Introduction
Airway dimensions are closely linked to the bone and soft-tissue craniofacial anatomy. Reduction of the airway is seen with airway disorders and can impair function. The purpose of this retrospective study was to determine whether changing from open to closed jaw position affects the volume of the nasal cavity, nasopharynx, and oropharynx; the soft palate; the soft-tissue thickness of the airway; and the most constricted area of the airway.
Methods
Following reliability studies, in this retrospective study, we analyzed cone-beam computed tomography scans taken in both closed and open jaw positions of 60 subjects who were undergoing diagnosis and treatment of temporomandibular disorders. On each scan, condyle-fossa measurements, volumes of airway segments (nasal cavity, nasopharynx, oropharynx), soft palate areas, soft tissue thicknesses of the airway, and the most constricted area of the airway and its location were measured using Dolphin imaging software (version 11.5; Patterson Dental Supply, Chatsworth, Calif). Differences between the 2 jaw positions were analyzed with paired t tests, accepting P ≤0.05 as significant.
Results
Significant changes in airway dimensions were found between the closed and open jaw positions. With jaw opening, the nasopharynx volume increased, whereas the oropharynx volume decreased. Significant decreases were also found for measurements of basion to posterior airway wall, cervical vertebrae to posterior airway wall, most constricted area, nasal cavity volume, and soft palate area when the jaw was open.
Conclusions
Changing jaw position significantly affects airway dimensions.
Highlights
- •
We examined the changes in airway dimensions between open and closed jaw positions.
- •
Opening the jaw significantly affects the airway dimensions.
- •
The oropharynx dimensions significantly decreased with jaw opening.
- •
The area of the most constriction significantly decreased with jaw opening.
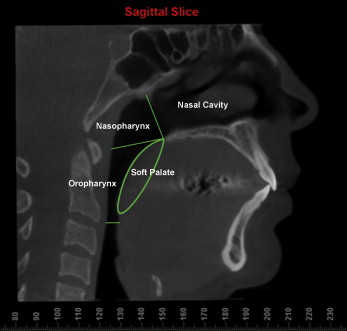
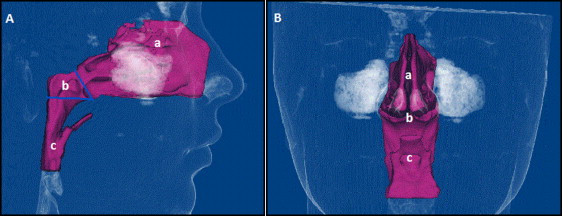
The upper human airway has 2 entrances: the nasal cavity and the oral cavity. They combine in the area known as the pharynx. The pharynx consists of 3 sections: nasopharynx, oropharynx, and laryngopharynx ( Fig 1 ). The nasopharynx is the superior portion of the pharynx that is posterior to the nasal cavity and located behind the soft palate. The oropharynx, below the nasopharynx, acts as a digestive and respiratory conduit and extends to the epiglottis. The laryngopharynx is the area of the pharynx caudal to the epiglottis.
Narrowing of the airway dimensions can lead to challenges in breathing. For example, the sizes of the pharyngeal and palatine tonsils, in the nasopharynx and oropharynx, respectively, influence airway dimensions. Respiratory diseases associated with edema or inflammation of soft tissues can cause airway restriction and decrease the quality of life. Common airway disorders include obstructive lung disorders such as asthma and apneas, which cause a decrease in the volume or flow of air. Obstructive sleep apnea (OSA) is defined as 30 or more episodes of apnea, cessation of airflow for more than 10 seconds, during a normal night of sleep (7 hours). OSA treatment by the orthodontist can vary in invasiveness, but all treatments aim to allow continuous breathing without the cessation of airflow experienced by OSA patients. Previous studies have shown that open-mouthed breathing can increase the severity risk of OSA during sleep. During prolonged dental treatment, those with OSA may have an increased risk of detrimental airway changes when their mouths are open.
Evaluation of the airway has become an important aspect in orthodontic treatment planning. The initial orthodontic screening evaluation is an excellent opportunity to identify symptoms of airway disorders. Questions about snoring, interrupted sleep patterns, and daytime somnolence combined with imaging taken at the examination can indicate possible sleep disorders and support the need for a polysomnograph test for diagnosis. With or without a diagnosis of OSA, it is important to understand the changes that opening the mouth causes in the airway dimensions.
