Introduction
The purpose of this study was to evaluate long-term skeletal and occlusal stability after bimaxillary surgery to correct skeletal Class III malocclusion.
Methods
The sample comprised 81 consecutively treated patients. All subjects had received a combined 1-piece LeFort I and bilateral sagittal split ostotomies with rigid fixation between 1990 and 2003 and were followed for 3 years. Lateral cephalograms were obtained before surgery and at 5 occasions after surgery.
Results
The mean setback was 6.9 mm in the mandible, and the maxilla was moved forward 3.7 mm. In most patients, the posterior maxilla was impacted. Relapse of maxillary advancement was insignificant (0.1 mm), whereas relapse at B-point was on average 1.7 mm ( P <0.010). After 3 years, mean overjet and overbite amounts were 2.0 and 1.9 mm, respectively. Skeletal relapse of the mandible increased significantly with the surgical setback ( P <0.001) and the change in the vertical position of the posterior maxilla ( P = 0.010) (multivariate regression analysis).
Conclusions
Bimaxillary surgery resulted in good occlusal stability. Maxillary advancement was stable, whereas relapse of the mandibular setback varied. Risk factors for horizontal relapse of the mandible were large setback and inferior repositioning of the posterior maxilla.
Skeletal Class III malocclusion is reported to be the most frequent anomaly corrected by combined orthognathic surgery and orthodontic treatment. Historically, Class III malocclusions have been treated by isolated mandibular setback, but recent reports indicate that bimaxillary procedures have become more frequent. Many studies on stability after 1-jaw surgery are available, and it has been questioned whether the findings are relevant for bimaxillary procedures.
Because a Class III malocclusion is often combined with a vertical discrepancy, the nature of the anomaly along with requirements for facial harmony give directions for surgical repositioning. It has been indicated that vertical changes can affect the amount of mandibular relapse. Although the use of bimaxillary procedures is apparently widespread, relatively few reports based on substantial and homogeneous samples are available, and only a few studies address stability after vertical changes in jaw position.
The purpose of the present study was to analyze skeletal and occlusal stability 3 years after bimaxillar surgery of skeletal Class III malocclusion to (1) examine the amount, direction, and timescale of postoperative changes; (2) examine the proportion of patients with clinically significant skeletal (≥2 mm) and occlusal relapse; and (3) analyze potential factors influencing skeletal stability (sex, age at surgery, presurgery morphology, direction, and amount of surgical repositioning).
Material and methods
The sample comprised 81 consecutively operated patients (55 male, 26 female) who had combined 1-piece LeFort I and bilateral sagittal split osteotomies with rigid fixation. None had undergone additional surgery (eg, genioplasty). The patients were selected from the files at the Department of Orthodontics of the University of Oslo in Norway. Surgery had been performed at the Ullevaal University Hospital in Oslo from 1990 through 2003. Before treatment, all patients were seen by Oslo University’s orthognathic team for evaluation and treatment planning, and all had been followed at the Department of Orthodontics over a 3-year period. Patients with syndromes, cleft of the lip or palate, or dentofacial trauma were excluded from the study. The ages at the surgery varied from 16.2 to 52.2 years (mean, 25.8 years; SD, 9.5 years). Records were collected 1 week before surgery (T1), within 1 week after surgery (T2), and at 4 follow-up reviews: 2 months (T3), 6 months (T4), 1 year (T5), and 3 years (T6). For a patient to be included in the study, in addition to cephalograms obtained at T1, T2, and T6, at least 2 other postoperative cephalograms of adequate quality had to be available.
Presurgical and postsurgical orthodontic treatment was carried out by specialist orthodontists in their practices or postgraduate students under supervision. Detailed information about duration of orthodontic treatment was not collected. However, at the postoperative follow-up, all but 1 patient had orthodontic appliances 2 months postoperatively, and 39 and 8 subjects had appliances 6 and 12 months after surgery, respectively. This indicates that the postoperative orthodontic treatment durations were comparable with the median of 5.9 months in a previous study of patients monitored by the same team.
