Introduction
The purpose of this study was to investigate the influence of the timing of orthodontic force application on the rates of orthodontic tooth movement into surgical alveolar defects with bone grafts in beagle dogs.
Methods
Twelve beagles were randomly divided into 2 groups according to the surgical procedure: alveolar osteotomy alone (control) or osteotomy with bone graft (experimental group). The maxillary second premolars were protracted for 6 weeks into the surgical sites: immediately, at 2 weeks, and at 12 weeks after surgery. The orthodontic tooth movement rates and alveolar remodeling concomitant with surgical defect healing were evaluated by model measurements and histomorphometry as well as microcomputed tomography and histology. One-way analysis of variance and the Scheffé post hoc comparison were performed for investigating the rates of orthodontic tooth movement and mineralized bone formation.
Results
Both the orthodontic tooth movement rate and the mean appositional length of mineralized bone in the tension side of teeth were significantly accelerated when force was applied at 2 weeks in the control group and immediately in the experimental group ( P <0.001). The 2-week control group showed a dramatic increase in apposition rate during 4 to 6 weeks after force application, whereas the immediate protraction experimental group did within the first 3 weeks ( P <0.001). Decreased orthodontic tooth movement rates and reduced bone remodeling activities were apparent in the 12-weeks groups, especially in nongrafted defects.
Conclusions
A bone graft into the surgical defect can not only allow immediate force application for accelerating orthodontic tooth movement with favorable periodontal regeneration, but also decrease the risk of inhibited orthodontic tooth movement in case of delayed force application after surgery.
Accelerated tooth movement aided by alveolar surgery such as osteotomy, corticotomy, alveolar distraction, selective decortication, and minimally invasive cortical activation has been popularized in orthodontic practices to shorten treatment periods. Among these, alveolar segmental osteotomy as an intentional surgery is widely used for various purposes during orthodontic treatment. Its benefits are faster retraction or intrusion of target teeth followed by immediate esthetic improvement, and minimizing anatomic limitations that impede orthodontic tooth movement (OTM) such as poor bone quantity and quality associated with insufficient cancellous remodeling, poor periodontal support, already resorbed or short roots, and severely uprighted incisors surrounded by thin cortices. Moreover, it has the potential to provide a solution for more challenging patients with constricted alveolar ridge after extractions, alveolar defects caused by trauma, or alveolar cleft, if combined with bone graft procedures.
As bone graft materials and techniques have been innovated in tissue engineering, accelerating tooth movement into the alveolar osteotomy site can be ensured in practice with healthy defect regeneration. A few studies have tried OTM into a bone defect area with bone grafts but they focused on defect regeneration, graft stability, and any side effects around the moved teeth or the periodontium. There was no investigation on the rate of OTM in relation to the graft characteristics or orthodontic force characteristics. Inconsistent experimental setups among studies, especially regarding protocols of orthodontic force application, made it difficult to obtain guidelines for clinical applications.
An osteotomy or a bone graft cannot guarantee accelerated tooth movement. Immediately after segmental surgeries, OTM toward the surgical defect can be accelerated because of less tissue resistance associated with the regional acceleratory phenomenon. However, the accelerated rate decreases over time along with disappearance of the regional acceleratory phenomenon, and OTM into the surgical site might be inhibited if the postoperative orthodontic adjustment was not performed properly. To maximize the effects of accelerated tooth movement aided by alveolar surgery, a standardized protocol for postsurgical orthodontic intervention should be established based on the healing progression of surgical sites with or without a graft.
The aim of this study was to investigate the effect of the timing of orthodontic force application after surgery on the rates of OTM into surgical alveolar defects with bone grafts, considering the healing state of the surgical sites in beagle dogs.
Material and methods
Twelve male beagles aged 18 to 24 months and weighing 10 to 13 kg were used for the experiments. They were randomly divided into 2 groups according to the surgical procedure: alveolar osteotomy alone (O, control group; n = 6) and osteotomy with bone graft (OG, experimental group; n = 6). Each group was further divided into 3 subgroups (n = 2) based on the timing of orthodontic force application: immediately (OG-0 and O-0), 2 weeks after surgery (OG-2 and O-2), and 12 weeks after surgery (OG-12 and O-12). The experimental protocols for each group were approved by the ethics committee on animal research of Kyung Hee University (KHMC-IACUC 11-007), Seoul, Korea, before the study.
The maxillary first premolars were extracted under general anesthesia by intramuscular injection of Zoletil 50 (0.25 mg/kg; Virbac Laboratory, Carros, France), and 4-walled critical size defects of approximately 5 mm (mesiodistal) × 5 mm (buccolingual) × 7 mm (vertical), including the extraction socket, were generated using a 2.0-mm round bur ( Fig 1 , A ). The distal wall of each defect was approximately 1.5 mm mesial from the mesial root of the maxillary second premolars to prevent immediate fracture of the interseptal wall. In the osteotomy with bone graft groups, the defect was immediately filled with a 1:1 mixture of deproteinized bovine bone mineral (Bio-Oss; Geistlich Sons, Wolhusen, Switzerland) and demineralized bone matrix (OrthoBlast II; IsoTis, Irvine, Calif). The particles were mixed with saline solution and carefully packed to fill the bone defect ( Fig 1 , B ). The mucosa was adjusted to allow full coverage of the surgical defect and subsequently sutured. After surgery, antibiotics (Gentamycin; Komipharm International Co, Shiheung, Korea) and anti-inflammatory analgesics (Ketopro; Uni Biotech Co, Chungnam, Korea) were administered via intramuscular injection twice daily for 6 days, and a 0.12% chlorhexidine gluconate solution dressing was applied simultaneously.
