Introduction
In this study, we evaluated the transverse dentoalveolar changes in the maxillary first molar region after early treatment with the quad-helix appliance.
Methods
Seventy-three consecutive patients (39 boys, 34 girls) who had phase 1 quad-helix treatment were evaluated with cone-beam computed tomography scans taken before phase 1 (mean age, 9.2 years) and phase 2 (mean age, 11.9 years) treatments. Buccal bone thickness, buccal cortical plate thickness, lingual bone thickness, alveolar width, palatal width, and intermolar width were measured by using standardized orientations.
Results
Slow palatal expansion with the quad-helix decreased buccal bone thickness (1.6 mm ± 0.8), and increased lingual bone thickness (1.6 mm ± 1.3) and alveolar width (0.5 mm ± 1.0). Intermolar widths and palatal widths increased 6.5 mm ± 2.9 and 3.9 mm ± 1.8, respectively. At the beginning of phase 2, approximately one third of the patients showed little or no buccal cortical plate on at least 1 side. Patients retained with the Hawley demonstrated some relapse tendencies; patients without retention had the greatest relapse tendencies.
Conclusions
Early treatment with the quad-helix appliance proved to be highly effective in increasing intermolar, palatal, and alveolar widths. The teeth moved through the alveolus, leading to substantial decreases in buccal bone thickness and increases in lingual bone thickness.
Transverse maxillary deficiency and maxillary crowding in children are problems commonly encountered and treated by orthodontists. Early treatment with palatal expansion has been recommended for children with transverse discrepancies, particularly unilateral crossbite, because it has been shown to be associated with abnormal chewing patterns and the development of skeletal asymmetries. Expansion is especially desirable for young Class II Division 1 patients who have constricted maxillae, because the transverse deficiency does not self-correct between the deciduous, mixed, and permanent dentitions. Maxillary arches are also routinely expanded early to relieve crowding, and create broader and more esthetic smiles.
Two basic approaches have been developed to expand the maxilla. Rapid maxillary expansion uses heavier interrupted forces to maximize orthopedic effects, and slow palatal expansion uses lighter continuous forces to move teeth at rates purported to be more physiologic. Slow expansion is commonly accomplished with removable expansion plates or fixed wire appliances such as the W-arch or the quad-helix. The quad-helix provides primarily buccal translation of the molars and does not require patient compliance; removable plates tend to tip the teeth buccally and depend on patient compliance. The quad-helix produces forces between 180 and 667 g, depending on the material used, and the length and the size of the wire. These forces are significantly lighter than those reported for rapid maxillary expansion, which range between 2700 and 7400 g. Quad-helix treatment has been shown to separate the midpalatal suture and significantly increase intermolar width (5–6 mm); it has been reported to be highly successful in correcting crossbites in the mixed dentition. Most of the expansion obtained is due to dental movement. Reported ratios of orthodontic to orthopedic effects range between 6:1 and 10:1 although 1 study reported a much smaller ratio (2:1).
It has been established that excessive tooth movements in the facial or buccal directions can lead to reductions in alveolar bone crest levels, bone dehiscences, and gingival recession. Recent computed tomography (CT) and cone-beam CT (CBCT) studies have demonstrated dehiscences and significant decreases in buccal bone thickness after approximately 3 months of retention in patients treated with rapid palatal expanders. The periodontal and alveolar effects of slow expansion with the quad-helix remain unknown. Such information is important because of the relative amounts of tooth movement reported for the quad-helix appliance. It is especially important to understand the long-term effects of this type of expansion on maxillary molar root positions and the surrounding alveolar bones.
The purpose of this study was to evaluate the transverse changes during and after phase 1 treatment with the quad-helix appliance. Longitudinal CBCT scans taken 2.7 years apart were used to distinguish between the overall, alveolar, and dental changes that took place.
Material and methods
All CBCT scans were taken at 1 location; the patients were treated by 3 orthodontists. The project was granted exemption by the Texas A&M Health Science Center, Baylor College of Dentistry Institutional Review Board. To be included in the study, each patient needed to have phase 1 quad-helix treatment, a CBCT scan taken before phase 1 (T1), and a CBCT scan taken before phase 2 (T2) treatment. The sample consisted of 73 consecutively treated patients (39 boys, 34 girls). The mean ages at T1 and T2 were 9.2 years (range, 6.4–13.8 years) and 11.9 years (range, 9.1–14.8 years), respectively.