Previous studies on dental patients have shown changes to the airway when patients have their mouths opened with a mouth prop. It is important to understand what the open-jaw position does to the patient’s airway so that treatment can be adapted to the patient’s needs. Some patients may need more breaks during treatment to keep their oxygen saturation higher. Even though continuous positive airway pressure is the gold standard in treatment, other treatment modalities can be used, such as dental appliances to improve airway function, or advancing the upper or lower jaw by orthognathic surgery. Most dental appliances aim to move the mandible forward and open the airway. Studies have shown airway changes with both mandibular advancement splints and tongue stabilizing devices. It has been reported that head and jaw positions significantly affect airway dimensions. However, comparing open-jaw position with closed-jaw position and its influence on the airway dimensions using 3-dimensional (3D) cone-beam computed tomography (CBCT) imaging has not been previously studied.
A few studies have previously evaluated the differences in airway between open and closed jaw position. However, these were done in patients wearing rubber dams or using mouth props for restorative dental procedures. In the study by Iwatani et al, 20 adult subjects were imaged with magnetic resonance imaging (MRI). The authors found that the oropharyngeal airway volume decreased significantly with the mouth open, but the retropalatal and hypopharyngeal areas were not significantly affected. The second study by Ito et al was done with 13 subjects and using lateral cephalograms, except for 1 subject who had a computed tomogram taken. They reported a decrease in upper airway sagittal diameter when using a mouth prop. The subjects also indicated increased dyspnea when the mouth was maximally open. With the greater interest in airway disorders and the estimated 80% to 90% of people with undiagnosed OSA having moderate-to-severe OSA, it is important to understand the changes when a patient fully opens his or her jaws.
Imaging methods to view the airway include cephalometric radiographs, CBCT, and MRI. Lateral cephalometric radiographs were the only method available before CBCT and MRI. This method had the limitation of imaging a 3D structure in 2 dimensions. Volume and cross-sectional areas could not be accurately assessed with lateral cephalometric radiographs. Some additional limitations with lateral cephalometric radiographs are image magnification or enlargement and distortion, structure overlap, limited identifiable landmarks, and positioning problems. MRI is used to measure the airway 3 dimensionally and to visualize ventilation differences in respiratory diseases. Studies have shown that both CBCT and MRI are accurate ways to measure the airway. However, CBCT offers an easier, quicker, and more accurate method to obtain a view of a patient’s airway than MRI. CBCT has been used for measuring airways in studies looking into changes related to facial bony structure, developmental changes, before-and-after orthodontic treatments, maxillofacial surgeries, temporomandibular disorder (TMD), and cleft lip and palate. CBCT imaging is an accurate way of visualizing the condyle and measuring its position and location.
This retrospective radiographic study was an exploratory study to determine the effects of mandibular positional changes on the upper airway dimensions.
Material and methods
After institutional review board approval from Indiana University for this retrospective study, we retrieved the CBCT images of 60 patients from the archives of the School of Dentistry’s Department of Oral Pathology, Medicine and Radiology. Each subject had 2 scans taken (13.3 in): 1 in closed jaw position and 1 at maximum open position (some showing a limited field of view due to jaw opening). The CBCT scans were taken at 8.9 seconds, with a voxel size of 0.3. The inclusion criteria for this study were patient age 18 years or more, no previous orthognathic surgery, 2 CBCT images (closed, open) taken at the same session, and no airway pathology noted on the radiology cone beam report. The average age of the subjects was 40 years 4 months ± 17 years 8 months. All subjects were female.
The CBCT images were downloaded into Dolphin 3D imaging software (version 11.5; Patterson Dental Supply, Chatsworth, Calif) and measured on the same computer and monitor. All 60 patient CBCTs were coded, and information on age and sex was recorded. Then the subject information was deidentified.
