Introduction
The objective of this trial was to compare the survival rates of mandibular lingual retainers bonded with either chemically cured or light-cured adhesive after orthodontic treatment.
Methods
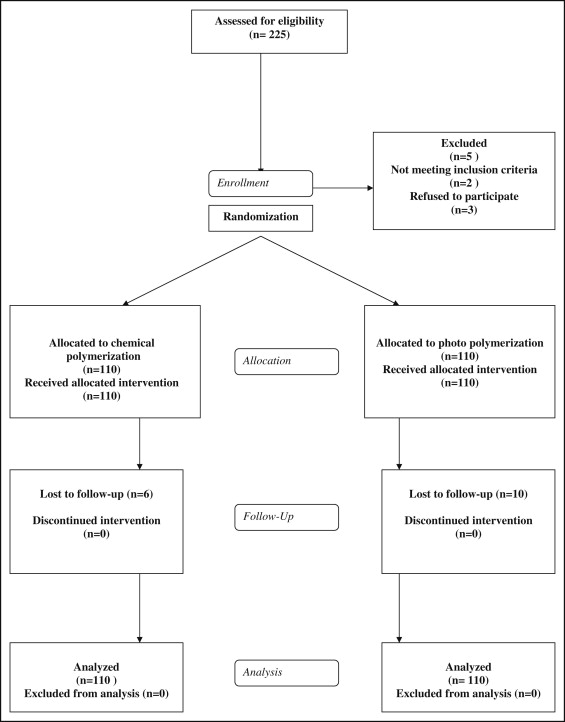
Patients having undergone orthodontic treatment at a private orthodontic office were randomly allocated to fixed retainers placed with chemically cured composite or light-cured composite. Eligibility criteria included no active caries, restorations, or fractures on the mandibular anterior teeth, and adequate oral hygiene. The main outcome was any type of first-time lingual retainer breakage; pattern of failure (adapted adhesive remnant index scores) was a secondary outcome. Randomization was accomplished with random permuted blocks of 20 patients with allocation concealed in sequentially numbered, opaque, sealed envelopes. Blinding was applicable for outcome assessment only. Patients were reviewed at 1, 3, and 6 months and then every 6 months after placement of the retainer until completion of the study. Data were analyzed using survival analysis including Cox regression; sensitivity analysis was carried out after data imputation for subjects lost to follow-up.
Results
Two hundred twenty patients (median age, 16 years; interquartile range, 2; range, 12-47 years) were randomized in a 1:1 ratio to either chemical or light curing. Baseline characteristics were similar between groups, the median follow-up period was 2.19 years (range, 0.003-3.64 years), and 16 patients were lost to follow-up. At a minimum follow-up of 2 years, 47 of 110 (42.7%) and 55 of 110 (50.0%) retainers had some type of failure with chemically cured and light-cured adhesive, respectively (log-rank test, P = 0.35). Data were analyzed on an intention-to-treat basis, and the hazard ratio (HR) was 1.15 (95% confidence interval [CI], 0.88-1.70; P = 0.47). There was weak evidence that age is a significant predictor for lingual retainer failures (HR, 0.96; 95% CI, 0.93-1.00; P = 0.08). Adhesive remnant index scoring was possible for only 66 of the 102 (64.7%) failures and did not differ between composites (Fisher exact test, P = 0.16). No serious harm was observed other than gingivitis associated with plaque accumulation.
Conclusions
The results of this study indicated no evidence that survival of mandibular lingual retainers differs between chemically and light-cured adhesives. The overall failure rate was 46.4%; however, this included any type of failure, which may have exaggerated the overall failure rate.
The guarantee of long-term stability after orthodontic treatment has been a fruitless quest since the specialty began. Posttreatment changes appear to be due to a combination of maturational changes and relapse. Acclaimed research has demonstrated that changes after orthodontics are unpredictable ; if stability is to ensue, only perfect retention can guarantee this. In view of variable compliance with removable retention regimens, fixed retention has become paramount since its inception in the 1970s, with up to one third of practitioners in the United States and 97% in The Netherlands routinely using mandibular fixed retainers.
