This case report describes the successful treatment of an adult patient with skeletal Class II open-bite malocclusion secondary to idiopathic condylar resorption. Total alloplastic joint reconstruction and counterclockwise rotation of the maxillomandibular complex combined with orthodontic treatment provided a satisfying outcome with maximum functional and esthetic improvement.
Idiopathic condylar resorption, also known as progressive condylar retrusion, is described as dysfunctional remodeling of the temporomandibular joint (TMJ) manifested by morphologic changes or resorption of the condyle. When this occurs in an adult, progressive resorption of the condyle results in a hyperdivergent skeletal Class II malocclusion. In addition to the skeletal changes, clinical signs and symptoms of idiopathic condylar resorption include reduction in masticatory performance, muscle and joint pain with function, limited range of motion, and occlusal and skeletal instabilities. Although the incidence in adults is rare, several authors have reported idiopathic condylar resorption and its association with orthodontics and orthognathic surgery.
The goals for managing idiopathic condylar resorption are to decrease pain, increase joint function, and prevent further joint damage and disability. As a general rule, the management of TMJ disease is to evaluate the patient’s response to noninvasive modalities before considering invasive surgical or salvaging procedures. However, for patients with advanced condylar resorption with evident changes in profile and occlusion, reconstruction therapy should also be considered. Here, we report the treatment process and its outcome of an adult with idiopathic condylar resorption who underwent total TMJ reconstruction.
Diagnosis and etiology
A 28-year-old woman was referred from the TMJ clinic at Gangnam Severance Dental Hospital in Seoul, Korea, for evaluation and treatment of her occlusion. She had complaints including difficulties in chewing, recent changes in profile, moderate joint pain in both TMJs, headache, and neck, muscle, and shoulder pain. She reported no parafunctional habits such as bruxism or clenching.
She had a history of previous orthodontic treatment for 4 years with maxillary first premolar extraction. Her chief complaint before her orthodontic treatment was lip protrusion. During and after the previous orthodontic treatment, she had experienced severe pain in both TMJ regions. Since the previous orthodontic treatment, she also experienced changes in her profile and difficulty in chewing.
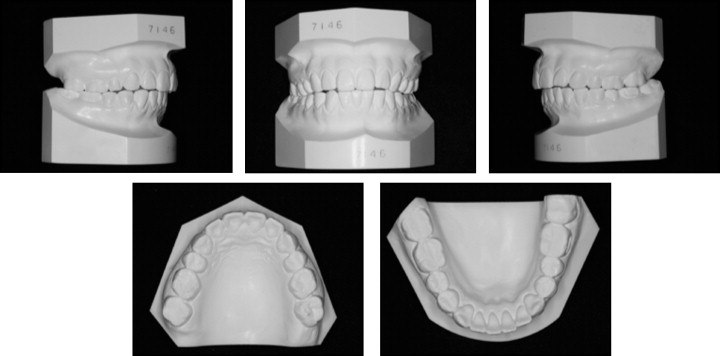
She had an obvious skeletal Class II profile with severe chin retrusion. Occlusal canting was also noted. An anterior open bite was present with Angle Class II molar and canine relationships. Her maxillary arch was slightly narrow with a crossbite tendency on the right. The mandibular midline was deviated to the left ( Figs 1 and 2 ).

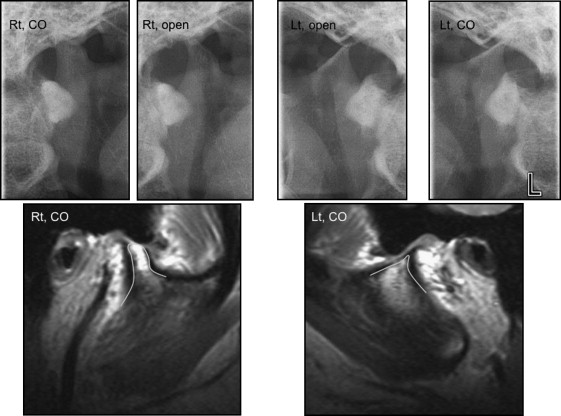
Evaluation of the panoramic radiograph and the TMJ tomograms showed severe condylar resorption. On the left side, there was complete resorption to the level of the sigmoid notch. Magnetic resonance imaging confirmed the complete resorption of the left side and also active resorption of the right condyle, presumably from the loss of cortical bone coverage ( Figs 3 and 4 ).