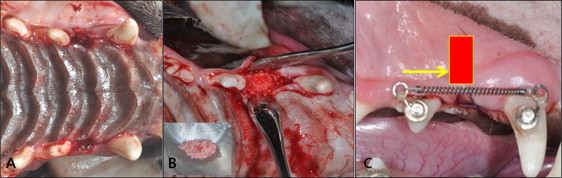
Orthodontic buttons (Ormco, Milwaukee, Wis) were bonded onto the labial surfaces of the maxillary canines (anchorage teeth) and the second premolars (target teeth) with Superbond C&B (Sun Medical, Shiga, Japan). To apply the force close to the center of resistance, an extension hook was connected to the orthodontic buttons. The second premolars were protracted mesially by a nickel-titanium closed-coil spring (light force; 3M Unitek, Monrovia, Calif) between the canine and the second premolar, exerting a force of approximately 100 g per side ( Fig 1 , C ). OTM was continued for 6 weeks in all groups. Oral hygiene, condition of the appliance, and force magnitude were checked once a week. Six weeks after appliance placement, the animals were killed by direct injection of Zoletil 50 (50 mg/kg) into the heart. Tissue blocks including the maxillary second premolar, the surgical defect, and the canine were harvested and immediately fixed and stored in 10% formalin for 48 hours.
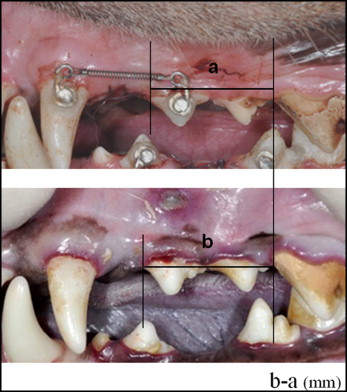
OTM was measured using precisely fabricated stone models (GC Europe, Leuven, Belgium) through alginate impressions (GC, Tokyo, Japan) recorded every week for 6 weeks. The distance from the mesial cervix of the second premolar to the mesial cervix of the first molar was measured using a digital caliper (Hangzhou Maxwell Tools, Hangzhou, China) at each time point ( Fig 2 ). All measurements were repeated after 2 weeks by 2 investigators (H.-W.A. and another), and the average of the 2 measurements was used.
Microcomputed tomography was used to evaluate the pattern of OTM and the defect healing state descriptively with SkyScan 1173 (Bruker-microCT, Kontich, Belgium). This information assisted the determination of the direction of tissue sections for histology. The region of interest was restricted to 3.5 × 2.8 × 2.5 mm to limit the area to the core and newly formed bone underlying the defect. Images were obtained with settings of 130 kVp source voltage, current of 30 μA, and an image pixel size of 44.7 μm. Microstructural parameters such as bone mineral density, percent bone volume, trabecular thickness, and trabecular number were directly calculated from the 2-dimensional and 3-dimensional data sets (version 1.12.0.0, CT Analyser; Bruker-microCT).
Half of the blocks was decalcified with 10% ethylenediaminetetraacetic acid (EDTA-2Na, pH 7.4) at 48°C for 30 days and dehydrated in ethyl alcohol of gradually increasing concentrations from 70% to 100%. After paraffin embedding, the samples were sectioned sagittally to a thickness of 6 μm. They were stained with hematoxylin and eosin and Masson’s trichrome stain and examined under a light microscope for evaluation of alveolar bone surrounding the moved tooth and the surgical defect. The other half of the blocks was prepared as nondecalcified specimens for histomorphometric analysis.
All dogs were injected intramuscularly with oxytetracycline hydrochloride (yellow orange, 30 mg/kg; Sigma-Aldrich Co, St Louis, Mo) at 24 hours before OTM, alizarin red (red, 30 mg/kg; Sigma-Aldrich) at 3 weeks after force application, and calcein (green, 10 mg/kg; Sigma-Aldrich) at 6 weeks after OTM (24 hours before the dogs were killed) to label the newly formed mineralized bone on the tension side of the moved teeth. Nondecalcified specimens were examined under an ultraviolet fluorescent microscope (BH-2; Olympus, Tokyo, Japan) with an ultraviolet filter (515 nm). Microphotographs were obtained using a digital charge-coupled device camera (PS30C; Kappa, Gleichen, Germany). Along the outline of the labeled bone traced from the microphotographs, 10 sites were randomly selected for linear measurements of newly formed bone, and the mean of these 10 values was used (Metreo version 2.5; Kappa).