A team of 5 senior surgeons was involved in performing the surgery. For all patients, a standard 1-piece Le Fort I osteotomy was performed. Reference marks were made on the lateral aspects of the maxilla before making the osteotomies. After mobilization, the maxilla was moved to its planned position by using the reference marks as guides. Fixation was achieved by using 4 L-shaped miniplates on each side of the maxilla. The plating system (Walter Lorentz Co., Jacksonville, Fla.) consisted of 1.0-mm plates, and 4 screws (diameter, 2.0 mm) were used for each plate, 2 above and 2 below the surgical cut. After the maxilla had been stabilized, the mandibular sagittal split osteotomies were performed. The teeth were placed in their planned occlusion and stabilized with maxillomandibular fixation with or without an interocclusal splint, depending on the stability of the occlusion. The bony segments were stabilized by using 3 bicortical lag screws (2.0 mm) with biconcave washers (Krenkel, Normed Medizin-Technik GMBH, Tuttlingen, Germany), which were placed in the gonial area through a transcutaneous approach. After completion of mandibular skeletal stabilization, the maxillomandibular fixation was released.
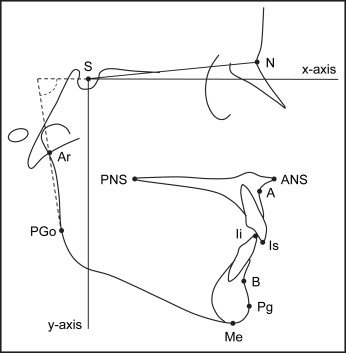
The same cephalostat was used for all radiographs, and the cephalograms were taken with the head in a standardized position with the teeth in occlusion and the lips relaxed. All cephalograms were hand-traced by the same examiner (G.J.) on acetate paper. The cephalogram of the best quality was traced first, and then tracings of the other radiographs were superimposed on sella, nasion, and the anterior and posterior cranial bases by using the best-fit method. From the same radiograph, a template of the outline of the maxilla was constructed and superimposed on the presurgical radiograph on the outline of the bony palatal structures. This method of anatomic best fit was used to account for surgical alteration of the anterior nasal spine. The tracings were scanned and digitized with Dentofacial Planner Plus software (Dentofacial Software, Toronto, Ontario, Canada) on a computer with a digitizing screen (Numonics, Montgomeryville, Pa). The measurements were not corrected for magnification (5.6%). If the interocclusal splint was in place in the immediate postoperative radiograph, a template of the mandible was constructed on acetate paper and autorotated to incisor contact. Changes in landmark position during the various time intervals were recorded with a coordinate system. A line through sella, rotated 7° from the nasion-sella line, was used as the horizontal reference line (x-axis). The line approximated the Frankfort horizontal plane. The y-axis was perpendicular to the x-axis and passed through sella ( Fig 1 ). The definitions of landmarks and measurements have been presented previously.
Statistical analysis
For analysis of the method errors, 20 radiographs, chosen at random, were traced and digitized by the same investigator on 2 separate occasions at least 2 weeks apart. Statistical analyses were performed with SPSS for Windows software (SPSS, Chicago, Ill). Paired t tests were used to analyze changes over time in the cephalometric variables. Significance was tested only for comparisons between T1 and T2 (changes during surgery) and between T2 and T6 (total relapse) to avoid multiple significance testing. Associations between variables were analyzed by Pearson correlation coefficients, and multivariate linear regression analysis was used to identify factors with possible influences on postoperative horizontal relapse of the mandible. The following 26 variables were analyzed as possible predictors for postoperative horizontal relapse of the mandible measured at B-point: (1) demographic characteristics: sex and age at operation; (2) presurgery morphology (T1): SNA, SNB, ANB, A to NP, Pg to NP, NL/NSL, ML/NSL, overjet, and overbite; (3) surgical changes (T1 to T2): SNA, SNB, ANB, NL/NSL, ML/NSL, horizontal position of A, horizontal position of B, vertical position of ANS, vertical position of PNS, vertical position of menton, overjet, overbite, and ramus inclination; and (4) postsurgery morphology (T2): overjet and overbite.