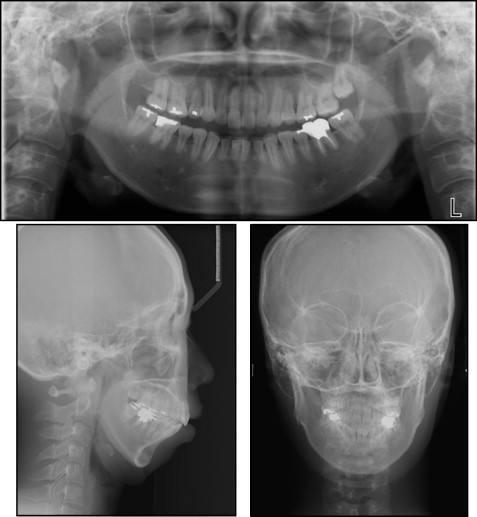
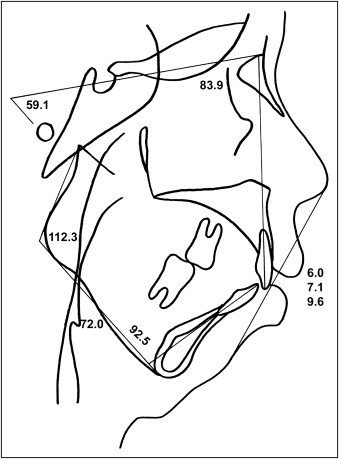
The cephalometric radiographs showed a significantly retruded mandible (SNB angle, 68°) compared with a relatively well-positioned maxilla (SNA angle, 80°), indicating a skeletal Class II malocclusion (ANB angle, 12°). A hyperdivergent profile was evident with a high mandibular plane angle (59°) and a facial height ratio of 50.0. The maxillary incisors were retroclined, possibly caused by the previous orthodontic treatment, which had been focused on camouflage of the skeletal Class II by extraction of the maxillary premolars ( Fig 5 , Table ).
| Variable | Norm | Pretreatment | Presurgery | Postsurgery | Posttreatment | Postretention |
|---|---|---|---|---|---|---|
| Skeletal | ||||||
| SNA (°) | 81.6 | 79.5 | 79.5 | 80.9 | 81.7 | 81.8 |
| SNB (°) | 79.1 | 67.0 | 69.0 | 75.2 | 76.3 | 75.6 |
| ANB (°) | 2.4 | 12.5 | 10.0 | 5.7 | 5.4 | 6.2 |
| FMA (°) | 24.0 | 50.7 | 47.6 | 37.0 | 37.2 | 37.4 |
| Gonial angle (°) | 118.6 | 112.3 | 123.6 | 130.1 | 125.1 | 125.7 |
| SN to MP (°) | 34.0 | 59.1 | 59.2 | 46.1 | 46.0 | 46.4 |
| Ramus height (mm) | 51.6 | 40.2 | 39.2 | 44.0 | 44.0 | 44.1 |
| Body length (mm) | 76.0 | 72 | 72.0 | 81.0 | 81.2 | 81.2 |
| Facial height ratio | 66.0 | 50.1 | 51.5 | 56.3 | 56.2 | 56.0 |
| Dental | ||||||
| U1 to SN (°) | 106.0 | 83.9 | 88.2 | 88.9 | 95.8 | 95.6 |
| IMPA (°) | 94.0 | 92.5 | 89.1 | 87.5 | 89.1 | 88.7 |
| Interincisal angle (°) | 126.0 | 124.5 | 122.6 | 127.8 | 127.5 | 129.3 |
| Occlusal plane (°) | 15.0 | 28.4 | 27.8 | 21.6 | 21.7 | 21.6 |
| Soft tissue | ||||||
| Upper lip to E-plane (mm) | −1.0 | 6.0 | 5.7 | 2.6 | −0.3 | 0.3 |
| Lower lip to E-plane (mm) | 1.0 | 9.6 | 10.0 | 6.1 | 1.3 | 2.4 |
We collected preorthodontic photos and a panoramic radiograph from the previous orthodontist. Although the patient had a poorly shaped condyle to begin with, it was evident that the etiology of the severe Class II hyperdivergent profile and recent changes in occlusion and profile were due to progressive condylar resorption during the 5-year postorthodontic period ( Fig 6 ).

Systemic diseases such as rheumatoid arthritis can also produce similar symptoms and degenerative changes in the TMJ. Therefore, a blood sample was evaluated for diagnostic markers of rheumatoid arthritis including rheumatoid factor. Since she had no other joint symptoms and the blood test was within normal limits, the possibility of rheumatoid arthritis was ruled out.
According to our evaluation of the orthodontic records and the patient’s history, she was diagnosed as skeletal Class II with idiopathic condylar resorption.
Treatment objectives
The treatment objectives were to (1) relieve joint pain and establish proper joint function, (2) correct the anterior open-bite malocclusion, and (3) improve facial esthetics.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


