Introduction
The objectives of this study were to evaluate the prevalence and long-term behavior of extraction space reopening in patients with Class I malocclusion and to identify some associated factors.
Methods
A sample of 43 patients met the inclusion criteria. Dental casts at the onset of treatment, after treatment, and 1 and 5 years after debonding were used. Initial and final cephalometric radiographs were used to measure the amount of incisor retraction. Cochran tests were used to compare the numbers of open and closed extraction spaces after treatment and at 1 and 5 years after debonding ( P <0.05). Initial incisor crowding, amounts of anterior retraction, and angulations between the canines and the second premolars were compared between patients with and without space reopening with t tests.
Results
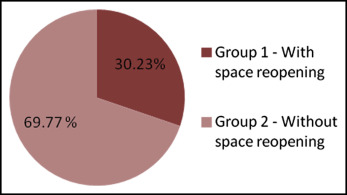
Of the sample, 30.23% had extraction space reopening. The frequency of open spaces significantly increased between the final and the 1-year posttreatment dental casts and decreased between the casts at 1 and 5 years posttreatment. Patients with space reopening had less initial anterior crowding and greater amounts of mandibular incisor retraction during treatment.
Conclusions
There was a high prevalence of space reopening 1 year after treatment. However, these spaces tended to decrease by 5 years after treatment.
Highlights
- •
Extraction space reopened in about 30% of the subjects by 5 years.
- •
Most of the reopening occurred in the first year after treatment.
- •
Space reopened in patients with less anterior crowding and more mandibular incisor retraction.
Posttreatment stability remains a challenge in orthodontics because long-term preservation of the teeth in their new positions is unpredictable. Angle stated that relapse would occur if normal occlusion was not achieved during treatment. Studies have demonstrated that even in patients finished with an adequate static and functional occlusion, there is a tendency for some relapse. Instability is individual and may be associated with other aspects such as severity and type of malocclusion, mechanics, the patient’s compliance, growth, and the adaptability of the hard and soft tissues.
An undesirable relapse expression often observed in clinical practice is the reopening of extraction spaces. Space reopening in extraction sites can cause periodontal issues related to food impaction and overload of occlusal forces. In addition, it may impair esthetics mainly when it occurs in the maxillary arch. Surprisingly, few studies have been dedicated to this subject, and no data on its prevalence were found. The search in Medline for “extraction space reopening” showed only 6 articles up to October 2013. Even in the most successfully treated extraction patients, whose teeth were tightly approximated, teeth adjacent to the old extraction area can separate. The opened spaces at the extraction sites may vary from a fraction of a millimeter to several millimeters. On the other hand, residual extraction spaces can demonstrate spontaneous closure in the long term after treatment. Oftedal and Wisth evaluated extraction spaces that were not completely closed and observed that 35% of maxillary residual spaces and 46% of mandibular residual spaces totally closed in the postretention period.
Some etiologic factors that were previously related to extraction space reopening are gingival invagination on the extraction site and root parallelism. Gingival invaginations may occur because of the approximating movement of neighboring teeth and are more frequent in the mandibular arch than in the maxillary arch. The explanation is the occurrence of gingival fiber displacement instead of remodeling, resulting in tissue accumulation. Because of the assumption that this local factor could predispose a patient to relapse of the extraction site closure, some authors have suggested periodontal surgery to remove the excessive gingival tissues. However, there is no evidence associating gingival invagination and extraction space reopening so far.
Additionally, root parallelism between the canines and the second premolars in patients having first premolar extractions has been considered an important factor for the stability of space closure. Hatasaka observed that parallel roots are more stable during the posttreatment period and also more favorable for tooth interdigitation. More recently, Chiqueto et al found no differences for neighboring tooth angulation in patients with and without extraction space reopening.
The prevalence of extraction space reopening after orthodontic treatment as well as its predisposing factors must be better elucidated, because extractions are often required in orthodontic treatment. In this study, we aimed to verify the frequency of extraction space reopening in patients with Class I malocclusions treated with extractions of the 4 first premolars and to evaluate the long-term behavior of these spaces. Additionally, possible associated factors such as initial tooth crowding, angulation between canine and second premolar crowns, and the amount of mandibular incisor retraction were investigated.
Material and methods
This study was approved by the ethics committee at the University of São Paulo in Brazil. To detect a 20% difference in space reopening with α = 5% and β = 80%, the sample should comprise at least 37 subjects. The sample was obtained from the files of the Department of Orthodontics at the University of São Paulo. The inclusion criteria were Class I malocclusion treated with 4 first premolar extractions, complete permanent dentition at the pretreatment stage, standard edgewise appliances used, no dental anomalies of number (agenesis or supernumerary teeth), no history of periodontal surgery in the extraction area, and availability of dental casts obtained at the end of treatment and at 1 and 5 years after treatment.
After applying these criteria, 43 patients were selected. The sample initial age ranged from 11.3 to 16.2 years (mean, 13.6 years; standard deviation [SD], 1.4 years). The age at the end of comprehensive orthodontic treatment ranged from 13.1 to 20.7 years (mean, 16.1 years; SD, 2.0 years). All patients had the same retention protocol, including a modified Hawley retainer for the maxillary arch and a canine-to-canine fixed bonded retainer for the mandibular arch. The Hawley retainer was recommended to be used full time for 6 months, followed by nights-only use for 6 months. The mandibular fixed bonded retainer was used for a mean period of 3 years.
