An ankylosed tooth and adjacent alveolar process can lead to the development of an open bite, an unesthetic smile line, and abnormal function in mastication. Intraoral alveolar bone distraction osteogenesis is an option for treating an ankylosed tooth. The purpose of this clinical report was to show the treatment of a growing patient with an ankylosed maxillary central incisor. A simple tooth-borne intraoral distractor was made with an expansion screw and 0.9-mm stainless steel wire, which enabled it to move easily. Intraoral alveolar bone distraction osteogenesis will give the best results in patients with favorable root length and severely resorbed alveolar bone in the vertical dimension.
Ankylosis means “failure to move” in Greek; it refers to the fusion of a tooth and the alveolar bone that prevents the tooth from physiologic and orthodontic movements. Deciduous molars often become ankylosed, but impacted canines and traumatized maxillary incisors can also be affected. Lack of normal physiologic tooth movements, such as those that occur with mastication and occlusion, can be a causative factor in ankylosis. Andreason suggested that splinting traumatized teeth, preventing physiologic movements, would result in ankylosis.
If ankylosed teeth are misdiagnosed or unrecognized, treatment progress and results can be severely compromised. Unfortunately, it is difficult to diagnose ankylosed teeth in the early stages. Key features leading to diagnosis include lack of mobility and orthodontic movement, tipping of adjacent teeth, ditching of the alveolar process, infraocclusion, and a characteristic dull sound on percussion.
Ankylosis can have regional dentoalveolar and more widespread craniofacial results. Infraocclusion of an ankylosed tooth or tipping of adjacent teeth and the alveolar process can lead to an open bite in the anterior or posterior teeth, midline shifts, changes in facial vertical dimensions, unesthetic face and smile line, occlusal disharmony, and abnormal functions in mastication. The most common treatment for ankylosis is extraction. In a growing patient, extracting an ankylosed tooth often allows for better development of the dentoalveolar process in this region. The adjacent teeth continue to erupt normally and bring the periosteum over the extraction site with them, thereby developing the alveolar bone. In addition, any succeeding permanent teeth will erupt and continue to develop the alveolar process.
In an adult, various procedures such as prosthodontic restorations, luxation, and surgical repositioning are available, depending on the extent and the position of the tooth. Surgical repositioning might involve a single-tooth osteotomy alone or with distraction osteogenesis.
Since Ilizarov pioneered distraction osteogenesis, McCarthy et al, Toth et al, Molina and Ortiz Monasterio, and Guerrero et al made improvements and demonstrated many successful cases in the 1990s. Alveolar bone distraction osteogenesis was introduced to augment the alveolar bone both vertically and horizontally.
In this clinical report, we present the treatment of a growing patient with an ankylosed maxillary incisor treated by intraoral alveolar bone distraction osteogenesis.
Case report
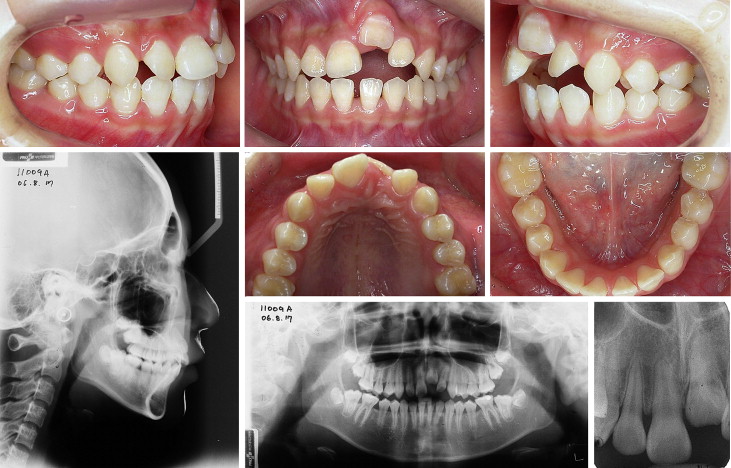
The patient was a girl, aged 11 years 11 months, who had bumped against the corner of a desk and damaged her maxillary incisors when she was 7 years old. The incisors were reimplanted, but the left central incisor eventually became ankylosed, preventing further growth of the alveolar bone, creating an open bite in the maxillary incisors, and resulting in tilting of the adjacent teeth as further dentoalveolar growth and development occurred. The diagnosis of ankylosis of the maxillary incisor was based on loss of movement, infraocclusion, lack of radiographic periodontal ligament space, tilting of adjacent teeth and the alveolar process, and a dull sound on percussion. Additional diagnosis included a skeletal Class II Division 1 malocclusion with cephalometric values of SNA of 87.1°, SNB of 79.1°, and ANB of 7.9° ( Fig 1 ).
