Temporomandibular disorder (TMD) is a collective term that encompasses a number of clinical problems involving the masticatory muscles or the temporomandibular joints. These disorders have been identified as a major cause of nondental pain in the orofacial region, and are considered to be a subclassification of musculoskeletal disorders .
Orofacial pain and TMD can be associated with pathologic conditions or with disorders related to somatic and neurologic structures, such as primary headache disorders and neurogenic pain disorders. Primary headache disorders are a group of pain disorders that originate in neuropathology and vascular pathology. Neurogenic pain disorders are conditions resulting from functional abnormalities within the nervous system. When patients present to the dental office with a chief complaint of pain or headaches, it is vital for the practitioner to understand the cause of the complaint and to perform a thorough examination that will lead to the correct diagnosis and appropriate treatment. A complete understanding of the associated medical conditions with symptomology common to TMD and orofacial pain is necessary for a proper diagnosis.
One critical point of understanding for the clinician is the concept of chronic versus acute pain. The International Association for the Study of Pain has defined chronic pain as pain lasting longer than 6 months. Therefore, acute pain refers to pain from onset to 6 months ( Fig. 1 ). The pain pathway has two divisions. One of the divisions travels through the midbrain, to terminate in the posterior aspect of the lateral thalamus (the discriminative system). The other division travels through the medial thalamus to the hypothalamus and limbic forebrain (the motivational/effective system). The discriminative system allows the brain to properly locate the site and source of pain. The motivational/effective system involves the emotional component of painful experiences .
During the first 6 months of pain, the discriminative system dominates the motivational/effective system, allowing the patient to comprehend better the location and duration of his/her pain. The patient can describe the pain more accurately because the brain is better able to localize and isolate it. However, as time progresses, expression of the motivational/effective system gains in strength and begins to play a more dominant role in the pain experience. At 6 months, an inversion of the pain response expression occurs, in which the motivational/effective system now dominates the pain language. Consequently, the pain language used by the chronic pain patient is characterized more by psychologic terms than descriptive terms. As the pain continues without resolution, the pain language becomes so nondescript that it is difficult for the dental practitioner to identify the source and site of the pain. In this situation, the words used to describe the pain can provide only “clues” to diagnosis and treatment. It is vital that the practitioner be aware of the patient’s history and any potential conflicts or contributing factors that may play a role in the patient’s pain expression .
When faced with a patient suffering from pain, the differentiation of acute from chronic pain begins at the initial visit. In history taking, one of the first questions the practitioner must ask is, “How long has this pain been present?”
The most common symptoms of acute pain are headaches, jaw pain, earache, neck pain, muscle soreness, muscle tightness, and teeth pain ( Box 1 ). Conversely, the most common symptoms reported by the chronic pain sufferer are headaches, depression, chronic fatigue, sleep disorders, decreased productivity, feelings of inadequacy, low self-esteem, withdrawal, and mood disorders ( Box 2 ).
- •
Headaches
- •
Jaw pain
- •
Earache
- •
Neck pain
- •
Muscle soreness
- •
Muscle tightness
- •
Tooth pain
From Auvenshine RC. Acute vs. chronic pain–an overview. Tex Dent J 2000;117(7):19.
- •
Headaches
- •
Depression
- •
Chronic fatigue
- •
Sleep disorders
- •
Decreased productivity
- •
Feelings of inadequacy
- •
Low self-esteem
- •
Withdrawal
- •
Decreased libido
From Auvenshine RC. Acute vs. chronic pain–an overview. Tex Dent J 2000;117(7):19.
Comparison between the symptoms of acute and chronic TMD suggests that the pain language and descriptions of patients who have acute pain are more specific and somatically accurate. Their reported symptoms define location and pain intensity. In contrast, the pain language used by chronic pain sufferers is more vague and less descript. Their pain language becomes wrapped in psychologic terminology, indicating the dominance of the motivational/effective system .
Chronic pain continues to be poorly understood and managed. However, research endeavors to broaden our understanding of pain and to contribute valuable insight into pain management. For instance, it is known that nerve signals arising from sites of tissue or nerve injury lead to long-term changes in the central nervous system (CNS) and in the amplification and persistence of pain. These nociceptor activity–induced, neuronal changes, known as central sensitization (CS), have important clinical implications in the development of new approaches to the management of persistent pain and to poorly understood conditions such as oral dysesthesia, burning mouth syndrome, atypical facial pain/atypical odontalgia, common peripheral nerve injury/deafferentation, and phantom tooth syndrome .
