MULTI-SYSTEM TRAUMA INFLUENCING THE TREATMENT OF MAXILLOFACIAL TRAUMA
The spectrum of management of the injured patient begins at the moment of injury and concludes when the patient has returned home and/or has attained his or her maximal level of functional recovery. The scope of care and tenets of evaluation of the trauma patient are complex and far-reaching—well exceeding the scope of a single review chapter. Important considerations for the evaluation of focal isolated injuries or organ-based injuries are also considered in other chapters of this textbook. The interested reader is also referred to other sources regarding trauma, including the Advanced Trauma Life Support course as well as textbook. Other useful references include the textbook Trauma by Moore, Feliciano, and Mattox. The scope of this chapter is to focus on the trauma patient with multi-system injuries with a specific eye on the “pearls and pitfalls” of managing the many details involved in this process. Specific attention will be devoted to those issues that impact on the care, coordination, and successful team management of the multi-system trauma patient with maxillofacial injuries. The construct and content of this discussion will arbitrarily divide these issues into the following time-related sequences:
- 1.
Issues of concern before leaving the trauma bay
- 2.
ICU implications
- 3.
Trauma patients on the floor
- 4.
Patients ready for rehabilitation
ISSUES IN THE TRAUMA BAY
The primary tenet(s) of care of the injured patient is to rapidly and immediately access the A irway, B reathing, and C irculation as well as the neurologic evaluation ( D isability) with complete E xposure ( Figure 6-1 ). A follow-up secondary survey most thoroughly evaluates for associated injuries, with particular attention to potentially occult problems such as intra-abdominal hemorrhage and pelvic fractures. The spectrum of this care extends well beyond the scope of this chapter. Instead, this chapter assumes that the immediate life-threatening concerns and problems are being evaluated and managed in an ongoing fashion by a multi-disciplinary team led by the trauma surgery service. It is at this point that finding the “devil in the detail” is so important.

Complete evaluation of the trauma patient includes recognition of all of those issues that threaten the survival of the patient. In many instances (penetrating trauma, major long bone fractures, traumatic brain injury with coma), these threats are visible and immediately recognizable. An equally challenging concern is to appropriately evaluate the apparently stable (or stabilized) patient to detect potentially occult injuries. A number of these occult injuries are discussed.
EVALUATION OF THE ABDOMEN
Missed intra-abdominal hemorrhage remains the most common cause of preventable death in the blunt trauma patient. It has been estimated that 16-25% of all potentially preventable trauma deaths are linked to failure to appropriately identify intra-abdominal hemorrhage. The evaluation of the trauma patient’s abdomen in the search for intra-abdominal hemorrhage is notoriously difficult because of changes of stress, altered levels of consciousness, pain from concomitant injuries, and/or the presence of alcohol or drugs, which limit the accuracy of physical examination. The peritoneal compartment can readily contain a significant volume of hemorrhage without visible evidence of distenion. The burden of proof remains the responsibility of the trauma team to rapidly and accurately identify any potential source of intra-abdominal hemorrhage. There are three commonly used evaluative tests to assay for the presence of intra-abdominal hemorrhage: diagnostic peritoneal lavage (DPL), focused abdominal sonography for trauma (FAST), and CT scan. Each of these tests has strengths and weaknesses, which the practitioner must be knowledgeable of in order to appropriately and successfully use them to the benefit of the patient. These tests are best considered as complementary to one another rather than exclusionary. Each of these tests is briefly discussed below.
Diagnostic Peritoneal Lavage
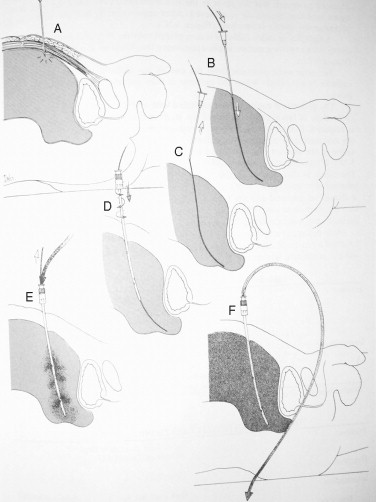
DPL was first described by Dr. Harlan Root and associates in the early 1960s. DPL consists of the placement of a peritoneal dialysis catheter directed to the pelvic space of the peritoneal compartment via a direct approach ( Figure 6-2 ). Following initial placement, the catheter is aspirated for the presence of blood, with greater than 10 mL of aspirated blood being considered a positive result ( Figure 6-3 ). If direct aspiration is negative, 1 L of crystalloid solution is infused via the catheter into the peritoneal cavity and then drained via gravity. The subsequently retrieved fluid is sent for laboratory analysis and/or is visually examined at the bedside ( Figure 6-4 ). Frankly sanguineous fluid or a laboratory count of greater than 10 red blood cells per cubic millimeter is considered a positive test and is generally accepted as an indication for exploratory laparotomy. The liabilities of DPL are considered to be the semi-invasive nature of the procedure and the necessity of familiarity with the surgical skills of peritoneal puncture. DPL has also been criticized for being overly sensitive (capable of detecting as little as 10 mL of blood within the abdomen) and thereby leading to a rate of non-therapeutic laparotomy as high as 40%. Despite these apparent shortfalls and criticisms, DPL remains a well-defined procedure that may be completed rapidly in the ER while a patient is undergoing simultaneous evaluation and resuscitation by other members of the trauma team. DPL also offers the advantage of being able to be conducted in an austere or remote situation with minimal equipment when more sophisticated equipment, such as ultrasound or CT scanners, is not available.