All patients were treated with .038-in blue Elgiloy prefabricated quad-helices (Rocky Mountain Orthodontics, Denver, Colo), which were soldered to molar bands. Most patients were treated with a size 3 quad-helix; occasionally, a size 4 was used for larger patients. The forces produced by the sizes 3 and 4 quad-helices have been estimated to be 441 and 278 g, respectively. The quad-helix was delivered approximately 1 week after the initial CBCT scan. Patients were expanded until the lingual cusps of the maxillary first molars were in contact with the buccal cusps of the mandibular first molars. Active quad-helix treatment lasted for approximately 6 months.
The quad-helix was in place for an average of 1.9 years (range, 4 months–5.3 years). In 49% of the patients, the quad-helix was left in place as the retainer until phase 2; 16% had no retention after quad-helix removal, and 35% received maxillary Hawley retainers. All but 2 patients who received Hawley retainers had maxillary 2 × 4 appliances along with the quad-helix. The Hawley was delivered after debonding of the braces and removal of the quad-helix.
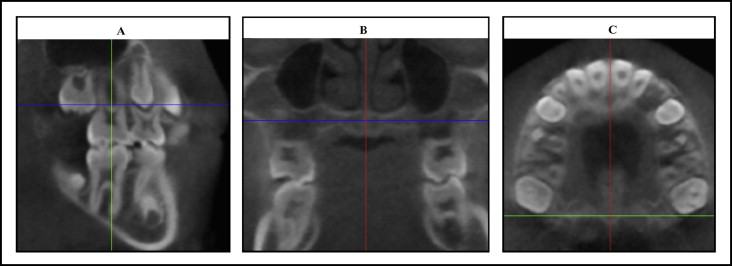
A total of 146 CBCT scans were evaluated. The scans were taken with either the NewTom 3G (Aperio Services, Verona, Italy) (n = 131 scans) or the NewTom DVT 9000 (QR SRL, Verona, Italy) (n = 15 scans). The DICOM files from each scan were renumbered and uploaded into Dolphin Imaging Premium (version 11.0, Dolphin Imaging and Management Solutions, Chatsworth, Calif) and evaluated by a blinded examiner (J.K.C.). By using 3-dimensional imaging software, multi-planar reformatted projections were oriented as follows: (1) the sagittal slice with the long axis of the maxillary first molar parallel to the vertical reference line ( Fig 1 , A ), (2) the coronal slice with the palatal plane and nasal floor parallel to the horizontal reference line ( Fig 1 , B ), and (3) the axial slice positioned at the level of the furcation between the mesiobuccal and distobuccal roots of the maxillary first molars ( Fig 1 , C ).
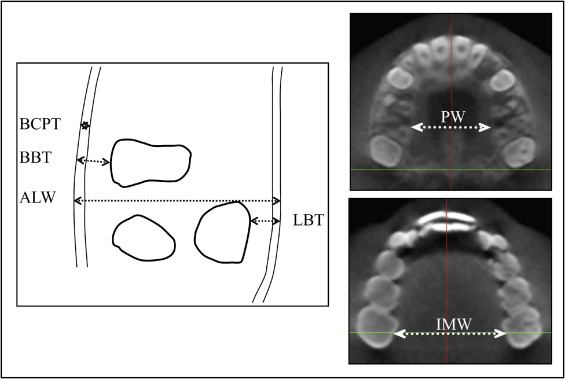
With the axial view, 5 bilateral measurements ( Fig 2 ) were made at the level of the buccal furcation of the maxillary first molar by the primary investigator (J.K.C.) including buccal bone thickness, defined as the shortest distance between the outer buccal alveolar cortical plate and the mesiobuccal root; (2) buccal cortical plate thickness, defined as the distance between the outer and inner borders of the buccal alveolar cortical plate in the interdental area mesial to the maxillary first molar; (3) lingual bone thickness, defined as the shortest distance between the lingual root of the maxillary first molar and the outer border of the lingual alveolar cortical plate; (4) alveolar width, measured from the outer limits of the buccal and lingual cortical plates, passing through the center of the maxillary first molar furcation, approximately perpendicular to each cortical plate; and (5) palatal width, defined as the distance between the right and left lingual cortical plates measured along a line passing approximately through the center of the furcation of the maxillary first molars. The cementoenamel junction of the maxillary first molars was then identified by moving inferiorly through the axial slice until enamel was first evident, and intermolar width (IMW) was measured between the lingual grooves at the cementoenamel junction of the maxillary first molars ( Fig 2 ). To evaluate reliability, 20 scans were randomly selected, and the measurements were repeated.