Historical background
Patients seek help from doctors for symptoms, which are warning signs of impending disease. Symptoms are the expression of a patient’s subjective experience in his/her body. Diseases are objectively observable abnormalities in the body. Difficulties arise when the doctor can find no objective changes to explain the patient’s subjective experience. When this occurs, these symptoms are referred to as “medically unexplained” or “functional” . Many different functional syndromes have been described. In fact, each medical specialty seems to have at least one. For rheumatologists, prominent muscle pain and tenderness is fibromyalgia (FM); for gastroenterologists, abdominal pain with altered bowel habit is irritable bowel syndrome (IBS); for internal medicine specialists, chronic fatigue and myalgia is a postviral or chronic fatigue syndrome (CFS) ( Table 1 ) .
| Specialty | Syndrome |
|---|---|
| Dentistry |
|
| Neurology |
|
| Ear, nose, and throat |
|
| Allergy | Multiple chemical sensitivity |
| Internal medicine | Chronic (postviral) fatigue syndrome |
| Rheumatology | Fibromyalgia |
| Gastroenterology |
|
| Gynecology |
|
| Respiratory medicine | Hyperventilation syndrome |
| Cardiology | Atypical or noncardiac chest pain/ MVP dysautonomia |
The existence of specific somatic syndromes is said to reflect a tendency of specialists to focus on only those symptoms pertinent to their specialty, rather than on any real differences among patients. Three major questions that can be postulated are:
- 1.
Do published diagnostic criteria for each specific functional syndrome overlap in their constituent symptoms?
- 2.
Do patients who have one functional somatic syndrome also meet symptom criteria for others?
- 3.
Are there similarities across syndromes and nonsymptom characteristics of sex, coexisting emotional disorders, proposed causes, and prognosis and response to treatment ?
Various names have been given to functional somatic syndromes, including somatization, somatoform disorders, and medically unexplained symptoms. Functional somatic syndromes and their symptoms pose a major challenge to medicine and dentistry. These syndromes have symptoms that are common and frequently persistent, and are associated with significant distress and disability. Functional somatic syndromes are not only common, but also clinically important, and can be a major health issue. Most of the current thinking toward these syndromes is focused on medical subspecialties, when, in fact, a review of the literature strongly suggests that these syndromes have much in common. Therefore, they should have a broader definition because several of these syndromes can be present in the same individual. Conventional medical therapy is fairly ineffective for these patients, and results in frustrated physicians and dissatisfied patients with chronic symptoms; it often leads to unnecessary expenditure of medical resources.
Central sensitivity syndrome
In 2000, Yunus reviewed the evidence for CS and functional somatic syndromes. He compared FM-related syndromes, and coined the term “central sensitivity syndrome” (CSS). He stated that CSS comprises a similar and overlapping group of syndromes that lack demonstrable structural pathology and are bound by a common pathway, which leads to CS ( Fig. 2 ). Members of this group include FM syndrome, chronic headaches, IBS, CFS, myofascial pain syndrome, restless leg syndrome, periodic limb movement disorder, TMD, multiple chemical sensitivity (MCS), female urethral syndromes, interstitial cystitis, primary dysmenorrhea/“functional” chronic pelvic pain, posttraumatic stress disorder, and depression . Although proof of CS is lacking in some of the syndromes at this time, Yunus included them, based on clinical presentation.
Yunus first suggested a relationship among these various syndromes in 1981. This controlled study demonstrated an association between IBS, tension type headaches, and migraine. In addition, the presence of overlapping conditions was noted to occur in some patients, with muscle spasms being the common binding symptom .
Nearly all chronic pain sufferers complain of depression, despite the current lack of direct evidence linking CS to sensory function in depression. In recent years, Post of the National Institutes of Health has presented arguments suggesting that depression is based on CS. This approach recognizes that most cases of depression follow stressful events, primarily of a psychosocial nature, which initiate various biologic processes, including gene transcription and other neurochemical-hormonal changes. These modifications lead to intracellular changes and subsequent CS . When continued exposure to stress occurs, even of less severity, there is a progressive sensitization of the CNS. Neuronal hyperexcitability then becomes self-sustained, so that, even without discernable stress, depression becomes chronic . A similar model has also been suggested for other psychiatric diseases, such as anxiety disorders .
The understanding of CSS is of great value to the dental practitioner. Therefore, emphasis should be placed on training the clinician for recognition, proper treatment, or referral of these distressing disorders. Because these disorders are interrelated and may be expressed in the same individual, knowledge of mutual association is vital for earlier and more accurate diagnosis, thus avoiding unnecessary and expensive investigations. Treatment that is effective by clinical trials in one patient may not be effective in others, but the more that is known about the pathophysiology of CS, the more appropriate will be the treatment rendered and the more positive the outcomes.
