Introduction
Our objectives were to develop a reproducible method of superimposing 3-dimensional images for measuring soft-tissue changes over time and to use this method to document changes in lip position after the removal of orthodontic appliances.
Methods
Three-dimensional photographs of 50 subjects were made in repose and maximum intercuspation before and after orthodontic appliance removal with a stereo camera. For reliability assessment, 2 photographs were repeated for 15 patients. The images were registered on stable areas, and surface-to-surface measurements were made for defined landmarks.
Results
Mean changes were below the level of clinical significance (set at 1.5 mm). However, 51% and 18% of the subjects experienced changes greater than 1.5 mm at the commissures and lower lips, respectively.
Conclusions
The use of serial 3-dimensional photographs is a reliable method of documenting soft-tissue changes. Soft-tissue changes after appliance removal are not clinically significant; however, there is great individual variability.
Orthodontic tooth or orthopedic bone movement in the face can affect soft-tissue drape; moreover, it is speculated that most fixed orthodontic appliances have a role to play in the soft-tissue drape. Orthodontic treatment decisions with regard to the need for extraction of teeth are often made in midtreatment based on soft-tissue positions. It is important to gain a better understanding of how or whether orthodontic appliances affect the appearance of the soft tissues, particularly the position of the lips.
To date, the only study on the role of orthodontic appliances on changes in soft-tissue contours used 2-dimensional photographs for evaluation. Advances in 3-dimensional imaging now make it possible to capture and superimpose digital images and measure changes in soft-tissue positions from 3-dimensional photographs taken at several time points. Such advances in facial imaging allow a more thorough investigation of changes in 3 dimensions and prevent the inherent loss of information that results from 2-dimensional imaging.
Cone-beam computed tomography, laser scanners, and structured light-stereo photogrammetry are the current prevailing technologies in 3-dimensional soft-tissue imaging. Although cone-beam computed tomography devices can produce high-quality soft-tissue images, exposure to radiation and noise in the skin surface at the periphery of the cone beam limit their role for soft-tissue assessment alone. In addition, motion artifacts are significantly diminished with the latter devices because the capture time is much shorter. The use of stereo cameras with short shutter speeds such as the 3dMDface stereo camera system (3dMD, Atlanta, Ga) is convenient for clinicians and patients for capturing soft-tissue records.
As 3-dimensional imaging devices and software designed for manipulating digital 3-dimensional files continue to improve, the orthodontic community must assess the effectiveness and reliability of these tools in both research and clinical settings. Previous work has shown the precision and accuracy of images obtained by stereo camera systems clinically compared with direct anthropometric measurements with phantom models. The intraobserver and interobserver repeatabilities of 3-dimensional landmark identification have also previously been established. However, the repeatability of images captured at different time points still must be established.
In this study, we aimed to (1) introduce a method of reliably measuring soft-tissue change between 2 time points using the 3dMDface stereo camera system and (2) use this methodology to evaluate the effect of orthodontic appliance removal on lip positions in 3 dimensions.
Material and methods
The sample included 50 subjects recruited from the patient population of the Department of Orthodontics at the University of North Carolina who had completed their orthodontic care, had a Class I occlusion, and were willing to participate. Patients with lip incompetence and major facial asymmetries were excluded from the study. No efforts were made to select a sample based on age, sex, ethnicity, or race. This study was approved by the institutional review board of the University of North Carolina.
The 3dMDface stereo camera system was used for 3-dimensional photograph capture. The camera consists of 2 sets of 3 cameras (2 monochrome, 1 color) positioned with known angulations and distances from each other. The stereo pair was synchronized to photograph the patient in 1.5 ms to generate 1 continuous point cloud system. The software provided, 3dMDpatient, includes algorithms that use the known location of each camera and information from the calibration process to build the 3-dimensional geometry after capture. The color information is then applied to the geometry to create a photo-realistic 3-dimensional picture.
To prevent displacement of the cameras between acquisitions, they were located in a separate consultation room, and their setup was kept constant. Additionally, daily calibration of the 3-dimensional camera was performed following the procedures recommended by the manufacturer.