Fixed retainers have proven fallible, however, with problems stemming from distortion or residual activity of the wire and the potential for periodontal consequences related to plaque stagnation, although fixed retainers have also shown compatibility with periodontal health. A significant problem continues to relate to bond failures, estimated at 6% to 25%, depending on the placement technique and the observation period.
Fixed retainers have evolved from preliminary designs typically involving large-diameter stainless steel round wires (0.030-0.032 in) bonded to the canines, to narrower, braided, or coaxial round wires, or reduced cross-section rectangular wires of various compositions and resilience, bonded to all mandibular anterior teeth. More recently, alternatives including fiber-reinforced materials and alumina ceramic retainers have been tested. A transition from the routine use of chemically cured composites to placement with light-cured polymerization has taken place over the past 2 decades. Although light-cured materials offer longer working times and improved moisture control, no randomized controlled trial has been published investigating the importance of these theoretical advantages. In this study, we aimed to compare the survival of mandibular lingual retainers placed using either chemical or photo polymerization after orthodontic treatment.
Material and methods
This was a parallel-group, randomized, active-controlled trial with a 1:1 allocation ratio. Consecutive patients who had completed orthodontic treatment with fixed appliances were recruited at the private practice of the first author (N.P.) from April 2009 to November 2010. The following selection criteria were applied: no active caries, restorations, fractures on the mandibular anterior teeth, or periodontal disease; and adequate oral hygiene. Subjects were excluded if they were unwilling to be assigned to any of the approaches or had any abnormal oral or medical condition contraindicating fixed retention. Consent was obtained from the patients (and the parents if the patients were adolescents) before their recruitment.
Two hundred twenty patients were randomized toretention involving a lingual retainer placed with either chemically cured composite or light-cured composite. Randomization was accomplished using the “- ralloc -” command in Stata software (StataCorp, College Station, Tex) in random permuted blocks of 20 patients, ensuring equal distribution in the 2 groups. Allocation concealment was achieved with sequentially numbered, opaque, sealed envelopes containing the treatment allocation cards, which were prepared before the trial. Baseline information was written on the outside before opening the envelope. The practice manager was responsible for opening the next envelope in sequence and implementing the randomization process.
After their orthodontic treatment, the patients were seen by their general dentist for supragingival debridement, and the appointment for the lingual retainer was confirmed. All patients received a soft bonded lingual retainer of 0.022-in (Tru-Chrome multi-stranded wire; Rocky Mountain Orthodontics, Denver, Colo) that was fabricated intraorally. A cheek retractor was placed; the lingual surfaces of the 6 mandibular anterior teeth from canine to canine were pumiced, rinsed, dried, and acid-etched with 37% phosphoric acid. The etched surfaces were subsequently rinsed and carefully dried, a cotton roll was placed in the vestibule, and 3 pieces of waxed dental floss were passed through the interproximal surfaces between the canines and the lateral incisors, and between the central incisors, forming loops to stabilize the retainer wire. The wire was passed through the loops; gentle labial traction was applied to the dental floss to secure the wire passively in place. Every effort was made to position the wire passively across the lingual surfaces of the teeth. The enamel surfaces were checked for moisture and redried as required, and small amounts of liquid and paste adhesives were placed on each tooth covering the wire.
In the chemical polymerization group, Maximum Cure 2-part liquid adhesive (Reliance Orthodontic Products, Itasca, Ill) was mixed and applied on the wire and the teeth, and Excel 2-part paste (Reliance Orthodontic Products) was mixed, loaded on a syringe dispenser, and applied. The dental floss was removed after 7 minutes. In the photo polymerization group, a light-cured liquid (Assure; Reliance Orthodontic Products) and paste in 2 layers (Flow-Tain; Reliance Orthodontic Products) were placed on the wire and adjacent enamel and were light cured for 9 seconds per tooth with a plasma light (Ortholite; 3M Unitek, Monrovia, Calif). After placement of the bonded wire, all patients were instructed to maintain meticulous dental hygiene and to visit their dentist every 6 months for monitoring of the periodontal conditions.
At baseline, the following information was collected: age, sex, Angle classification, and gingival index, and a subjective 3-level score of cooperation (poor, average, or good) was assigned to each patient based on the practitioner’s impressions during the orthodontic therapy. The main outcome was any first-time failure of the lingual retainer. The secondary outcome was the pattern of failure based on the adhesive remnant index (0, no retained resin on tooth surface; 1, <50% retained resin on tooth surface; 2, >50% retained resin on tooth surface; and 3, all resin retained on tooth surface).
