Introduction
The aim was to evaluate the short-term success rate of combined orthodontic-orthognathic surgical correction of anterior open bite.
Methods
Fifteen patients (ages, 15-28 years) with open bite treated with a combined orthodontic-surgical approach were examined. Lateral cephalograms from before treatment, after treatment, and after an average of 18 months (range, 10-26 months) of retention were evaluated. Overbite was classified as normal (2-3.5 mm), borderline (0-1.5 mm), or relapse (<0 mm), and overjet as normal (2-3.5 mm) or relapse (≥4 and ≤1.5 mm).
Results
The average overbite was –3.2 mm before treatment, 1.8 mm after treatment, and 1.3 mm after retention. During active treatment, overbite and overjet were normalized in 53.3% and 66.7% of the subjects, respectively. After the retention period, 1 patient (6.7%) showed a negative overbite, whereas a borderline overbite was found in 53.3% of the subjects. Overjet relapsed in 40% of the subjects. Only 40% of the patients had a completely successful treatment with incisal contact and normal overjet and overbite.
Conclusions
Orthodontic-surgical treatment of anterior open bite improves the overbite, but an excellent treatment outcome with normal overjet and overbite and proper incisal contact was achieved in only 40% of the subjects.
Successful treatment of skeletal open bite is considered a challenge. Attempts to control maxillary development and prevent eruption of the posterior teeth during growth are often counteracted by late adolescent growth changes, thus resulting in a relatively high percentage of adult open-bite treatments.
In adult patients with milder open bites, camouflage therapy (incisor extrusion and posterior teeth intrusion) is a possible treatment option. On the other hand, in adult patients with severe open bites, combined orthodontic-orthognathic treatment with LeFort I impaction or bimaxillary surgery aims at correcting the jaw inclination and reducing the excessive anterior facial height to achieve good facial esthetics as well as a functional occlusion. However, relapse even after combined orthodontic-orthognathic treatment does occur.
A functional occlusion that includes among other characteristics a correct interincisal relationship with incisal overlap and interincisal contact is a general orthodontic treatment goal. Lack of interincisal contact despite a positive overbite (OB)—a so-called open bite with OB—was first described by Moyers. It was found to be an indicator for habits and a prognostic factor for open-bite stability.
However, most open-bite studies evaluated only OB as a parameter for success and stability. Only Denison et al differentiated real open bites and open bites with OB at pretreatment, but whether interincisal contact could be established and maintained was unfortunately not described.
Therefore, the aim of this study was to evaluate the short-term success rate of combined orthodontic-orthognathic surgical correction of anterior open bite, giving special emphasis to interincisal relationship and contact.
Material and methods
Between 1995 and 2008, a total of 41 open-bite patients were planned for a combined orthodontic-orthognathic surgical approach at the Department of Orthodontics of the University of Giessen in Germany. Twenty-six patients were excluded from the study because of no surgical treatment desired (n = 22), syndromes (n = 2), and incomplete documentation (n = 2). The remaining 15 Angle Class I (n = 1), Class II (n = 9), and Class III (n = 5) open-bite patients (9 male, 6 female) with a mean pretreatment age of 19.9 ± 4.03 years (range, 15-28 years) were examined retrospectively. All patients had undergone presurgical and postsurgical orthodontic treatment with fixed appliances. The system used for all patients was a Tip-Edge bracket system (TP Orthodontics, LaPorte, Ind) with a 0.22-in slot. No patient received any myofunctional therapy either during or after treatment. Lateral cephalograms from before treatment (T1), after orthodontic-surgical treatment (T2), and after retention—ie, after appliance removal—(T3) were evaluated. The average length of the retention period was 18 months (range, 10-26 months). All radiographs were traced and evaluated by the same investigator (U.J.). No correction for linear enlargement (approximately 8%) was performed.
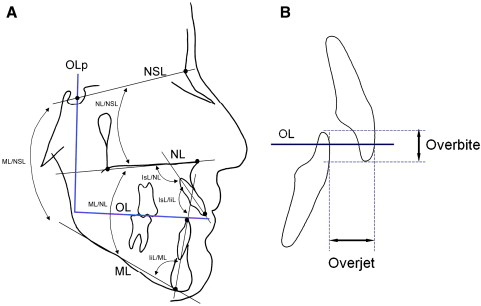
Standard cephalometric parameters, overjet (OJ) and OB, were measured ( Fig 1 ). OB was classified as normal (2-3.5 mm), borderline (0-1.5 mm), or relapse (<0 mm), and OJ as normal (2-3.5 mm) or relapse (≥4 and ≤1.5 mm). Furthermore, interincisal contact was evaluated visually.
Results
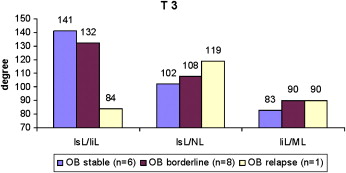
Average OB values were –3.2 mm at T1, 1.8 mm at T2, and 1.3 mm at T3. During active treatment (T1-T2), OB and OJ were normalized in 53.3% and 66.7% of the subjects, respectively. At T3, 1 patient (6.7%) showed a negative OB, whereas a borderline OB was found in 53.3% of the subjects ( Fig 2 ). OJ relapsed in 40% of the subjects.
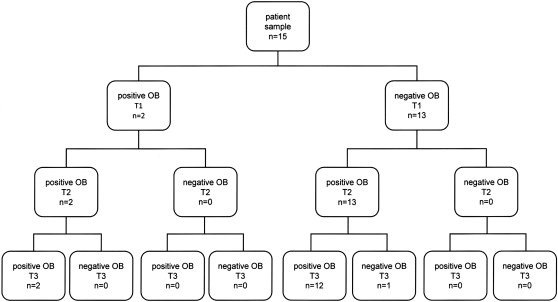
An interincisal contact was found in 53.3% (at T2) and 46.6% (at T3) of the patients, respectively. However, only 40% of the patients had a completely successful treatment with interincisal contact and normal OJ and OB.
Considering the skeletal parameters, before active orthodontic treatment, 80% of the subjects had a hyperdivergent (>38°) vertical jaw base relationship with an average mandibular plane angle (ML/NSL) of 43.6°. During the retention period (T2-T3), the ML/NSL increased in 40% of the subjects. Half of these patients exhibited a stable OB, 33.3% were borderline, and 1 had a negative OB (16.7%). The interjawbase angle (ML/NL) first decreased during active treatment (T1-T2) from 35.5° to 31.8°, but increased slightly to 32.9° thereafter. The maxillary plane angle (NL/NSL) was relatively stable, increasing from 8.3° to 11.1° (T1-T2) and decreasing to 10.2° (T3).
Patients with a borderline or relapsed OB after retention exhibited more proclined incisors than did those with a stable OB ( Fig 3 ). Correspondingly, the interincisal angle (IsL/IiL) at T3 was greatest in patients with a stable OB (140.8°) and smallest in those with OB relapse (84°).