Vertical dimension control is critical for adults with Class II high-angle malocclusions. If the patient has a temporomandibular disorder, this requirement is exacerbated. When extraction is planned, the treatment challenge is further increased. This article reports on a new biomechanical design (C-therapy) appropriate for anterior segment retraction with excellent control of the vertical dimension, even in a Class II high-angle patient with a temporomandibular disorder. Maximum retraction of the maxillary anterior segment can be achieved with a lingual retractor and a palatal miniplate without appliances on the maxillary posterior segments. Mandibular anterior vertical height was well controlled by a second miniplate in the mental region. This device also contributed to mandibular anchorage reinforcement. A patient with temporomandibular disorder symptoms treated with this approach is shown.
As the incidence of adult orthodontic treatment increases, orthodontists learn more about conducting such treatment safely and with improved outcomes. The risks are higher than with a growing adolescent, especially when extractions are involved, because treatment time is extended and resistance to periodontal breakdown is lower. In some patients, extractions are a necessity for a reasonable outcome. Orthodontic specialists know that a hyperdivergent skeletal pattern poses some barriers to a good esthetic outcome. The use of temporary skeletal anchorage devices has renewed enthusiasm for a more dependable result when treating such patients. Improper treatment planning or faulty treatment mechanics can result in backward mandibular rotation and an unesthetic increase in anterior facial height. Any change in the vertical height of the dentoalveolar complex as a result of orthodontic therapy can aggravate the temporomandibular disorder symptoms. The ideal method of anchorage control in these patients allows the desired tooth movement without noxious influences on the temporomandibular joint complex. This concept is particularly valuable in adults, because they will have no compensatory growth in posterior facial height.
Clinicians have proposed a wedge hypothesis to the effect that extraction treatment plans facilitate bite closure. However, recent studies have shown that, even though molars move mesially out of the wedge, they also extrude, keeping pace with an increase in facial height. Thus, careful planning is necessary to control any increase in the anterior vertical dimension that would degrade the esthetics of chin contour.
Common strategies for resisting an increase in anterior vertical dimension and anchorage reinforcement include headgear, a low-hanging transpalatal arch, the Nance holding appliance, and interocclusal bite coverage. Even with these extra measures, we still see minor increases in the mandibular plane angle and moderate loss of posterior anchorage. To compensate for a loss of posterior anchorage, clinicians often follow up with Class II elastics to achieve a Class I outcome. Unfortunately, in a skeletally hyperdivergent patient, the use of Class II elastics will extrude the mandibular molars and prop open the mandible. Independent treatment of the maxillary and mandibular arches can help to prevent these side effects.
When compared with headgear anchorage, temporary skeletal anchorage devices have been reported to predictably distalize or intrude the maxillary and mandibular molars and achieve better results in the treatment of maxillary dentoalveolar protrusion. Many reports support the advantages of temporary skeletal anchorage devices: eg, greater retraction of the maxillary anterior teeth, less anchorage loss of the maxillary posterior teeth, and even molar intrusion, followed by counterclockwise rotation of the mandible, resulting in a decreased sagittal jaw discrepancy.
In this article, we introduce new biomechanical designs appropriate for Class II high-angle patients with temporomandibular disorder, to avoid the use of intermaxillary mechanics. Our target approach has a goal to maintain the vertical dimensions by introducing minimum or no change to the maxillary posterior teeth. No appliances are placed in the maxillary posterior segments. Retraction of the maxillary anterior segment with a palatal miniplate tethered to a lingual retractor was done independently of the maxillary posterior teeth. Mandibular anterior vertical height was controlled during retraction with a special miniplate (C-tube) in the symphysis-menton area.
Material and methods
In the maxillary arch, the lingual appliance (C-retractor) is made of 0.036-in 18-8 stainless steel wire soldered to mesh pads, consolidating the 6 anterior teeth into 1 physical unit ( Fig 1 ). This bonded splint has 2 lever arms extending into the palatal vault, usually extended from a point distal to the central incisors. The palatal plate has a wide horizontal arm (C-plate; Jin Biomed, Bucheon, Korea). It is fixed to the cortical bone of the palate with up to 4 titanium screws (5-6 mm) placed adjacent to the median palatal suture. This temporary skeletal anchorage device provides maximum anchorage with no need for attachments on the teeth of the posterior buccal segment. We have used this setup for both pure orthodontic retraction and corticotomy-assisted retraction or osteotomy patients.
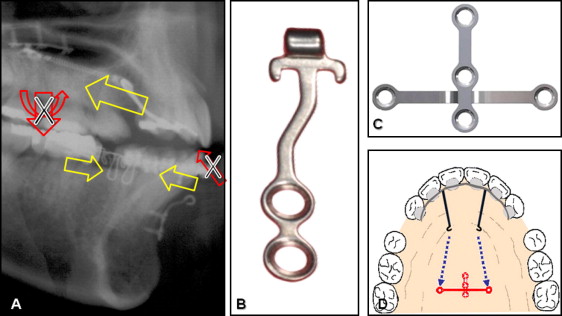
The desired length of the retractor lever arms can be determined by estimating the center of resistance to retraction of the maxillary anterior teeth. If bodily movement is needed, a long lever arm is chosen (about 10 mm into the palate from the facial-axis point on the lingual surface of these teeth). For a controlled tipping movement (with the incisor’s apical tip as the center of rotation), a shorter lever arm (about 7 mm) is effective.