Central sensitivity syndrome
In 2000, Yunus reviewed the evidence for CS and functional somatic syndromes. He compared FM-related syndromes, and coined the term “central sensitivity syndrome” (CSS). He stated that CSS comprises a similar and overlapping group of syndromes that lack demonstrable structural pathology and are bound by a common pathway, which leads to CS ( Fig. 2 ). Members of this group include FM syndrome, chronic headaches, IBS, CFS, myofascial pain syndrome, restless leg syndrome, periodic limb movement disorder, TMD, multiple chemical sensitivity (MCS), female urethral syndromes, interstitial cystitis, primary dysmenorrhea/“functional” chronic pelvic pain, posttraumatic stress disorder, and depression . Although proof of CS is lacking in some of the syndromes at this time, Yunus included them, based on clinical presentation.
Yunus first suggested a relationship among these various syndromes in 1981. This controlled study demonstrated an association between IBS, tension type headaches, and migraine. In addition, the presence of overlapping conditions was noted to occur in some patients, with muscle spasms being the common binding symptom .
Nearly all chronic pain sufferers complain of depression, despite the current lack of direct evidence linking CS to sensory function in depression. In recent years, Post of the National Institutes of Health has presented arguments suggesting that depression is based on CS. This approach recognizes that most cases of depression follow stressful events, primarily of a psychosocial nature, which initiate various biologic processes, including gene transcription and other neurochemical-hormonal changes. These modifications lead to intracellular changes and subsequent CS . When continued exposure to stress occurs, even of less severity, there is a progressive sensitization of the CNS. Neuronal hyperexcitability then becomes self-sustained, so that, even without discernable stress, depression becomes chronic . A similar model has also been suggested for other psychiatric diseases, such as anxiety disorders .
The understanding of CSS is of great value to the dental practitioner. Therefore, emphasis should be placed on training the clinician for recognition, proper treatment, or referral of these distressing disorders. Because these disorders are interrelated and may be expressed in the same individual, knowledge of mutual association is vital for earlier and more accurate diagnosis, thus avoiding unnecessary and expensive investigations. Treatment that is effective by clinical trials in one patient may not be effective in others, but the more that is known about the pathophysiology of CS, the more appropriate will be the treatment rendered and the more positive the outcomes.
Hypothalamic-pituitary-adrenal axis
The hypothalamic-pituitary-adrenal (HPA) axis is known to play a role in the coordinating of the body’s physiologic response to physical and emotional stressors. The HPA axis exhibits a circadian rhythm related to night/day, or sleep/awake, 24-hour cycles. Peak production of cortisol occurs in the early morning hours and decreases steadily to its lowest level in the evening. In addition to normal cortisol production, stress-induced secretion of cortisol can be added to the supply. Regulation of the HPA axis depends on key substances, such as hypothalamic corticotropin-releasing hormone (CRH) acting in synergy with vasopressin. They induce the release of adrenocorticotropic hormone (ACTH) from the anterior pituitary. Release of ACTH results in the production of corticosteroids from the adrenal glands that subsequently exert negative feedback on the hippocampus, the pituitary, and the hypothalamus through mineralocorticoid and glucocorticoid receptors. Other mediators that regulate the HPA axis include serotonin, norepinephrine, substance P, and IL-6 .
A study recently published by Ulrich-Lai demonstrated a relationship between increased nociceptor sensitivity during chronic pain and alterations in the limbic system, and a disassociation from HPA activation. The limbic system, which integrates behavior, is composed of the limbic forebrain, hippocampus, fornix, amygdala, medial thalamus, mamillary body, hypothalamus, and pituitary. The intimate relationship of the limbic lobe with the hypothalamus, and the inclusion of the neurostructures within the limbic system, have caused many to refer to the limbic system as the visceral brain . This system has a close, anatomic, and functional relationship to the hypothalamus. It is concerned intimately not only with emotional expression, but also with the genesis of emotions. In addition to its roles in olfaction and regulation of feeding behavior, the limbic system affects motivation and the expression of fear and rage. It exerts control over the autonomic nervous system by way of the pituitary gland and its target organs.
The close relationship of the limbic lobe to the hypothalamus allows it to influence control over the releasing factors located within the hypothalamus. When released, these factors start a chain of hormonal events that begins with stimulation of the pituitary gland and eventually results in a desired effect on a target organ. For example, stimulation of the pituitary gland causes the release of pituitary hormones that act on target glands to release target gland hormones. Target organs are influenced by the release of target gland hormones, such as cortisone and aldosterone from the adrenal cortex; testosterone, estrogen, and progesterone from the male and female gonads; thyroxine (T 4 ) from the thyroid glands; and somatomedin from the liver. These events continue to form a feedback loop as many of the hormones, in turn, affect brain function. The transduction of psychologic events into endocrine changes occurs by way of neuromodulators and neurotransmitters, which regulate the sensitivity of neurons to the stimulation, discharge, and conduction of nerve impulses from one neuron to another across the synaptic clef. Many such substances have been identified in the CNS, including biogenic amines like dopamine, norepinephrine, and serotonin, and acetylcholine, histamine, gamma-aminobutyric acid, and glycine, along with steroid and pituitary hormones and their hypothalamic and inhibiting factors .