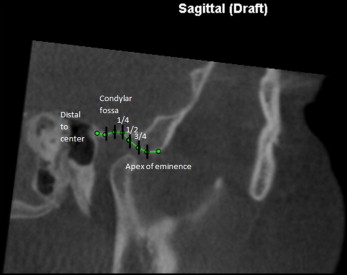
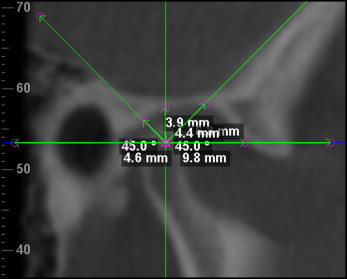
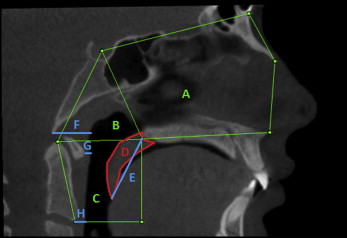
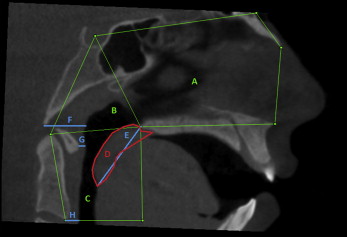
Because of the limited field of view, some of the 3D CBCT images did not show both the maxillary and mandibular incisors. Because of this, the condyle-fossa relationship of the jaws was used to determine the amount of opening by the amount of translation of the condylar head along the articular eminence instead of measuring the vertical distances between the central incisors of the maxilla and mandible. On views that showed both the condyle and incisors, the vertical distance between the maxillary and mandibular incisors was also measured. Both the rotation and the translational movement along the articular eminence to the apex of the eminence lead to opening of the mouth. The magnitude of opening is based on the amount of rotation and the amount of translation during mandibular movement. Translation and rotation were measured on both condyles in the open and closed radiographs. Translation was determined by visually dividing the glenoid fossa into 6 sections: center of the fossa, quarter, half, three quarters, top of eminence, and past eminence ( Fig 2 ), and determining how far along the glenoid fossa the condyle had translated. This view was obtained from a sagittal slice through the middle of both condylar heads. Rotation was measured by taking 5 linear measurements from the glenoid fossa to the condyle. A sagittal slice through the middle of the condyles was obtained. Then a horizontal plane was placed through the widest width of the condylar heads visible on the slice. Lines were drawn through the midpoint of the condylar head crossing at 45°, 90°, and 135°. Five linear measurements representing the anterior, anterosuperior, superior, posterosuperior, and posterior directions were taken from the fossa wall to the center of the condyle (intersection of the 5 lines) ( Fig 3 ). All images were oriented in the sagittal, axial, and coronal planes before taking measurements following methods used in previous airway studies. This allowed us to determine changes in the condylar head position as the jaw opens.
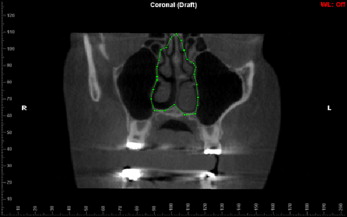
The airway and soft-tissue measurements taken on CBCT images with both open and closed jaws are shown in Table I and Figures 4 through 7 .
| Anterior boundary | Posterior boundary | Superior boundary | Inferior boundary | |
|---|---|---|---|---|
| Nasal cavity | Line connecting the anterior nasal spine (ANS) and the apex of the nasal bone | Line extending from sella (S) to posterior nasal spine (PNS) | Line connecting nasion or the highest point on the nasal bone 1 mm inferior to the edge of the field of view and S | Line extending from ANS to PNS |
| Nasal cavity coronal boundary: outline of nasal cavity in section containing maxillary first molar bifurcation, starting at crista galli and running down to the nasal floor following the sidewalls of the right and left nasal cavity | ||||
| Nasopharynx | Line extending from S to the PNS | Line extending from S to the tip of the odontoid process | Line extending from PNS to the tip of the odontoid process | |
| Oropharynx | Line extending from PNS perpendicular dropping to the line parallel to the ruler running through anteroinferior border of CV2 | Line extending from the tip of the odontoid process to the anteroinferior border of CV2 | Line extending from PNS to the tip of the odontoid process | Line extending from PNS to the tip of the odontoid process |
| Soft palate | ||||
| Length: length from the PNS to the most posteroinferior point of the soft palate | ||||
| Area: confined by the area that starts and ends at PNS through the uvula tip | ||||
| Soft-tissue measurements | ||||
| AA (most anterior point on the anterior arch of the atlas vertebrae) to the posterior airway wall | ||||
| CV2ia (most inferior-anterior point of CV2) to the posterior airway wall | ||||
| Basion to the posterior airway wall | ||||
| Most constricted area of airway | ||||
The primary investigator (L.G.) performed reliability measures using 10 coded and randomized CBCTs on all parameters. These CBCTs were coded and randomized, and the investigator was blinded to the names of the subjects. In 2 weeks, the same 10 subjects were retraced in a new randomly assigned order. All measurements were checked for accuracy and reviewed by another expert investigator (A.G.). Reliability was calculated with the goal that the intraclass correlation coefficient (ICC) was greater than or equal to 0.80. This process was repeated until ICCs were greater than or equal to 0.80.
Statistical analysis
The reliability data were analyzed using ICCs and Bland-Altman plots to assess the intraexaminer reliability. Summary statistics (means, standard deviations, standard errors, ranges) were calculated for all measurements from both the closed and open jaw positions. The differences between the measurements and the ratio of the measurements for the 2 jaw positions were calculated and summarized. Comparisons between the closed and open jaw position measurements were made using paired t tests with P ≤0.05 as significant. For measurements that were made on both the left and right sides, mixed-model analysis of variance was used to evaluate whether the closed vs open comparison was affected by side. Pearson correlation coefficients were used to evaluate the associations among the airway parameters. Translation of the condyles was compared using Cochran-Mantel-Haenszel tests for repeated ordered categorical data.
