Positive airway pressure can be effective for OSA treatment but is not effectively used by many patients. Surgical reconstruction of the airway is appropriate for patients who are not otherwise effectively treated or as first-line treatment for patients with focal airway lesions. For surgical planning, examination schemes of the awake patient, as well as sleep endoscopy may be used. Nasal surgery may facilitate treatment using positive airway pressure or oral appliances or to improve quality of life. Pharyngoplasty and tongue base techniques for therapeutic upper airway reconstruction may be performed staged or simultaneously. Current and future approaches are described.
Rationale for surgery
Obstructive sleep apnea syndrome (OSA) is a common and serious medical disorder that remains difficult to treat. OSA is characterized by repetitive episodes of upper airway obstruction leading to hypoxemia and autonomic and cortical arousals. The consequences of untreated OSA are significant and include increased risk of cardiovascular disease such hypertension, atrial fibrillation, stroke, as well as diabetes, neurocognitive dysfunction, poor quality of life, motor vehicle accidents, and premature death. Although efficacious OSA treatments such as continuous positive airway pressure (CPAP) are available, many patients do not accept chronic, nightly use of a device for sleep, and many others do not adhere to such therapy long term. Surgical airway upper reconstruction is thus appropriate for certain patient populations.
The goal of surgical and medical treatment of OSA is to provide major clinical improvement and to promote survival of the patient. Because OSA is a chronic disease, cure is uncommon, and lack of cure does not imply failure. CPAP is considered a clinically effective treatment of OSA even though partial adherence is common, and possibly inadequate. An apnea-hypopnea index (AHI) greater than 5 was shown to be present in as many as 73% of fully CPAP-adherent patients. The primary goal of surgery is to improve clinical outcome for a chronic disease and secondarily to improve the AHI, as it is a surrogate outcome measure.
Surgical treatment of OSA has been shown to result in improved survival and function in well-controlled studies. In an analysis of more than 20,000 patients with OSA in Veteran’s Administration, controlled for comorbidities, survival was greater with surgery than with CPAP. Long-term survival was also shown to be improved with surgery in additional studies. Cardiovascular outcome was improved in patients treated with uvulopalatopharyngoplasty (UPPP). UPPP was shown to be associated with diminished motor vehicle accident risk, with a lowering of the relative risk from 9.6 to 1.3. Surgery for OSA has resulted in improved quality of life, alertness, and reaction time.
The AHI is a surrogate outcome measure for OSA, but is nonetheless used for objective treatment outcome assessment. For surgical reconstruction for the airway, data analysis is complex given the heterogeneity of procedures and mostly small series studies. Pooling of data is necessary to assess results for specific surgical techniques and for multilevel surgical interventions. In a systematic review, surgical success, as defined by reduction in the AHI of 50% or more and an AHI of less than 20, was 66%. In an evidence-based medicine review of hypopharyngeal procedures for OSA, the success rate for AHI was 35% to 62% and improvement in quality of life and daytime somnolence were also noted.
Which Patients Should Undergo Surgery?
Disease severity
Which patients are the best candidates for surgical intervention, those with milder or more severe OSA? Some have suggested that surgery is more suitable for mild to moderate OSA, based on AHI criteria for severity, and in some cases series, patients with more severely increased AHI scores had a lower rate of surgical success, defined only by AHI reduction. However, in other studies, preoperative AHI severity did not correlate with successful reduction of the AHI, and anatomic staging was more predictive. Another consideration is that otherwise untreated patients with moderate to severe OSA are at higher risk for adverse sequelae, and therefore have the greatest need for treatment using surgery.
