bismuth oxychloride, calcium lactate pentahydrate, silica; p-tolyimino diethanol, phenyl bis(2,4,6-trimethyl benzoyl) phosphate oxide
|
The lack of biocompatibility of these sealers to periodontal cells is shown in the low numbers of cells which can attach to the sealers, as shown in Fig. 8.1.
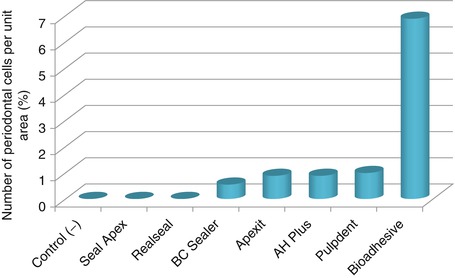
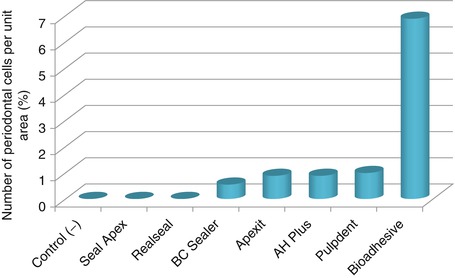
Fig. 8.1
The lack of biocompatibility of some common root canal sealers shown by the lack of periodontal cell attachment. The best treatment was an experimental bioadhesive which is not marketed as a sealer called bioadhesive, but it demonstrates that it is possible to formulate sealers which are more biocompatible
Selecting Obturation Materials
Since the late 1800s, the selection of the root canal obturation material and the accompanying technique for its usage has been a controversial aspect of endodontics. Today, the selection of material for obturation is less controversial. The majority of dentists will use gutta-percha as the primary filling material in root canal therapy [9]. Some dentists in the past used silver points for narrow and extremely curved canals, but this is not recommended; and a few dentists will use alternative materials such as GuttaCore [10], Thermafil [11], or resin-based composite [12] for obturating teeth. In 2004, Resilon, a composite resin obturation material, was introduced [13, 14]. Recent studies have demonstrated that resin composites can prevent more microleakage in comparison to gutta-percha [13, 14] and that roots obturated with composite resin have a greater fracture resistance [15]. The handling properties of composite resin and gutta-percha are similar [14], and since GuttaCore contains cross-linked gutta-percha, it also has good handling properties. GuttaCore was developed from a Thermafil carrier system [16]. It is possible to obturate teeth with other materials, such as MTA or cements, but the high cost can make those obturation materials prohibitively expensive for everyday use.
Gutta-Percha Obturation
The reason for the success of gutta-percha among dentists is because it is easy to manipulate into the root canal, it is radiopaque and easily seen on radiographs, and it can be removed from the canal and be replaced when necessary [17]. Fresh gutta-percha has good handling properties, while aged gutta-percha can become brittle. Gutta-percha is an isomer of natural rubber derived from the Taban tree (Isonandra perchas). The natural chemical form of gutta-percha is 1, 4-polyisoprene [18]. It was first used in dentistry in the late 1800s as a temporary restorative material and then to obturate root canal systems [19]. The semi-plastic physical properties of gutta-percha allow it to be reshaped and molded within the canal system by condensation forces [20]. Gutta-percha can be softened by heated instruments and chemicals such as chloroform and eucalyptol. This makes gutta-percha easy to obdurate the root canal and easy to remove from the root canal if a retreatment is needed. An advantage of gutta-percha is that it is inert to the periapical tissues if it should become extruded past the root apex [21]. The quality of root canal obturation with gutta-percha is important; if a root canal is poorly obturated, it can be associated with nonhealing periapical lesions in up to 65 % of treatments [22], and 60 % of endodontic treatment failures are caused by the incomplete obturation of the root canal [2]. The difference between a poorly obturated and a retreated well-obturated root canal can be seen in Fig. 8.2.


Fig. 8.2
Obturation quality of gutta-percha in root canals. The left radiograph shows a poorly obturated tooth because the root canals are not completely obturated. The right radiograph shows a good quality of root canal obturation. (a) Preoperative radiograph with poorly obturated canals. (b) Postoperative radiograph with obturated retreated canals
Some dentists prefer to insert the gutta-percha point into the canal without altering it [23], while other dentists like to soften the gutta-percha with heated instruments or chemicals. The softened gutta-percha can then be condensed into the canal using lateral or vertical condensation [24]. The separation of obturation methods into vertical or lateral condensations is unrealistic, since it is physically impossible to condense either laterally or vertically alone [25]. Often, the condensation procedure to insert the gutta-percha will vary according to the shape of the instrumented root. If the shape of the instrumented root matches the shape of the gutta-percha point, then not much condensation of the gutta-percha is needed to get a good obturation of the root canal. However, if the nearest size of gutta-percha point is a poor-fit, it might need to be condensed to fit the root canal space. Gutta-percha is most difficult to place into a minimally prepared narrow canal. Gutta-percha requires condensation pressure be applied in the apical third region of the canal, and it can easily become extruded through an open apex, leaving fragments in the periradicular tissues [26].
Gutta-percha filling techniques use a prefitted primary point procedure, verified by a radiograph to fit the full length of the canal and to still fit tightly in the apical region of the root canal [9]. Normally, if the instrumented canal has an adequate condensation space or flare has been prepared, it is often impossible to fill the length of the canal with a gutta-percha point that fits tightly at the root apical region. The largest possible gutta-percha point is normally selected according to the size of the last instrument used to the full length of the prepared canal. A radiograph of the root canal must be taken with the gutta-percha point inserted to check that it fits the working length of the root canal. If it does not fit, it may be necessary to reprepare the apical aspect of the canal or to select another gutta-percha point.