Results
A correlation coefficient greater than 0.80 was obtained for all reliability values except for the anterosuperior condyle measurement, which had too much variability to accept the readings.
Descriptive statistics for the measurements in the closed and open jaw positions and for the differences (open, closed) are presented in Tables II and III . Statistically significant differences were detected in multiple parameters between the groups ( Table III ). Measurements that decreased in the open position compared with the closed position were basion-posterior airway wall, CV2ia-posterior airway wall, most constricted area, nasal cavity volume, oropharynx volume, and soft palate area; nasopharynx volume and maxillary incisor tip to mandibular incisor tip increased ( Table III ). The values of AA-posterior airway wall and soft palate length did not show any significant differences. Statistics for each condyle measurement by side and jaw position are summarized ( Table IV ). A summary of the condyle measurement statistics for the differences between the closed and open jaw positions of each condyle measure is given in Table V . Comparisons of condyle positions show the differences between the open and closed jaw positions, with the open position always significantly larger than the closed ( Table VI ). This shows that there was a change in jaw position with the jaw open but no difference between the right and left sides.
| Measurement | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| AA-posterior airway wall (mm) | |||||
| Closed | 60 | 3.37 | 1.57 | 0.10 | 8.40 |
| Open | 60 | 3.32 | 1.53 | 1.30 | 8.00 |
| Basion-posterior airway wall (mm) | |||||
| Closed | 60 | 16.95 | 3.65 | 11.60 | 29.50 |
| Open | 60 | 16.61 | 3.59 | 11.20 | 30.20 |
| CV2ia-posterior airway wall (mm) | |||||
| Closed | 60 | 3.94 | 0.89 | 2.70 | 8.50 |
| Open | 60 | 3.68 | 1.10 | 1.30 | 8.00 |
| Most constricted area (mm 2 ) | |||||
| Closed | 60 | 177.11 | 79.49 | 19.90 | 323.60 |
| Open | 60 | 112.05 | 59.48 | 29.80 | 272.80 |
| Nasal cavity volume (mm 3 ) | |||||
| Closed | 60 | 16590 | 4351 | 9440 | 30230 |
| Open | 60 | 15487 | 4182 | 6714 | 26552 |
| Nasopharynx volume (mm 3 ) | |||||
| Closed | 60 | 7015 | 1951 | 1926 | 10873 |
| Open | 60 | 7556 | 2007 | 1991 | 11230 |
| Oropharynx volume (mm 3 ) | |||||
| Closed | 60 | 11893 | 4060 | 3209 | 20110 |
| Open | 60 | 9893 | 3499 | 3921 | 17924 |
| Soft palate area (mm 2 ) | |||||
| Closed | 60 | 286.94 | 49.24 | 185.00 | 400.10 |
| Open | 60 | 272.09 | 50.24 | 120.50 | 385.10 |
| Soft palate length (mm) | |||||
| Closed | 60 | 37.88 | 4.35 | 28.40 | 47.90 |
| Open | 60 | 38.68 | 4.15 | 25.50 | 45.00 |
| U1 tip-L1 tip (mm) | |||||
| Closed | 60 | −2.84 | 1.99 | −7.20 | 5.20 |
| Open | 57 | 20.76 | 8.13 | 5.20 | 36.80 |
| Measurement | n | Minimum | Maximum | Mean difference, open-closed | SD | P value |
|---|---|---|---|---|---|---|
| AA-posterior airway wall (mm) | 60 | −1.60 | 3.40 | −0.05 | 0.88 | 0.6597 |
| Basion-posterior airway wall (mm) | 60 | −3.60 | 3.40 | −0.34 | 1.11 | 0.0217 |
| CV2ia-posterior airway wall (mm) | 60 | −2.30 | 1.50 | −0.26 | 0.82 | 0.0173 |
| Most constricted area (mm 2 ) | 60 | −217.0 | 104.10 | −65.06 | 68.78 | <0.0001 |
| Nasal cavity volume (mm 3 ) | 60 | −5900 | 7010 | −1103 | 2028 | <0.0001 |
| Nasopharynx volume (mm 3 ) | 60 | −2700 | 2457 | 542 | 930 | <0.0001 |
| Oropharynx volume (mm 3 ) | 60 | −10096 | 5322 | −2000 | 3005 | <0.0001 |
| Soft palate area (mm 2 ) | 60 | −190.7 | 75.20 | −14.85 | 43.93 | 0.0112 |
| Soft palate length (mm) | 60 | −22.40 | 10.40 | 0.80 | 4.30 | 0.1536 |
| U1 tip-L1 tip (mm) | 57 | 10.10 | 39.20 | 23.59 | 8.15 | <0.0001 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