Discrete anatomic lesions
Patients with discrete anatomic loci that are amenable to surgery, such as enlarged palatine tonsils, are good candidates for surgery as the primary treatment. In the pediatric population, tonsillectomy and adenoidectomy are the recommended first-line therapies for OSA. Likewise, in a young adult with palatine tonsillar hypertrophy, it is more reasonable to perform tonsillectomy than to instruct the patient to use an appliance for decades. Hypertrophic lingual tonsils, at the tongue base, are also readily amenable to simple surgical resection with resultant airway enlargement. Lingual tonsils are most commonly identified by flexible fiberoptic endoscopy performed by an otolaryngologist, and are also readily apparent on magnetic resonance imaging (MRI). Infrequently, obstructive lesions such as antrochoanal polyp, nasal or nasopharyngeal tumors, pharyngeal or laryngeal lesions, and goiters may also mediate OSA and may be surgically resected for treatment.
Nasal obstruction
Patients with nasal obstruction may find it more difficult to tolerate CPAP and oral appliance therapy. For oral appliance therapy, nasal obstruction may compromise the ability to use an appliance that partially occludes the mouth. Patients who did not respond to oral appliance therapy were shown to have higher nasal resistance compared with responders. Women with complaints of nasal obstruction had an odds radio for successful treatment using oral appliances of only 0.1. For CPAP use, preferential oral breathing and nasal obstruction have also been shown to be risk factors for low use and acceptance. Nasal surgery has been shown to result in lower CPAP levels for treatment and improved adherence in small studies. Thus nasal surgery may be used to facilitate medical therapy for OSA.
Is nasal surgery appropriate for definitive therapy for OSA? When used as the only surgical intervention, the overall success rate of septal and turbinate surgery, as defined by AHI reduction of 50% and to a level less than 20 per hour, is about 17%. Response to nasal surgery may depend on whether there is a postoperative shift from oral breathing to more nasal breathing and absence of other contributory loci for airway obstruction, often present in patients with OSA. Nasal surgery has been shown to reduce sleepiness and improve quality of life for patients with OSA, as measured by the Epworth Sleepiness Score (ESS) and Short Form 36 inventory. These quality-of-life scores are relevant to patients with OSA and do not correlate with the AHI. Nasal surgery is thus often used in combination with pharyngeal surgery, primarily to improve quality of life.
