Introduction
The influence of the forces exerted by the perioral musculature on the position of the teeth has been the object of many scientific studies. Of the forces from the soft tissues, those from the tissues in the passive resting state are believed to be more important than forces exerted on the teeth during various functions such as speech and swallowing. The aims of this study were to measure upper lip pressure at rest and during swallowing in 2 groups of patients with different occlusions and to evaluate any differences among the groups.
Methods
Fifty subjects were divided into 2 groups according to occlusal and skeletal patterns: Class I and Class II. Both groups were divided into 2 subgroups according to age: young patients (9-17 years) and adult patients (18-35 years). A force-sensing resistor device (Datalog, Flexiforce low type, Biometrics Ltd, Gwent, United Kingdom) with a transducer thickness of less of 1 mm was used for the measurements. The sensor was positioned on the midline between the maxillary incisors with a thin layer of soft wax. Labial pressure measurements were made with the lips at rest and during swallowing saliva.
Results
The average resting lip pressure was 24.59 ± 2.55 g/cm 2 ; during swallowing, the mean pressure was 24.87 ± 2.45 g/cm 2 . No significant difference was found between lip pressure at rest and at function or between the two groups with different occlusions and skeletal patterns. There was a significant correlation between lip pressure and age.
Conclusions
In healthy patients, (1) upper lip pressure does not change at rest and during swallowing, (2) upper lip pressure was similar in the 2 groups (Class I, 24.33 g/cm 2 ; Class II, 24.61 g/cm 2 ), and (3) lip pressure was higher in adults than in young subjects. Further studies are needed to measure the pressure of the lower lip and to evaluate whether there are differences in labial pressure between subjects with labial competence and incompetence.
The influence of the forces exerted by the perioral musculature on the position of the teeth has been the object of several scientific studies. The force plays a role in guiding tooth eruption and maintaining dental arch form and stability. Most authors accept, as a basis, the equilibrium theory of tooth position. The lips, cheeks, and tongue are the most important environmental determinants of tooth position. The forces from the tongue have consistentely been found to be greater than those from the lips. However, the teeth are in an equilibrium position because the forces are equal on them over time from all directions, regardless of the strength of the muscle that is applying the force.
Of the forces from the soft tissues, those from the tissues in the passive resting state are believed to be more important than forces exerted on the teeth during various functions such as speech and swallowing. Forces that act on incisors during function are of short duration, but it has been postulated that forces operating longer than 4 to 6 hours per day can produce movements in a relatively short time. The question is raised: is there any difference between resting lip pressure and dynamic labial pressure?
The main function of the lips, oral competence, is controlled by the orbicularis oris muscle. The orbicularis oris muscle is a concentric, sphincter-like muscle around the mouth that closes, withdraws, and protrudes lips. Its action is analogous to the orbicularis oculi around the eye. The main function of the lips during swallowing is to maintain oral competence. Briefly, the upper lip closing movement is performed by the orbicularis oris muscle, and the lower lip closing movement is performed by the mentalis and orbicularis oris muscle.
In some patients with maxillary protrusion or severe Class II Division 1 malocclusion, lip incompetency and muscle imbalance are observed. Posen described a device for measuring the strength of the lips called the pommeter (perioral muscle meter). He found that the subjects with bimaxillary protrusion had low lip strength, compared with Class I and Class II Division 2 patients. Posen reached that conclusion with the pommeter, which is different from the force-sensing resistor sensors that we used in this study.
The question is whether there are any differences in labial pressure among subjects with different occlusions. The aims of this study were to measure upper lip pressure at rest and during swallowing in 2 groups of patients with different occlusions and to evaluate any differences among the groups.
Material and methods
Fifty subjects were divided into 2 groups according to occlusal and skeletal patterns: group 1, 25 patients (9 male, 16 female) with Class I skeletal pattern and Class I occlusal relationship, and group 2, 25 patients (12 male, 13 female) with Class II skeletal pattern and Class II Division 1 or Division 2 dental pattern. Subjects with increased overjet (>7 mm) were excluded. The groups were further divided into 2 subgroups according to age: subgroup A, young patients aged 9 to 17 years (mean age, 13 years), and subgroup B, adults aged 18 to 35 years (median age, 27.5 years).
To evaluate the occlusal and skeletal patterns of each subject, the usual orthodontic documentations, including extraoral and intraoral photos, dental casts, and profile x-ray cephalograms, were made. All landmarks were identified and digitized by 1 investigator using Dolphin Imaging Software (version 10.5, Dolphin, Imaging and Management Solutions, Chatsworth, CA, USA). McLaughlin’s cephalometric analysis was chosen for this purpose.
The inclusion criteria were no permanent teeth lost; no missing or supernumerary teeth; no history of orthognathic surgery or previous orthodontic treatment; no congenital craniofacial anomalies; no occlusal canting or other asymmetric skeletal patterns; no Class III skeletal and dental pattern; no overjet greater than 7 mm; no labial incompetence, oral breathing, and sucking habits; no hypodivergent or hyperdivergent patients; no patients whose upper lip and maxillary incisors were not in the correct positions for the sensor; and no patients in treatment with drugs influencing the tone of the muscles.
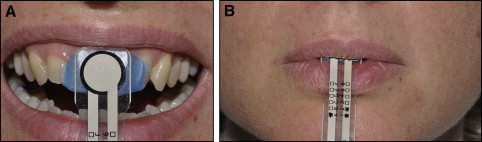
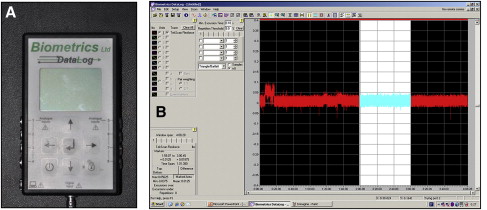
A force-sensing resistor device (Datalog, Flexiforce low type, Biometrics Ltd, Gwent, United Kingdom) with a transducer thickness of less of 1 mm was used for the measurements. The sensor was 20 cm long, 3 cm wide, and ultraflexible so that it was comfortable in the mouth ( Fig 1 ). It was reliable for a wide range of temperatures: –28°C to 216°C, including the mouth’s temperature (37°C); this allowed minimized temperature-induced errors. The sensor was positioned on the midline between the maxillary incisors with a thin layer of soft wax about 0.5 mm thick. A data logger (Biometrics Datalog II of NexGen Ergonomics, Units 25 and 26, Biometrics) ( Fig. 2, A ) and DataLog Display and Analysis Software ( Fig 2 , B ) were used for data acquisition.
Lip pressure measurements were made with the lips at rest and during swallowing saliva. The measurements were performed 3 times for 4 minutes each, at 5-minute intervals. During recording, each subject was asked to swallow at minutes 1, 2, 3, and 4. All measurements were made by the same operator (D.D.).
To achieve natural head position, the subjects were seated in front of a mirror. They were asked to look into the mirror image of their eyes, after tilting their head up and down with decreasing amplitude until they relaxed. The mirror was positioned 200 cm in front the subject.
Statistical analysis
The means of the 3 measurements and the standard deviations were calculated. Because of the sample size, we used the Friedman test to study systematic differences between lip pressure at rest and during swallowing of the 50 patients. The Mann-Whitney test was used to test for any differences between groups 1 and 2, each comprising 25 subjects with a different occlusion. For the assessment of the method error, measurements of 10 randomly selected subjects were repeated 1 week later, and Dahlberg’s formula was calculated si=∑d2/2n−−−−−−−√
si = ∑ d 2 / 2 n
. The method error calculated was about 1.410628 g/cm 2 .
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