Results
The method errors ranged from 0.33 to 0.61 mm for linear measurements and from 0.40° to 1.22° for angular measurements. The difference between duplicate measurements for no variable was significant at the 10% level. Cephalometric variables describing presurgical cranial and dentofacial morphology of the sample are summarized in Table I . Of these skeletal Class III patients, 56 had an anterior open bite.
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| SNA (°) | 79.6 | 3.6 | 70.5 | 85.7 |
| SNB (°) | 84.7 | 5.5 | 70.2 | 100.3 |
| ANB (°) | −5.1 | 4.1 | −15.1 | 4.8 |
| A to NP (mm) | −1.8 | 4.5 | −14.5 | 8.1 |
| Pg to NP (mm) | 9.7 | 10.1 | −16.2 | 33.6 |
| NL/NSL (°) | 8.5 | 4.4 | −4.9 | 21.5 |
| ML/NSL (°) | 35.8 | 7.7 | 16.9 | 54.2 |
| Overjet (mm) | −7.0 | 5.0 | −18.9 | 3.2 |
| Overbite (mm) | −1.8 | 3.8 | −9.7 | 6.4 |
Mean changes in the cephalometric variables as a result of surgery and during the observation period are presented in Table II . During surgery (T1-T2), the maxilla was on average moved forward 3.7 mm at A-point ( P <0.001), with a range from 1.8 mm in the posterior direction to 9.8 mm in the anterior direction. On average, the posterior part of the maxilla was moved up (1.7 mm at PNS, P <0.001), whereas the anterior maxilla was moved slightly down (0.7 mm at ANS). The mean surgical movement of the mandible was 6.9 mm backward measured at B-point ( P <0.001) (range, –18.3-5.1 mm). During surgery, there was a mean increase in ramus inclination of 3.4° ( P <0.001), indicating backward movement of the proximal segment. Overjet and overbite increased on average 9.8 and 3.7 mm, respectively ( P <0.001).
| T1 to T2 | T2 to T3 | T3 to T4 | T4 to T5 | T5 to T6 | T2 to T6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 81 | n = 78 | n = 75 | n = 76 | n = 80 | n = 81 | |||||||
| Horizontal changes (mm) | ||||||||||||
| A | 3.7 † | (2.5) | −0.1 | (0.9) | 0.0 | (0.7) | 0.0 | (0.6) | 0.0 | (0.7) | −0.1 | (1.0) |
| B | −6.9 † | (5.5) | 0.8 | (1.8) | 0.3 | (1.1) | 0.1 | (1.0) | 0.5 | (1.0) | 1.7 † | (2.2) |
| Pg | −6.6 † | (7.0) | 1.0 | (1.9) | 0.6 | (1.2) | 0.1 | (1.2) | 0.5 | (1.2) | 2.2 † | (2.5) |
| Is | 2.9 † | (3.6) | 0.6 | (1.2) | 0.1 | (1.1) | −0.1 | (0.9) | 0.1 | (1.1) | 0.7∗ | (1.9) |
| Ii | −7.1 † | (4.1) | 0.9 | (1.4) | 0.2 | (1.2) | 0.1 | (1.3) | 0.4 | (1.0) | 1.5 † | (1.8) |