The root canal must be dried with paper points prior to its obturation, as residual irrigation fluids will leave voids [27]. The sealer is evenly coated on the prepared canal surface, with the last instrument used to spread it throughout the canal length using an up and down motion [28].
The fitted gutta-percha point is cut to the root canal working length, and a spreader is used to condense it into the root canal space. A radiograph is taken to evaluate the quality of the root canal obturation and to assess the need to reposition the point or apply more condensation pressure. In anterior teeth, if the filling is satisfactory, the gutta-percha should be removed to the gingival line or below it, because gutta-percha can discolor the tooth [29]. In posterior teeth, it is advisable to have a “bed” of gutta-percha on the floor of the pulp chamber; this can act as a guide for retreatment or to alert the operator that he is getting too close to the floor of the crown when making a final preparation [30]. It will also assist in the sealing of furcal accessory canals.
Because no one gutta-percha obturation technique could possibly satisfy all endodontic situations [31], it is necessary to consider some modifications of the basic technique. In a root canal where an adequate apical stop or constriction is impossible to achieve, as in an immature canal after apexification, the gutta-percha point can be custom contoured by dipping the apical 3–4 mm in chloroform and then placing it into the canal with pressure. By the repeated placement and removal of the apical softened point, this uses the apical canal space to mold the gutta-percha to accomplish a good fit. Thin root canals or canals with an extreme curve are more difficult to obturate with standard sizes of gutta-percha points. In these situations, heated instruments or chloroform can be used to chemically soften the gutta-percha for 5 s so that it can be more easily into the curvature and the minimally prepared apex. All of these gutta-percha obturation techniques must be considered to accomplish the goal of fully obturating the root canal. A summary of the terms and techniques for obturating root canals is shown in Table 8.2.
Table 8.2
A summary of techniques for obturating root canal systems
|
Technique
|
Description
|
|---|---|
|
Apical barrier [32]
|
Creating an apical barrier when the apical foramen is open in immature teeth for apexification and is important to prevent the extrusion of gutta-percha into the periradicular tissues. A 2-mm-thick cone of MTA or another biocompatible material such as Biodentine® can be placed in immature teeth as the apical barrier [32]
|
|
Carrier-based (sectional)
|
A sized and fitted section of gutta-percha with sealer is inserted into the final 4-mm apical region of the root canal. The remaining root canal is filled with injectable thermoplasticized gutta-percha using an injection gun such as the SimpliFill device [33]
|
|
Carrier-based (thermoplasticized)
|
A warm gutta-percha on a plastic carrier is delivered directly into the canal to fill it. Some of the main carrier systems are Densfil™, RealSeal™, Soft-Core®, and Thermafil® [34]
|
|
Chemoplasticized
|
The gutta-percha is softened using solvents such as chloroform or eucalyptol and is placed on already fitted gutta-percha points. The gutta-percha points are inserted into the canal, laterally condensed with spreaders, and the remaining canal space is filled with points [35]
|
|
Continuous wave
|
A down-packing (vertical compaction) of core material and sealer into the apical region of the root canal using heating devices such as a System B or Elements Obturation Unit and then backfilling the remaining root canal with thermoplasticized core material using injection devices such as the Obtura Elements Obturation Unit or HotShot heating devices [36]
|
|
Custom cone molding
|
The outer surface of the gutta-percha point is softened using solvents such as chloroform or eucalyptol, and then, it is inserted into the apical region of the canal to make a mold. Gutta-percha shrinks as it hardens, so the point is removed, sealer is placed into the canal, and then the point is reinserted and condensed with spreaders [37]
|
|
Injection (preheated)
|
Sealer is injected into the canal. A preheated, thermoplasticized, injectable core material is injected to obturate the root canal using a heating device such as an Obtura, or Ultrafil, or Calamus® system [38]
|
|
Injection (cold)
|
Sealer is injected into the canal. A cold, flowable core material such as GuttaFlow® is injected to obturate the root canal [39]
|
|
Lateral compaction
|
A gutta-percha point with the same size as the final instrumentation size is cut to the working length of the root canal. The point is coated with sealer and inserted into the canal. The point is laterally compacted with spreaders and other points are added to fill the remaining root canal [40]
|
|
Thermomechanical
|
A gutta-percha point is coated with sealer and placed in the root canal. The point is then rotated with an instrument to warm the core material with friction. The warm core material is then compacted into the root canal [41]
|
|
Vertical compaction
|
A gutta-percha point with the same size as the final instrumentation size is cut to a length of 4 mm. The point is coated with sealer, heated, and inserted into the apical region of the canal. The point is vertically compacted with pluggers, and warm gutta-percha points are added to fill the remaining root canal [42]
|
|
Warm lateral condensation
|
A gutta-percha point with the same size as the final instrumentation size is cut to the working length of the root canal. The point is coated with sealer and inserted into the canal, the point is laterally condensed with a warm spreader, and warm gutta-percha points are added to fill the remaining root canal [43]
|
Summary of the Root Canal Obturation Technique
Situations when it is acceptable to fill the root canal:
Suggested gutta-percha obturation procedure:
1.
Dry the canals by inserting paper points cut to the root canal working length.
2.
Fit a standardized gutta-percha point to the established root canal working length, which is 1 mm short of the root canal length.
3.
Check the fit of the gutta-percha point in a radiograph.
4.
Mark the occlusal or incisal level of the gutta-percha point by pinching it with an instrument.
5.
Place a paper point into the canal that matches the size of the gutta-percha point. Inject the sealer to evenly coat the root canal surface and spread it using the last instrument size used in the root canal preparation.
6.
Dip the gutta-percha point into the sealer, and insert it into the canal to the fitted working length.
7.
If there are any voids, add more gutta-percha to fill them.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