Upper airway evaluation
The upper airway is a complex space, whose dimensions and morphology are determined by skeletal and soft tissues. For anatomic analysis for surgery, it is important to conceptualize the skeletal structural container as well as the soft tissue contents. Patients with OSA have been shown to have retruded maxillae, enlarged tongues, and thick pharyngeal walls, but the presence and magnitude of anatomic features vary between patients. Hence, staging systems that describe the anatomic features are needed to target surgical intervention.
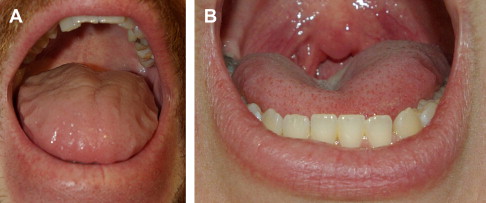
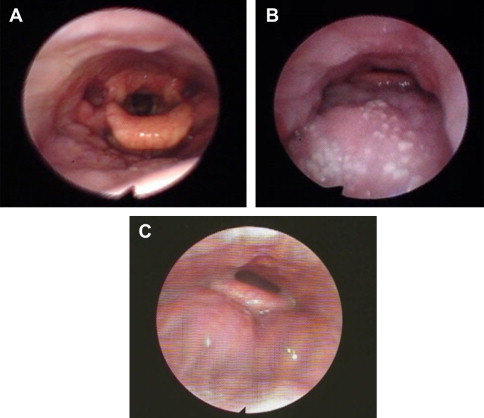
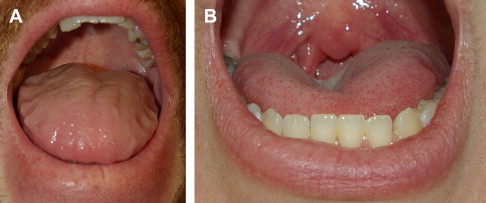
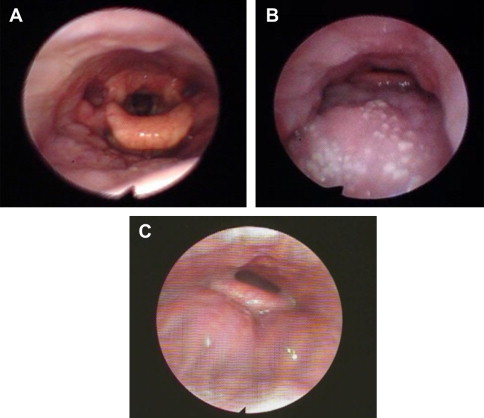
Awake, office examination is used to assess the skeletal and soft tissue features. Retrognathia, maxillary retrusion, and hard palate width are noted. The presence of oral and pharyngeal macroglossia is assessed using direct examination and fiberoptic endoscopy in the supine, end-expiratory state. The relative position of the oral tongue, presence of crenations, and central grooving are noted as markers of relative macroglossia ( Fig. 1 ). The width of the oropharynx, presence of soft palatal webbing, and tonsillar size are assessed. The tongue base is examined for lingual tonsillar size the presence of lesions, glossoptosis, and epiglottic morphology ( Fig. 2 ). Some surgeons use the Mueller maneuver, consisting of negative pressure against a closed mouth and nose to assess for hypopharyngeal collapse.
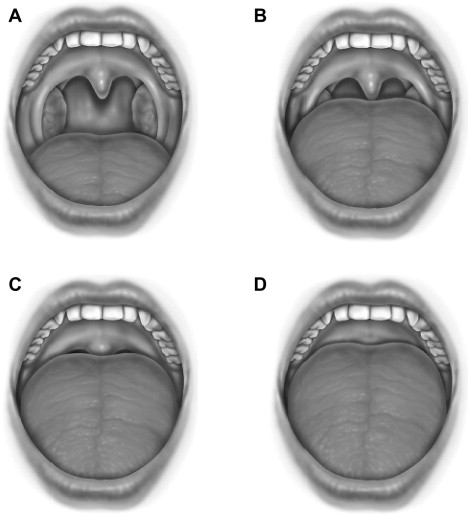
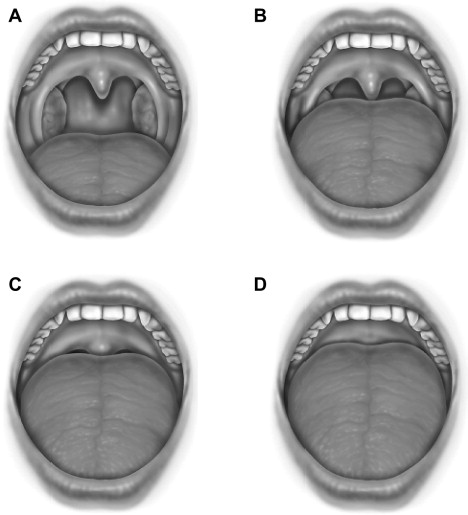
A commonly used surgical staging system is the Friedman tongue position, a modification of the Malampatti scale, in which the tongue position is assessed in reference to the soft palate ( Fig. 3 ). When the tongue position is combined with tonsillar size and body mass index (BMI), the Friedman staging system may be used to predict patient success with traditional UPPP surgery. Patients with smaller tongues and larger tonsils have a high rate of success, as defined by the AHI, for UPPP with tonsillectomy. However, this system does not describe the pharyngeal morphology or airway shape and does not direct specific airway procedures; it only specifies a pharyngeal level.