Statistical analysis
Comparisons of the second measurements with the first ones for each variable were performed using the Pearson correlation coefficient, which was above 0.98 at the 95% confidence level. Therefore, the mean of 2 data sets was used for further description. Normality of the data distribution of the accumulated distance of OTM and the amount of new bone deposition at the tension side were confirmed using the Shapiro-Wilks test. For intergroup comparison between the 6 subgroups, 1-way analysis of variance and the Scheffé post hoc comparison were performed. A P value <0.05 was considered to indicate a statistically significant difference.
Results
All sites healed uneventfully after the surgical procedures, and 2 beagles showed a weight loss (<1 kg) during the experiment.
The cumulative amount of OTM after 6 weeks ranged from 1.75 to 3.44 mm in the grafted groups and from 1.18 to 3.51 mm in the nongrafted groups. The highest OTM rate was observed in the OG-0 and O-2 groups ( P <0.001, Fig 3 , Table I ). During earlier stages (1-3 weeks after force application), the OG-0 group showed more OTM than did the O-2 group. The OG-2 and O-0 groups had similar OTM rates (2.42 and 2.30 mm, respectively). After a 12-week healing period, OTM slowed rapidly in both grafted and nongrafted groups ( P <0.001). However, as time elapsed, the gap between the OG-12 and O-12 groups gradually increased ( P <0.001; 1.75 and 1.18 mm, respectively).
| Number | Group | 1 wk | 2 wk | 3 wk | 4 wk | 5 wk | 6 wk (total) | P value Multiple comparisons |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| 1 | O-0 | 1.04 | 0.10 | 1.33 | 0.06 | 1.71 | 0.08 | 2.00 | 0.05 | 2.08 | 0.07 | 2.30 | 0.07 | |
| 2 | O-2 | 1.04 | 0.05 | 1.74 | 0.06 | 2.32 | 0.19 | 2.87 | 0.35 | 3.17 | 0.21 | 3.51 | 0.07 | 0.0000 ∗ |
| 3 | O-12 | 0.35 | 0.08 | 0.61 | 0.10 | 0.80 | 0.06 | 0.89 | 0.03 | 0.99 | 0.04 | 1.18 | 0.04 | (2, 4) > (5, 1) > 6 > 3 |
| 4 | OG-0 | 1.04 | 0.15 | 2.05 | 0.10 | 2.55 | 0.07 | 2.93 | 0.12 | 3.14 | 0.11 | 3.44 | 0.07 | |
| 5 | OG-2 | 0.80 | 0.12 | 1.39 | 0.09 | 1.82 | 0.10 | 1.91 | 0.11 | 2.15 | 0.18 | 2.42 | 0.14 | |
| 6 | OG-12 | 0.40 | 0.13 | 0.63 | 0.12 | 1.01 | 0.13 | 1.11 | 0.15 | 1.48 | 0.13 | 1.75 | 0.09 | |
Microcomputed tomography images of the surgical defect and the target tooth are shown in Figure 4 . All subgroups except O-12 showed the tendency of bodily movement of the premolar. However, group O-12 demonstrated a bony discontinuity and insufficient vertical bone support that induced rotational tooth movement rather than mesialization of the premolar. Of the grafted groups, even OG-12 showed good healing of the surgical defect, although the repair of vertical bone height was not sufficient compared with the others. Microstructural parameters indicated the characteristic bone maturation state of the surgical defect in each group. Bone mineral density increased in proportion to the healing time. The grafted groups showed greater bone mineral density than did the nongrafted groups at every time point and also the percent bone volume. The percent bone volume was lowest at 12 weeks (21.24% in O-12 and 46.24% in OG-12) and highest at 2 weeks (53.64% in O-2 and 75.18% in OG-2) in both groups. The lowest trabecular thickness values were 0.18 mm in the nongrafted group (O-2) and 0.14 mm in the grafted group (OG-0). The thickest trabeculae were found at 12 weeks in both the grafted and nongrafted groups (0.66 and 0.55 mm, respectively). The highest trabecular number was 2.40 mm −1 in the grafted group (OG-0), and it decreased as time passed. Of the nongrafted groups, the O-2 group showed higher trabecular numbers than did the O-0 group (2.39 vs 1.35 mm −1 ).
Light microscopy findings of the surgical defects are shown in Figures 5 and 6 . Of the nongrafted groups, O-2 showed good healing of the surgical defect by active new bone formation that maintained the vertical alveolar bone height. However, group O-12 demonstrated a wide surgical gap and discontinuity of alveolar bone. Bone formation was limited in the neighboring teeth. In grafted groups, even OG-12, the vertical alveolar bone volume was well maintained, and new bone formation was greater than that in the nongrafted groups. This newly formed bone contained multiple developed marrow spaces and exhibited compact trabecular bone that was easily distinguishable from the old lamellar bone. The bone contour of the surgical defects showed a convex profile toward the gingiva in the OG-0 and OG-2 groups compared with their nongrafted counterparts.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