Chronic pain may be considered a form of chronic stress. Patients experiencing this type of pain often exhibit disturbances in the HPA axis, including abnormal cortisol levels. Chronic pain patients report an increased incidence of depression and anxiety, stress-related disorders that frequently are accompanied by disturbances in the limbic system and in the HPA axis. Despite the fact that the literature supports a strong link between chronic pain, stress disorders, and limbic dysfunctions, the mechanisms underlying the effects of chronic pain on the HPA axis and the limbic system are not understood fully. The HPA axis is hyperactive during depression because of genetic factors or aversive stimuli that may occur during early development or adult life. The functioning of the hypothalamic-pituitary-thyroid axis, on the other hand, is inhibited during depression. Furthermore, a close interaction between the HPA axis and the hypothalamic-pituitary-gonadal axis exists. Organizing effects during fetal life, and activating effects of sex hormones on the HPA axis, have been reported. Such mechanisms may be the basis for a higher prevalence of mood disorders in women, as compared with men .
Studies of rats have shown that higher levels of cumulative corticosteroid exposure and extreme chronic stress induce neuronal damage that selectively affects hippocampal structure. The hippocampus has been shown to affect sleep and sleep hygiene dramatically .
Because various stressors activate the HPA axis, and because glucocorticoids are the end product of HPA axis activation, these hormones have been viewed as the physical embodiment of stress-induced pathology. It has been suggested that prolonged overproduction of glucocorticoids, whether as a result of ongoing stress or a genetic predisposition to HPA axis hyperactivity, brings about damage to certain brain structures (especially the hippocampus) essential for HPA axis restraint. Such damage, in turn, has been hypothesized to lead to a “feed-forward circuit,” in which ongoing stressors drive glucocorticoid production indefinitely. This theory has been called the “glucocorticoid cascade hypothesis” .
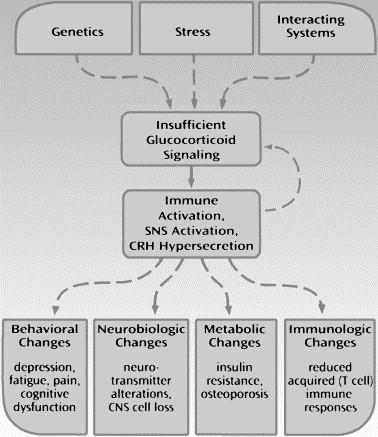
Despite the popularity of the glucocorticoid cascade hypothesis, increasing data provide evidence that in addition to glucocorticoid excess, insufficient glucocorticoid signaling may play a significant role in the development and expression of pathology in stress-related disorders . Insufficient glucocorticoid signaling is defined as any state in which the signaling capacity of glucocorticoids is inadequate to restrain relevant stress-response systems, either as a result of decreased hormone bioavailability (eg, hypocortisolism) or as a result of weakened glucocorticoid responsiveness (ie, secondary to reduce glucocorticoid receptor sensitivity). As defined, insufficient glucocorticoid signaling implies no specific mechanism or absolute deficiency, but focuses instead on the end point of glucocorticoid activity. A critical function of glucocorticoids is to shape and mobilize immune responses during stress . Virtually all stressors, including infection, physical trauma, and even psychologic insults, are associated with immune activation and release of proinflammatory cytokines such as interleukin-1 (IL-1) and interleukin-6 (IL-6). Because of their inhibitory effects on nuclear factor signaling pathways, glucocorticoids are the most potent anti-inflammatory hormones in the body. They serve to suppress the production and activity of proinflammatory cytokines during stressor exposure and to return the organism back to homeostasis after cessation of the stressor.
The relationship of insufficient glucocorticoid signaling to stress-related disorders has been proposed by Raison as effects stemming from environmental challenges (stress), genetic predisposition, and the influence of interacting systems, including neurotransmitter systems and the endocrine system. Insufficient glucocorticoid signaling is manifested most commonly as either hypocortisolism or impaired glucocorticoid responsiveness. Inadequate glucocorticoid activity, in turn, prevents stress-response systems, including the immune system, the sympathetic nervous system (SNS), and CRH from inhibitory control, which leads to unrestrained stress hyperreactivity. The resulting increased release of proinflammatory cytokines, catecholamines, and CRH leads to health consequences relevant to behavior, CNS function, metabolism, and immune function. Immune activation and cytokine release can then lead to further impairment in glucocorticoid signaling (feed-forward cascade) through direct inhibitory effects on glucocorticoid receptor function ( Fig. 3 ).