Statistical analysis
Skewness and kurtosis showed normal distributions. The right and left sides were compared by using paired t tests. Sex differences were evaluated with Student t tests. Changes over time were analyzed by using single-sample t tests. Pearson correlations were used to relate the measures. The data were divided into 3 retention groups, including those whose quad-helices were left in place until phase 2, those retained with a Hawley, and those without retention before phase 2. Seven patients were not included in the retention groups because they had either a different type of retention or a combination of the retention strategies. The 3 groups were compared by using analysis of variance (ANOVA), with post-hoc Bonferroni tests. Intraexaminer reliability was evaluated by using paired t tests for systematic and method errors <SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='(∑d22n)’>(∑d22n−−−−√)(∑d22n)
( ∑ d 2 2 n )
for random error. Based on the observed effect sizes, post-hoc power analyses were conducted to determine the power of the study.
Results
Post-hoc power analysis showed greater than 95% power for all variables measured except buccal cortical plate thickness. Systematic intraexaminer reliability ranged between −0.130 and 0.125 mm; only the right-side difference for buccal bone thickness was statistically significant ( Table I ). Method error ranged between 0.11 and 0.37 mm.
| Systematic error | Random error | ||
|---|---|---|---|
| Mean (mm) | SEM | Method error (mm) | |
| BBT | |||
| Right | 0.105 | 0.047 ∗ | 0.16 |
| Left | −0.016 | 0.043 | 0.13 |
| LBT | |||
| Right | 0.005 | 0.121 | 0.37 |
| Left | −0.040 | 0.088 | 0.27 |
| ALW | |||
| Right | 0.125 | 0.103 | 0.33 |
| Left | 0.005 | 0.075 | 0.22 |
| BCPT | |||
| Right | 0.031 | 0.044 | 0.11 |
| Left | 0.075 | 0.046 | 0.12 |
| PW | −0.130 | 0.103 | 0.33 |
| IMW | 0.100 | 0.083 | 0.27 |
There were statistically significant differences between the right and left sides for buccal cortical plate thickness at T1 and for lingual bone thickness at T2. Age was not correlated with any measurements except alveolar width at T1 (r = .364 and .282 for the right and left sides, respectively). There were no statistically significant differences in age between the sexes at T1 or T2. The only statistically significant sex differences were the right and left alveolar widths at T1; the boys were 0.7 and 0.6 mm wider, respectively.
With the exception of buccal cortical plate thickness on the right side, all changes that occurred over time (ΔT1→T2) were statistically significant ( P <0.05). Before treatment, buccal bone thickness values were 2.2 and 2.1 mm on the right and left sides, respectively; buccal bone thickness decreased 1.6 mm ( Table II , Fig 3 ) between T1 and T2. At T2, approximately one third of the subjects showed little or no buccal bone on 1 side (n = 17) or both sides (n = 7) ( Fig 4 ); 2 patients had little or no buccal bone on 1 side at T1. Lingual bone thickness, which was 1.4 and 1.5 mm on the right and left sides, respectively, at T1, more than doubled in thickness (right, +1.5 mm; left, +1.7 mm). Alveolar width, which was 15.2 mm at T1, increased 0.5 mm. Buccal cortical plate thickness was 1.1 and 1.2 mm on the right and left sides, respectively, at T2, and decreased by 0.1 mm. Palatal width increased from 25.9 mm at T1 to 29.8 mm at T2. IMW increased by 6.5 mm.