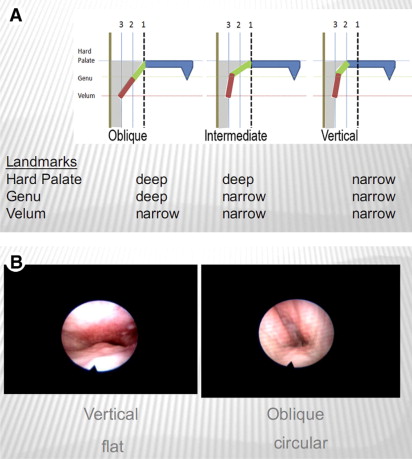
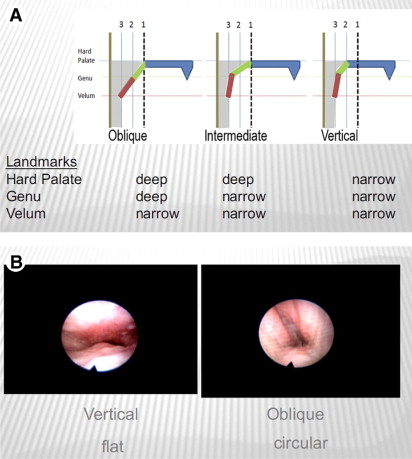
A more recent anatomic system for the awake patient was proposed by Woodson, incorporating the luminal shape and underlying structural features of the upper airway ( Fig. 4 ). For example, the retropalatal pharyngeal airway is assessed in terms of its width, anteroposterior length, and overall shape. Taken together with knowledge of the structures that determine different pharyngeal shapes, the surgeon may then elect to perform a specific palatopharyngoplasty procedure variant. For example, if a flat/vertical airway shape is noted, consistent with anteroposterior narrowing of the superior retropalatal airway, then procedures that advance the superior palate anteriorly are selected, rather than a distal palate, soft tissue UPPP. If a circular/deep airway shape is noted, then the surgeon may select procedures that modify the distal soft palate and the thickened lateral pharyngeal wall, as described later in this article.
Drug-induced Sleep Endoscopy
To better approximate the airway examination during sleep, drug-induced sleep endoscopy (DISE) may be used for preoperative assessment. Infusion of agents such as propofol or midazolam is used to induce snoring and airway instability, as muscle tone is reduced with sedation. Snoring occurs in patients with OSA but not in control subjects, and the technique has been shown to result in similar AHI levels as in true sleep except that rapid eye movement is diminished or absent in DISE and thus may not be as reliable for REM-dependent OSA. Using sedated, sleep endoscopy, operative management and procedural selection has been reported to significantly change from that planned using the awake examination. DISE has been also used to assess residual loci of obstruction after unsuccessful initial upper airway surgery and potentially predict oral appliance treatment success. Recently, Hohenhorst and colleagues described a classification, to uniformly describe DISE patterns of obstruction at the velum, oropharynx, tongue base, and epiglottis (VOTE).
Perioperative Management
Patients with OSA may be at higher risk when undergoing surgery, especially on the upper airway. Before surgery, patients should undergo a thorough medical optimization given the increased risk of cardiovascular disease with OSA. Communication or consultation with the anesthesiologist is recommended because patients with OSA are often more difficult to intubate and may have a lower threshold to opiates or sedatives for respiratory depression and airway collapse. After surgery, nonsupine positioning and head elevation are preferable. Pain should be adequately controlled but use of opiates should be minimized. A multimodal regimen consisting of systemic steroids, gabapentinoids, acetaminophen, cyclooxygenase-2 selective inhibitors, antibiotics, and tissue cooling may be used to treat and prevent pain, to lower the opiate requirement for analgesia. Patients are typically observed several hours or in an inpatient setting, depending on specific procedures performed, medical comorbidities, and OSA severity.
Upper airway evaluation
The upper airway is a complex space, whose dimensions and morphology are determined by skeletal and soft tissues. For anatomic analysis for surgery, it is important to conceptualize the skeletal structural container as well as the soft tissue contents. Patients with OSA have been shown to have retruded maxillae, enlarged tongues, and thick pharyngeal walls, but the presence and magnitude of anatomic features vary between patients. Hence, staging systems that describe the anatomic features are needed to target surgical intervention.