The patients were advised to visit the orthodontist initially at 1, 3, and 6 months after retainer placement, followed by scheduled appointments at 12, 18, and 24 months after the initial placement of the bonded retainer to evaluate its integrity. In case of breakage, the patients were instructed to call and visit the office immediately. The subsequent appointment to review the retainer was scheduled in advance to ensure regular follow-up; reminders were sent in case of appointment failures. When scheduled appointments were unfeasible, particularly approaching the end of the trial, an assessment of retainer integrity was made over the telephone. During the telephone interview, the patient was asked to the best of his or her knowledge whether the lingual retainer was intact and bonded on all teeth, loose on any tooth, or completely lost. When breakages were reported, it was not possible to assess the adhesive remnant index score. Blinding of either patient or operator was not possible; however, assessment was blind because it was not possible to distinguish between the treatment groups.
Calculation of sample size was based on the ability to detect a clinically relevant difference in the risk of first-time failure (primary outcome) of 20% between the 2 trial arms (15% vs 35% with α = 0.05 and power of 85%). Foek et al found a 35% failure rate for light-cured lingual retainers; we used this value as our reference for the sample calculation. This calculation indicated that 93 participants were required in each arm; this was rounded up to 110 to account for losses to follow-up.
Statistical analysis
Comparisons of the survival of lingual retainers bonded with the 2 techniques were carried out with statistical methods for survival analysis. The log-rank test was used and Kaplan-Meier plots were produced. Hazard ratios (HR) and associated 95% confidence intervals (CI) were calculated using Cox regression modeling. The Nelson-Aalen plot was used to assess the proportional hazards assumption. A sensitivity analysis was carried out comparing a data set with and without imputed outcome data for patients lost to follow-up. Imputations were carried out under the missing at random assumption using the “-mi-” family of commands adapted for Cox regression. Missing outcomes were imputed using the variable intervention type; sex and age were imputed via logistic regression. All analyses were conducted with Stata software (version 12.01; StataCorp).
Results
Two hundred twenty patients (median age, 16 years; interquartile range, 2 years; range, 12-47 years) were randomized in a 1:1 ratio to either chemical or light curing; 16 patients were lost to follow-up ( Fig 1 ). Baseline characteristics were similar in both groups ( Table I ) with a median follow-up period of 2.19 years (range, 0.003-3.64 years; Table II ). Two years after entry of the final patient, 47 of 110 (42.7%) and 55 of 110 (50.0%) retainers bonded with chemically cured and light-cured adhesive had failed, respectively. The primary analysis was carried out on an intention-to–treat basis involving all patients randomized after imputation of missing data.
| Total n = 220 Median or % |
IQR | Excel n =110 Median or % |
IQR | Flow-Tain n = 110 Median or % |
IQR | |
|---|---|---|---|---|---|---|
| Demographic characteristics | ||||||
| Age (y) | 16.0 | 2 | 16.0 | 2 | 15.0 | 2 |
| Sex | ||||||
| Female | 72.7 | 71.8 | 73.6 | |||
| Male | 27.3 | 28.2 | 26.4 | |||
| Clinical characteristics | ||||||
| Gingival index | 1.5 | 1 | 1.3 | 1-2 | 1.5 | 1 |
| Cooperation | ||||||
| Bad | 26.4 | 27.3 | 25.5 | |||
| Average | 55.9 | 59 | 52.7 | |||
| Excellent | 17.7 | 13.7 | 21.8 | |||
| Angle Class | ||||||
| I | 59.2 | 56.4 | 62 | |||
| II | 39 | 40.9 | 37 | |||
| III | 1.8 | 2.7 | 1 | |||
| Risk factor | Total number (%) | No. of failures observed (%) | Follow-up period in person years | Median (y) | Range (y) |
|---|---|---|---|---|---|
| Adhesive | |||||
| Excel | 110 (50) | 47 (42.7) | 206.30 | 2.22 | 0.003-3.64 |
| Flow-Tain | 110 (50) | 55 (50.0) | 201.68 | 2.16 | 0.005-3.58 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