Five 3-dimensional photographs were captured for each patient at the debonding appointment ( Fig 1 ). For all patients, 2 photographs were captured immediately before debonding and consisted of “lips sealed before” with the patient in maximum intercuspation occlusion with lips together and “repose before” with the patient in wax-record supported rest position. The wax record was obtained by placing a layer of wax between the posterior teeth and having the patient bite on 3 tongue depressors (height, 3 mm) between the maxillary and mandibular central incisors. The record was subsequently trimmed so that no wax extended beyond the facial surfaces of any teeth. A third predebond 3-dimensional photograph, “lips sealed before repeated,” was taken of 15 patients: this was a repeat of the “lips sealed before” and was captured to determine the reliability of the photographic capture method. For each photograph, the patient was asked to relax his or her facial musculature, swallow, and occlude lightly on the posterior teeth. After the brackets and remaining composite resin were removed, 2 additional photographs were captured. These photographs were “lips sealed after” with the patient in maximum intercuspation occlusion with lips together, as in “lips sealed before,” and “repose after” with the patient in wax-record supported rest position, as in “repose before.” For these images, the subjects were asked again to relax their facial muscles and occlude lightly on first their posterior teeth (for “lips sealed after”) and then the wax record (for “repose after”).
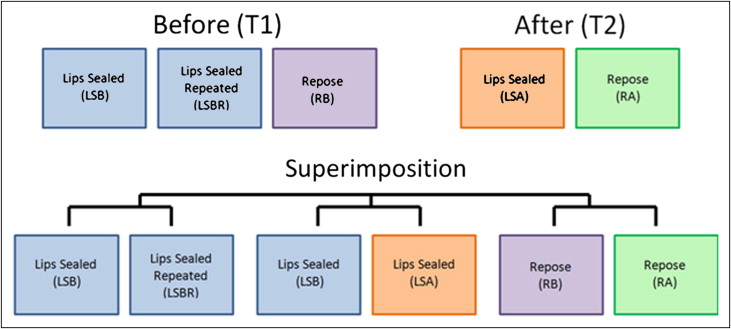
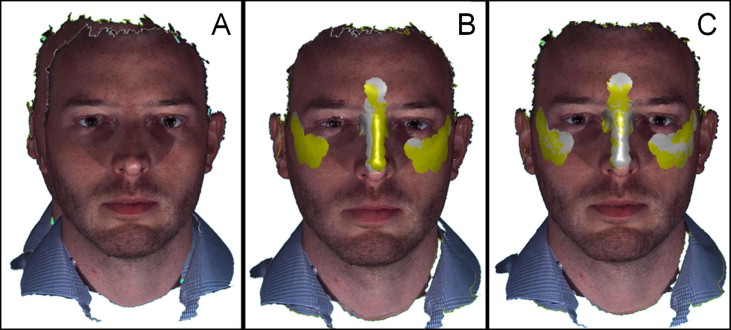
Images from before debonding and after removal of the brackets and resin were registered with the 3dMDpatient software. The postdebond 3-dimensional photo was used as a reference (“lips sealed before” to “lips sealed after,” and “repose before” to “repose after”). The images of “lips sealed before” and “lips sealed before repeated” were registered in the same manner. The images were first registered by using the whole-surfaces function. After the initial registration, as shown in Figure 2 , selections of facial areas on the before and after images were made of the images before debonding and after removal of the brackets and resin of facial areas assumed to be stable between photo acquisitions and unaltered by the orthodontic fixed appliances (intercanthal region, dorsum of the nose, temporal region, and upper zygoma). The program was then used to complete a second best-fit registration based on those selected regions by using iterative closest-point algorithms. Registration error is given by the program as the root mean square of the mean differences between images (mean value, 0.14 mm; SD, 0.05 mm).
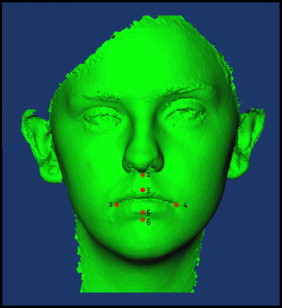
The registered files were exported as open format, binary .STL files, and subsequently converted to open inventor .IV files by using .STL to .SGI open inventor (version 2.0, utility beta; Reuben Reyes, School of Geosciences, University of Texas, Austin). The images were then imported into CranioMaxilloFacial (CMF) application (developed at the M. E. Müller Institute for Surgical Technology and Biomechanics, University of Bern, Switzerland, under the funding of the Co-Me network [ http://co-me.ch/ ]) for 3-dimensional evaluation. To assess changes in anteroposterior lip position after appliance removal, landmarks of interest (right chelion, left chelion, upper lip, lower lip, subnasale, and soft-tissue B-point) were identified on the “lips sealed before” and “lips sealed after” images. The landmarks are shown in Figure 3 . After acquisition and before proceeding to image analysis, a careful quality-control assessment was performed to verify differences in head posture or facial expression that could bias the measurements in this study. The images of 11 subjects showing changes in facial expression from a slight smile or pursing of lips ( Fig 4 ) were discarded, leaving a final sample of 39 subjects in the study. Distance measurements at each landmark were computed by CMF application and reported in millimeters. Directional change was described as either anterior movement after appliance removal (positive value) or posterior movement (negative value).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