Awake, office examination is used to assess the skeletal and soft tissue features. Retrognathia, maxillary retrusion, and hard palate width are noted. The presence of oral and pharyngeal macroglossia is assessed using direct examination and fiberoptic endoscopy in the supine, end-expiratory state. The relative position of the oral tongue, presence of crenations, and central grooving are noted as markers of relative macroglossia ( Fig. 1 ). The width of the oropharynx, presence of soft palatal webbing, and tonsillar size are assessed. The tongue base is examined for lingual tonsillar size the presence of lesions, glossoptosis, and epiglottic morphology ( Fig. 2 ). Some surgeons use the Mueller maneuver, consisting of negative pressure against a closed mouth and nose to assess for hypopharyngeal collapse.
A commonly used surgical staging system is the Friedman tongue position, a modification of the Malampatti scale, in which the tongue position is assessed in reference to the soft palate ( Fig. 3 ). When the tongue position is combined with tonsillar size and body mass index (BMI), the Friedman staging system may be used to predict patient success with traditional UPPP surgery. Patients with smaller tongues and larger tonsils have a high rate of success, as defined by the AHI, for UPPP with tonsillectomy. However, this system does not describe the pharyngeal morphology or airway shape and does not direct specific airway procedures; it only specifies a pharyngeal level.
A more recent anatomic system for the awake patient was proposed by Woodson, incorporating the luminal shape and underlying structural features of the upper airway ( Fig. 4 ). For example, the retropalatal pharyngeal airway is assessed in terms of its width, anteroposterior length, and overall shape. Taken together with knowledge of the structures that determine different pharyngeal shapes, the surgeon may then elect to perform a specific palatopharyngoplasty procedure variant. For example, if a flat/vertical airway shape is noted, consistent with anteroposterior narrowing of the superior retropalatal airway, then procedures that advance the superior palate anteriorly are selected, rather than a distal palate, soft tissue UPPP. If a circular/deep airway shape is noted, then the surgeon may select procedures that modify the distal soft palate and the thickened lateral pharyngeal wall, as described later in this article.
Drug-induced Sleep Endoscopy
To better approximate the airway examination during sleep, drug-induced sleep endoscopy (DISE) may be used for preoperative assessment. Infusion of agents such as propofol or midazolam is used to induce snoring and airway instability, as muscle tone is reduced with sedation. Snoring occurs in patients with OSA but not in control subjects, and the technique has been shown to result in similar AHI levels as in true sleep except that rapid eye movement is diminished or absent in DISE and thus may not be as reliable for REM-dependent OSA. Using sedated, sleep endoscopy, operative management and procedural selection has been reported to significantly change from that planned using the awake examination. DISE has been also used to assess residual loci of obstruction after unsuccessful initial upper airway surgery and potentially predict oral appliance treatment success. Recently, Hohenhorst and colleagues described a classification, to uniformly describe DISE patterns of obstruction at the velum, oropharynx, tongue base, and epiglottis (VOTE).
Perioperative Management
Patients with OSA may be at higher risk when undergoing surgery, especially on the upper airway. Before surgery, patients should undergo a thorough medical optimization given the increased risk of cardiovascular disease with OSA. Communication or consultation with the anesthesiologist is recommended because patients with OSA are often more difficult to intubate and may have a lower threshold to opiates or sedatives for respiratory depression and airway collapse. After surgery, nonsupine positioning and head elevation are preferable. Pain should be adequately controlled but use of opiates should be minimized. A multimodal regimen consisting of systemic steroids, gabapentinoids, acetaminophen, cyclooxygenase-2 selective inhibitors, antibiotics, and tissue cooling may be used to treat and prevent pain, to lower the opiate requirement for analgesia. Patients are typically observed several hours or in an inpatient setting, depending on specific procedures performed, medical comorbidities, and OSA severity.