| Overjet | 9.8 † | (4.6) | −0.3 | (1.4) | −0.2 | (1.2) | −0.1 | (0.9) | −0.2 | (1.2) | −0.8∗ | (2.0) |
| Vertical changes (mm) | ||||||||||||
| ANS | 0.7 | (3.5) | −0.5 | (1.3) | −0.2 | (0.9) | 0.0 | (0.9) | −0.1 | (1.0) | −0.7 † | (1.7) |
| PNS | −1.7 † | (3.0) | −0.1 | (0.8) | 0.1 | (0.9) | 0.1 | (0.7) | 0.1 | (0.7) | 0.2 | (1.1) |
| Me | −1.7∗ | (5.0) | −0.7 | (1.4) | −0.3 | (1.4) | 0.0 | (0.8) | 0.2 | (1.2) | −0.8∗ | (2.6) |
| Is | 1.2∗ | (3.8) | −0.6 | (1.4) | −0.3 | (1.0) | 0.0 | (0.7) | −0.2 | (0.9) | −1.1 † | (2.0) |
| Ii | −1.8∗ | (5.3) | −1.3 | (1.7) | −0.2 | (1.3) | 0.2 | (0.8) | 0.1 | (1.2) | −1.1 † | (2.6) |
| Overbite | 3.7 † | (3.5) | 0.6 | (1.4) | −0.1 | (1.1) | −0.2 | (0.8) | −0.3 | (0.9) | 0.0 | (1.7) |
| Angular changes (°) | ||||||||||||
| SNA | 3.3 † | (2.1) | −0.1 | (0.6) | 0.1 | (0.5) | −0.1 | (0.5) | 0.0 | (0.8) | −0.1 | (0.9) |
| SNB | −4.0 † | (3.0) | 0.5 | (1.0) | 0.2 | (0.6) | 0.1 | (0.5) | 0.2 | (0.6) | 1.0 † | (1.2) |
| ANB | 7.3 † | (3.4) | −0.6 | (0.9) | −0.1 | (0.6) | −0.2 | (0.6) | −0.2 | (0.7) | −1.0 † | (1.2) |
| NL/NSL | 2.7 † | (4.2) | −0.4 | (1.5) | −0.2 | (1.0) | −0.1 | (1.0) | −0.2 | (0.9) | −0.9 † | (1.9) |
| ML/NSL | −0.5 | (5.6) | −0.2 | (1.7) | −0.1 | (1.6) | 0.2 | (1.1) | 0.2 | (1.2) | 0.0 | (2.3) |
| Ramus inclination | 3.4 † | (4.3) | −0.5 | (2.1) | −0.3 | (1.9) | 0.0 | (1.6) | −0.2 | (1.4) | −0.9 † | (2.0) |
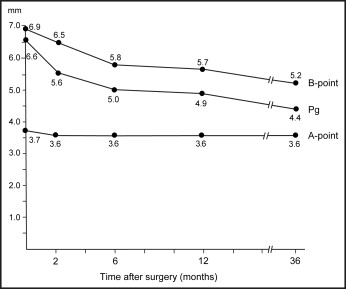
During the 3-year follow-up period (T2-T6), the mean horizontal change at A-point (0.1 mm) and the vertical change at PNS (0.2 mm) were not significant. ANS moved on average up 0.7 mm ( P <0.001). The horizontal change at B-point (T2-T6) was 1.7 mm in the anterior direction ( P <0.001), representing a 25% relapse of the surgical movement. The greatest relapse observed was 6.6 mm in a patient with a setback of 10.5 mm. The ramus inclination decreased by 0.9° ( P <0.001), and this relapse was significantly correlated with the horizontal relapse at B-point (r = 0.432, P <0.001). Overbite remained on average unchanged, and overjet decreased less than 1 mm (0.8 mm, P <0.01). After 3 years, the mean amounts of overjet and overbite were 2.0 and 1.9 mm, respectively. Two subjects had a negative overjet (2 and 6 mm). Open bite, observed in 8 subjects, was less than 1 mm in 5 of them.