Focused Abdominal Sonography for Trauma
The detection of occult intra-abdominal hemorrhage remains a key component of the trauma evaluation. In the mid 1990s, Rozycki, Ochsner, and others, began to detail the use of ultrasonography as a means of rapidly assaying the intra-abdominal compartment. The FAST examination consists of four narrowly defined ultrasound windows that are intended to be evaluated for the presence of fluid. The FAST examination considers the presence of fluid in the abdomen in this setting to be the equivalent of blood. The four views consist of (1) subxiphoid to evaluate the cardiac silhouette and the presence of cardiac tamponade, (2) the right upper quadrant or Morison’s pouch to detect blood in the hepatorenal fossa (the lowest point of the right upper quadrant), (3) left upper quadrant to detect blood in the spleno-renal space, and (4) a pelvic view to detect blood in the pouch of Douglas (behind the bladder and anterior to the rectum, which is the most dependent portion of the peritoneum). The views of the FAST examination take advantage of the anatomically dependent portions of the abdomen in the supine patient ( Figure 6-5 ). Acquiring adequate expertise requires a fairly distinct learning curve of approximately 50 examinations. In experienced hands, the FAST examination has a demonstrated sensitivity in excess of 85-90% for the detection of quantities of blood greater than 200 mL in the abdomen. The FAST scan is rapid and non-invasive and may be completed early in the trauma resuscitation while other care is being delivered. With continued technologic evolution, the equipment for FAST is becoming increasingly portable (5-8 lb) with ever-increasing sophistication and resolution of this equipment. The liabilities of the FAST examination are primarily the reliance on equipment and the necessity of appropriate skill and experience in order to conduct this test reliably. Certain patient conditions such as morbid obesity and/or the presence of subcutaneous air also limit the applicability of the FAST examination.

Computed Tomography Scanning
CT scanning of the abdomen has been a recognized component of the trauma evaluation for over 20 years. The advantage of CT scanning is the significant anatomic detail delivered by this modality. With each successive generation of CT scanners, resolution increases and time of data acquisition decreases. The continued liability of CT scanning remains the necessity of transporting a critically ill and potentially unstable patient to a remote site and then leaving the patient in the scanner removed from the immediate care of the team. Although initially used for evaluation of the head and the abdomen, CT scanning is now of recognized utility for delineating injuries to the chest and neck as well. As each additional diagnostic CT survey is added, the clinician must remain cognizant of the additional time required while a trauma patient is essentially inaccessible to ongoing care. It is not unusual even for a modern, sophisticated CT scanner to require over 45 minutes in acquiring the necessary information for scans of the head, neck, chest, and abdomen. Two specific aspects of CT scanning should be mentioned for additional consideration: namely, the presence of a “blush” and the ability of CT scanners to detect complex vascular injuries.
The standard CT protocol for evaluating the trauma patient includes the administration of IV contrast just prior to the initiation of the scanning of the chest and/or abdomen. The presence of IV contrast enhances the ability to discern anatomic detail and enhances the ability to detect acute ongoing hemorrhage from intra-abdominal or intra-thoracic sources. Most commonly this is visualized as a “hot spot” or “blush” of focal intense contrast indicating pooling or extravascular accumulation of the contrast agent. Detecting a vascular “blush” during a trauma CT scan is an important value added to this diagnostic modality. The detection of a blush aids in the diagnosis of hemorrhagic shock and may aid in directing therapy. The presence of a vascular blush in a fractured spleen or liver indicates a higher probability of the need for intervention as well as the potential use for angiographic embolization. The presence of a vascular blush in a fractured pelvis suggests the need for urgent pelvic angiography as an adjunct to hemodynamic and orthopedic stabilization. The presence of the trauma team at the CT scanner aids in early recognition of a blush and allows for the acquisition of delayed scans to lend additional detail of the anatomic area in question. If a blush is seen on the first pass CT, the patient is rescanned while still on the CT table. This “delayed” scan delivers a second set of anatomic details, which allows for the temporal evaluation of the extent and aggressiveness of the bleeding pattern. The presence of on-site interpretation of trauma CT scans by experienced trauma surgeons and/or radiologists remains an integral part of the successful use of CT scanning.
The utility of CT scanning in detecting complex and occult vascular injuries is discussed further in this chapter.
THINGS TO BE CHECKED BEFORE LEAVING THE EMERGENCY DEPARTMENT
The conduct and care skills of the immediate ABCs of trauma resuscitation are well-detailed in other sources (ATLS) and are beyond the scope of this discussion. The next portion will look at a number of considerations that must be discussed among the trauma team members and consulting services after the patient has been initially stabilized and before the patient is moved from the trauma bay. These considerations include, but are not limited to, detection of occult pneumothorax, management of complex pelvic fractures, and recognition of the potential for great vessel injuries.
OCCULT PNEUMOTHORAX
The initial chest x-ray obtained early in the resuscitation sequence is usually obtained while the patient is lying in a supine position and often on a spine stabilization device such as a backboard. These considerations impose technical limitations on the quality of trauma bay chest x-rays. It has been demonstrated that as many as 40% of traumatic pneumothoraces are missed on initial trauma bay anterior-posterior chest radiographs. Once stabilized and spine clearance is achieved, consideration should be given to obtaining an upright PA chest x-ray in follow-up to provide a more thorough evaluation for the presence of pneumothorax. As an alternative, CT scanning of the upper abdomen or of the thorax provides exquisite anatomic detail and should be carefully reviewed for the presence of extra-parenchymal air (pneumothorax) ( Figure 6-6 ). The presence of a traumatic pneumothorax of any significant size (>5-10%) is generally considered an indication for the placement of a chest tube thoracostomy prior to general anesthesia and/or if the patient is intubated and undergoing mechanical ventilation.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