Surgical Procedure Selection
Although UPPP is the most common procedure performed for OSA, the range of upper and lower pharyngeal procedures that are used to address the upper airway is extensive. A nonexhaustive list in presented in Table 1 , in which procedures are grouped based on sites. The choice of procedure depends on patient features, the surgeon’s expertise, and patient preferences. There is no widely accepted protocol in the sleep surgery community for airway reconstruction. The Stanford protocol of Riley and Powell has been of great value but is limited because it only includes UPPP, genioglossus advancement, hyoid suspension as phase I, maxillomandibular advancement as phase II, and because this multiprocedure protocol is of high intensity and morbidity.
| Site | Procedure |
|---|---|
| Nasal/nasopharyngeal | Septoplasty |
| Inferior turbinate reduction | |
| Nasal valve repair | |
| Nasal valve suspension | |
| Nasal polypectomy | |
| Adenoidectomy | |
| Oral | Tongue ablation |
| Lingualplasty | |
| Excision of oral tori | |
| Oropharyngeal | Uvulopalatopharyngoplasty |
| Lateral pharyngoplasty | |
| Palatal advancement pharyngoplasty | |
| Z-palatopharyngoplasty | |
| Relocation pharyngoplasty | |
| Anterior pharyngoplasty | |
| Tonsillectomy | |
| Hypopharyngeal | Partial glossectomy |
| Radiofrequency tongue ablation | |
| Lingual tonsillectomy | |
| Genioglossus advancement | |
| Tongue suspension | |
| Epiglottoplasty | |
| Neck | Hyoid suspension |
| Tracheotomy | |
| Multilevel | Maxillomandibular advancement |
Patients may undergo staged or concurrent procedures for upper airway reconstruction depending on their personal preferences or those of their surgeon. From a safety perspective, performance of nasal with upper pharyngeal surgery does not seem to increase the risk for serious complications but concurrent upper pharyngeal and hypopharyngeal surgeries are of higher risk. From the patient’s perspective, concurrent surgery may be preferred given the convenience of only 1 operative event and work hiatus. However, others may prefer staged surgeries that may be performed ambulatory, with less pain, and more rapid return to work. Another reason why staged surgery may be preferable is that the preoperative assessment of procedures needed for effective therapy is not always accurate and that a single procedure, rather than multiple procedures, may suffice.
The difficulty in predicting a priori the extent of surgery needed may be related to postoperative changes in pharyngeal pressures, anatomic palate-tongue interaction, or neuromuscular tone differences not apparent during an examination while awake. Surgery on the upper pharynx may affect the lower pharynx and vice versa. In patients who underwent palatal surgery, the degree of subpalatal obstructions was lower after surgery, as measured by manometry. The potential mechanism may be that, after alleviation of the upper pharyngeal critical obstruction, lower overall negative pharyngeal pressures are generated and less tongue base obstruction occurs. An additional palatal-tongue relation is anatomic. Recent study showed anatomic connection of the superior constrictor muscle with the tongue’s transversus intrinsic muscle, hence tongue or palatal modification may affect the latter as well.
The author’s current preference is to perform staged surgeries rather than more intensive multilevel concurrent procedures. Although a prior protocol consisting of UPPP, genioglossus advancement, hyoid suspension, and radiofrequency treatment of the tongue base resulted in symptomatic treatment and AHI reduction to less than 20 with greater than 50% reduction from baseline for 74% of patients of an advanced Friedman stage, the approach was associated with high morbidity. Procedures are now performed staged, and patients with moderate to severe OSA are observed overnight for airway and cardiovascular monitoring, and treated using a multimodal analgesia protocol. A palatopharyngoplasty procedure is usually performed first, because the upper pharyngeal airway is the narrowest site in the upper airway and, with treatment, downstream hypopharyngeal collapse could diminish. About 3 months following surgery, patients are assessed using sleep studies for the need for subsequent intervention before proceeding with additional surgery.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