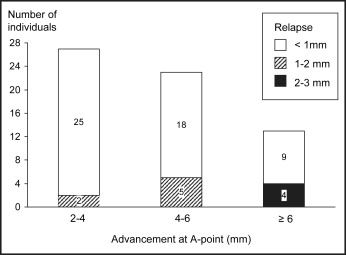
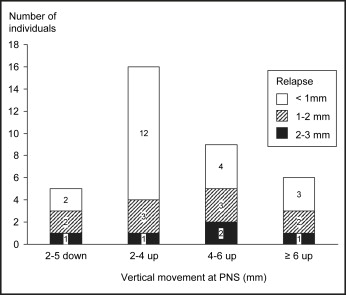
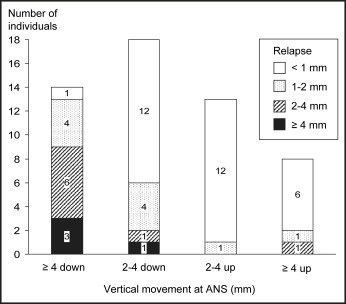
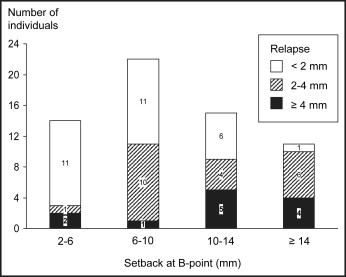
The amount of relapse was significantly ( P <0.01) correlated with the amount of surgical repositioning: the Pearson correlation coefficients were –0.386, –0.342, –0.613, and –0.499 for A-point, PNS, ANS, and B-point, respectively. The distribution of subjects with various amounts of relapse related to the magnitude of surgical movement is presented in Figures 2 through 5 for those with ≥2 mm repositioning of the maxillary and mandibular landmarks (A-point, PNS, ANS, and B-point). Relapse of 2 mm or more always occurred in the opposite direction of the surgical movement. Of the 63 subjects with ≥2 mm advancement of the maxilla, 83% had less than 1 mm of relapse ( Fig 2 ). A relapse of more than 2 mm was observed in only 4 subjects, and none relapsed more than 3 mm at A-point. In the 31 patients with ≥2 mm impaction of the posterior maxilla (PNS), 4 (13%) had relapse of 2 to 3 mm, and the other 27 had relapse less than 2 mm ( Fig 3 ). Figure 4 illustrates that impaction of the anterior maxilla (ANS) remained stable in most of the 21 subjects with impaction ≥2 mm. In 32 subjects, ANS was moved down ≥2 mm during surgery, and relapse of more than 2 mm occurred in 11 (34%) of them. In the subgroup with ≥4 mm of downward movement during surgery, 9 of the 14 patients (64%) had a relapse of ≥2 mm, and the greatest relapse observed was 6.4 mm. The mandible was moved back ≥2 mm (B-point) in 62 of the 81 subjects ( Fig 5 ). Among the 26 subjects with a setback of ≥10 mm, a relapse of 4 mm or more was observed in 9 (35%). In comparison, surgical movement of less than 10 mm resulted in a relapse of 4 mm or more in 3 (8%) of 36 subjects.
Most of the relapse occurred during the first 6 months after surgery ( Fig 6 ). A somewhat greater relapse occurred at pogonion compared with B-point. Figure 6 also illustrates the changes in horizontal relationship between the maxillary and mandibular skeletal components over the 3-year period.
Of the 26 variables included in the regression analysis, 16 were significantly associated with horizontal relapse of the mandible at B-point (Pearson correlation coefficient, P <0.05) ( Table III ). Because of strong intercorrelations, 8 variables were excluded from the multivariate regression analysis. Thus, the remaining 8 variables were included in the regression model with forward variable selection (presurgical morphology: Pg to NP, ML/NSL, overjet; surgical change: horizontal position of B, vertical position of ANS, PNS, and Me, and ramus inclination). In the final model, only 2 variables were included: horizontal change at B-point ( P <0.001) and vertical change at PNS during surgery ( P = 0.010). This model explained 31% of the variation in the horizontal relapse of the mandible. Table IV shows that the mean relapse increased 0.2 mm for each millimeter that the mandible was moved back and the posterior maxilla was moved down during surgery. This implies that increased stability of the mandible was obtained when the setback was limited and the posterior maxilla was impacted. Figure 7 suggests a linear association between the amount of horizontal relapse at B-point and the amount of setback during surgery.