In consideration of the patient’s age and the occlusal and esthetic goals, conventional approaches were ruled out. Leaving an ankylosed maxillary left central incisor in place and restoring it prosthetically would further impede vertical development of the alveolar bone, increase the infraocclusion, and severely compromise the esthetic results. However, if the tooth was extracted, significant bone would be lost in this area, and recession of the adjacent periodontal support could occur. Bone augmentation would be required at extraction and again after growth. If a bridge was placed at this time, the central incisor crown would be significantly longer than the contralateral tooth, or there would be a large gap under this pontic. These compromises were considered unacceptable; therefore, extraction and prosthodontic treatment were excluded.
The 2 procedures considered to alter the vertical position of the maxillary incisor and the alveolar bone were a single-tooth osteotomy and alveolar bone distraction ostegenesis. However, the ankylosed incisor needed to be repositioned by approximately 8 mm. This large movement with a single-tooth osteotomy would be impossible because of gingival pull. In contrast, a great deal of bony movement, histogenesis, and tissue remodeling would be possible with distraction osteogenesis. Therefore, this was considered the treatment of choice. The plan was to take advantage of the ankylosed maxillary left central incisor and use it as anchorage to distalize the molars. Subsequently, the ankylosed tooth would be moved by distraction osteogenesis with a tooth-borne alveolar bone distractor.
Several teeth in the maxilla were banded, and an impression was taken to construct an indirect anchorage transpalatal appliance with a 0.9-mm stainless steel archwire ( Fig 2 ). This would be used to consolidate an anterior anchor unit for the distalization of the posterior maxillary dentition.

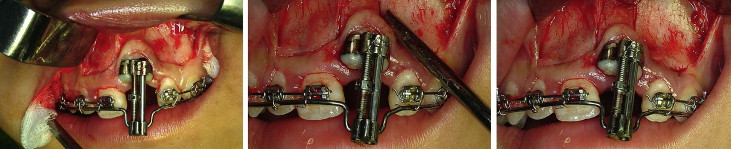
After the maxillary molars were adequately distalized, .022-in slot fixed appliances were placed on the maxillary and mandiblular teeth to provide adequate arch length for the maxillary left central incisor. After presurgical orthodonthic treatment, an intraoral tooth-borne distractor was fabricated with an expansion screw (#198-1223, Forestadent, Pforzheim, Germany) ( Fig 3 ).

The ankylosed tooth was banded and an impression taken. After preexpanding the screw to its final position, it was adapted to the band and the 0.9-mm stainless steel wire. The archwire was carefully soldered to the preexpanded screw and the band. This is important to determine the direction of the distraction. Six to 8 spurs, 1.5 to 2 mm long, were soldered to this wire at interdental spaces for stability.
With the patient under local anesthesia, an interdental osteotomy and subapical osteotomy were performed around the maxillary left central incisor ( Fig 4 ). Mobility of the osteotomy block containing the incisor and the operation of the distractor were confirmed. A key aspect of the surgical procedure was to conserve as much attached gingiva as possible during the incision and suturing.
After a 5-day latency period, distraction was started ( Fig 5 ). Distraction is typically carried out at a rate of approximately 1 mm per day for larger segments of the maxilla and mandible, but 0.5 to 0.8 mm per day would be appropriate for this procedure in alveolar bone. However, in consideration of the strong resistance to movement of the osteotomy block in the early stages of distraction, we elected to distract at the rate of 1 mm per day for the first 4 days. To induce histogenesis, the rate was decreased to 0.4 mm per day. An overcorrection of 1 mm was planned to account for continued vertical growth of the dentition and the potential for relapse. After 2 weeks of consolidation, the distractor was removed, and the maxillary left central incisor bracket was ligated onto the .019 × .025-in heat-activated nickel-titanium archwire ( Fig 6 ). Further healing, remodeling, and consolidation of the osteotomy site continued while the archwire sequence progressed to .019 × .025-in stainless steel ( Fig 7 ). The final results are shown in Figure 8 .