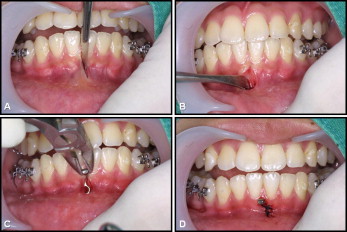
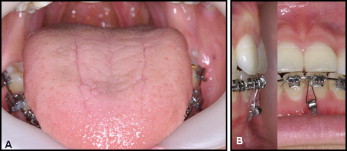
In the mandibular arch, a smaller miniplate (C-Tube; Jin Biomed) is placed on the facial surface of the symphysis. This miniplate is smaller than most and has an adjustable leg ending in a tube that is easily opened to form a hook, if desired. The small size and I-shape design of the C-Tube plate ( Fig 1 , B ) make its surgical placement procedure simple enough that an orthodontic specialist can do it. Here is a brief description of the procedure. After palpation of the symphyseal area, a 5-mm vertical incision is made along the midline ( Fig 2 , A ). Detach the periosteum with an elevator ( Fig 2 , B ). Position the I-type C-tube and anchor it with 2 titanium screws (1.5-mm diameter, 4-mm length). The tube-shaped head part remains exposed to the oral cavity ( Fig 2 , C ). One or 2 sutures are recommended after fixation of the miniplate ( Fig 2 , D ). This system provides good esthetics, rapid and controlled space closure without deepening the overbite, and reasonable comfort ( Fig 3 ). During the retraction period, no intermaxillary elastics were applied. After the en-masse retraction, full fixed orthodontic appliances can be bonded to the maxillary teeth for finishing details.
Clinical application
A 22-year-old woman came to the outpatient clinic of Kyung Hee University Dental Hospital with a chief complaint of mouth protrusion. There were no significant temporomandibular joint symptoms, but a mild degenerative bony change of the condyle was evident on the panoramic view. However, the complication in this patient was a large sagittal centric occlusion-centric relation discrepancy. The pretreatment intraoral photographs showed Class I molar and canine relationships, but in centric relation, the occlusion was Class II molar and canine with a large 6-mm overjet ( Fig 4 ). The pretreatment photographs show the everted thick upper and lower lips, lip incompetency, skeletal Class II, and dental Class I mouth protrusion. The dental midline coincided with the facial midline. There was no obvious crowding. An open-bite tendency and a shallow overjet were observed, and the patient’s swallowing pattern included an anterior thrust. She had no missing teeth and 4 impacted third molars. A panogram (not shown) showed root dilaceration of the maxillary second premolars. The cephalometric analysis (in centric occlusion) showed a slight skeletal Class II relationship (ANB, 4.8°) with a normodivergent facial pattern. Labioversion of the maxillary and mandibular incisors (U1 to FH, 120.5°; IMPA, 110.3°) and a reduced interincisal angle (106.3°) were observed. The patient was diagnosed with skeletal Class II malocclusion with bidentoalveolar protrusion and temporomandibular disorder with a large centric occlusion-centric relation discrepancy.
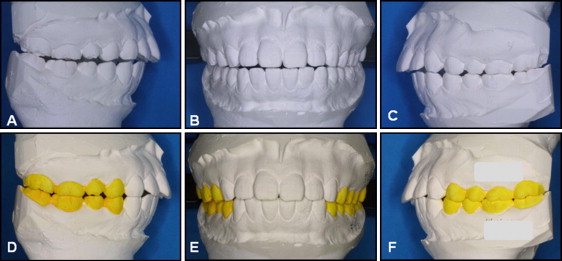
The centric occlusion-centric relation discrepancy was confirmed after a 5-month period of splint wear and adjustment. Three more months of splint therapy established a stable centric relation, so orthodontic treatment could commence. To determine the appropriate teeth for extraction, the cast mounted in centric relation position ( Fig 4 , A-C ) was adjusted by occlusal reduction of the posterior teeth for bite closure ( Fig 4 , D-F ). After occlusal adjustment, the Class II dental relationship was evident. Therefore, a Class II extraction pattern was chosen (maxillary first premolars and mandibular second premolars).
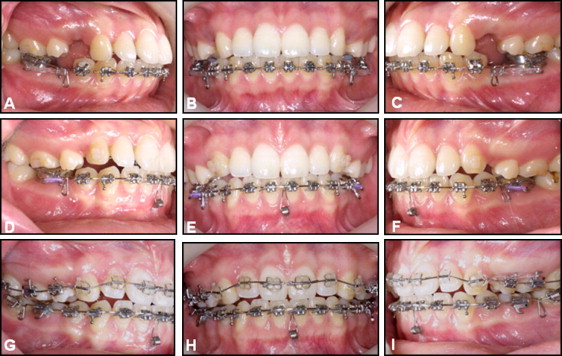
The maxillary anterior teeth were splinted into 1 unit with the C-lingual retractor, and the palatal C-plate provided temporary skeletal anchorage. Nickel-titanium coil springs provided gentle retraction forces ( Fig 5 , A-C ). A total of 400 g was initially loaded on the C-plate by the 2 sides of the lever arm (200 g each). The maxillary first molars were intruded by using a power chain (Forestadent, Pforzheim, Germany) between a bonded transpalatal arch and the horizontal arm of the miniplate. In the mandibular dentition, the goal was reciprocal space closure, so it was treated with conventional labial fixed appliances. A steel closing loop archwire was used in the mandibular arch. Five months later, there was a need to control the vertical height of the mandibular incisors, so a C-tube miniplate was placed in the mandibular symphysis area ( Fig 5 , D-F ). At 14 months, space closure of the mandibular arch was almost completed. The maxillary retraction was completed at 16 months, and the lingual retractor was removed. To detail the occlusal relationships, a 0.022-in slot preadjusted edgewise appliance was placed ( Fig 5 , G-I ). Leveling and further finishing were continued, including final root angulation on the maxillary canines. The total active treatment period was 20 months.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