On the final, 1-year, and 5-year dental casts from these patients, the numbers of open and closed extraction sites were calculated at each stage and compared to evaluate the frequency of extraction space reopening in patients with Class I malocclusions. Only the quadrants that were fully closed at the end of treatment were considered: 124 quadrants. To evaluate whether initial tooth crowding, angulations between the canine and second premolar crowns in each quadrant, and amounts of mandibular incisor retraction were predisposing factors for extraction space reopening, the 43 patients were divided into 2 groups: group 1, with 13 patients with at least 1 extraction space reopening, and group 2, with 30 patients without space reopening in the posttreatment periods of 1 and 5 years.
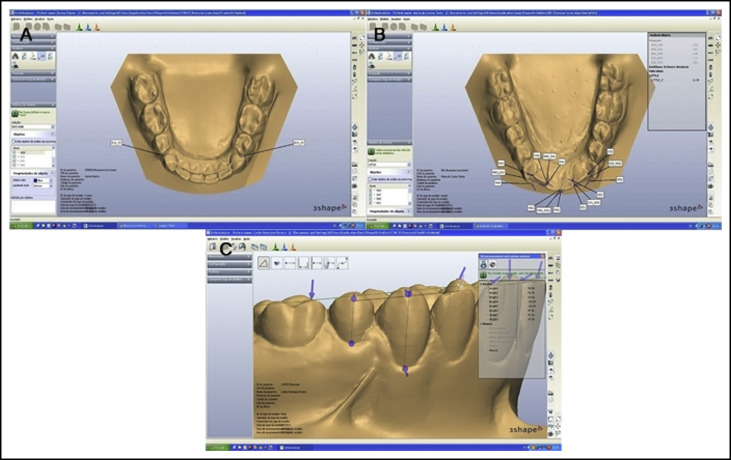
To measure the dental cast variables, the initial, final, 1-year, and 5-years posttreatment dental casts were digitized using a 3-dimensional scanner (R700; 3Shape, Copenhagen, Denmark). The following variables were measured with the OrthoAnalyzer 3-dimensional software (3Shape) ( Fig 1 ).
- 1.
Initial mandibular crowding measured with Little’s irregularity index. After identifying points on the proximal aspects of the anterior teeth, the software automatically calculated the irregularity index value.
- 2.
Angulation between the canines and the second premolars. The angulation of the crown long axis was measured relative to the occlusal plane. The occlusal plane was obtained by marking 3 points: bilaterally on the mesiobuccal cusp tips of the first molars and one point on the incisors. The long axis of the clinical crown was constructed according to the method of Andrews. The digital model was rotated to position the occlusal plane parallel to the horizontal plane. The angulation measurements were performed on the perspective of a buccal segment plane by rotating the model on the vertical axis from the lateral view so that the operator could see the entire mesiodistal width of the contralateral central incisor ( Fig 1 , C ). The angulation between the canine and the second premolar was calculated. Negative values meant convergence between the crowns’ long axes, and positive values meant divergence between the crowns’ axes.
To measure the amount of mandibular incisor retraction, the initial and final cephalometric radiographs were digitized with a scanner (i800; Microtek ScanMaker, Santa Fe Springs, Calif) and analyzed with imaging software (version 11.5; Dolphin Imaging & Managent Solutions, Chatsworth, Calif). The magnification factors were corrected by the software. To measure the amount of mandibular incisor retraction during orthodontic treatment, the distance from the labial aspect of the mandibular central incisor crown to the line from nasion through point B of the mandible was measured. The difference between the initial and final measurements was calculated.
Thirty patients were randomly selected, and all variables were remeasured after 30 days. Random and systematic errors were calculated with Dahlberg’s formula and dependent t tests, respectively, at a significance level of 5%.
Statistical analysis
The percentage of patients with at least 1 site that was fully closed at the end of treatment and reopened in the posttreatment stage was calculated in the whole sample. Also, the percentages of space reopening in the maxillary and mandibular arches were calculated.
To compare the numbers of open and closed extraction spaces between the posttreatment and the 1-year and 5-years posttreatment dental casts, Cochran tests were used. To evaluate space reopening after treatment, only fully closed spaces at the end of treatment were considered for this analysis.
All quantitative variables were tested for normality using Shapiro-Wilk tests, which showed that they had a normal distribution. Therefore, t tests were used to compare groups 1 and 2 regarding the initial and final ages, initial mandibular crowding, angulations between the canine and second premolar crowns in each quadrant, and the amounts of mandibular incisor retraction. The significance level considered was 5%. All statistical analyses were performed with software (Statistica for Windows version 11.0; StatSoft, Tulsa, Okla).
Results
The random errors were within acceptable limits, varying from 0.03 to 1.51, and there were no statistically significant systematic errors ( Table I ).
| Variable | Measurement 1 (n = 30) | Measurement 2 (n = 30) | Dahlberg | P | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Mandibular crowding | 9.96 | 4.08 | 10.16 | 4.03 | 0.55 | 0.16 |
| Right maxilla | 0.19 | 0.41 | 0.20 | 0.43 | 0.04 | 0.49 |
| Left maxilla | 0.15 | 0.31 | 0.16 | 0.33 | 0.04 | 0.62 |
| Right mandible | 0.17 | 0.31 | 0.17 | 0.31 | 0.03 | 0.38 |
| Left mandible | 0.19 | 0.33 | 0.23 | 0.37 | 0.12 | 0.20 |
| Right maxillary angle | −1.42 | 5.86 | −1.43 | 5.52 | 1.36 | 0.98 |
| Left maxillary angle | −2.77 | 4.56 | −2.05 | 5.11 | 1.51 | 0.06 |
| Right mandibular angle | −0.68 | 4.08 | −0.63 | 4.12 | 1.12 | 0.88 |
| Left mandibular angle | −2.82 | 4.46 | −2.31 | 4.45 | 1.03 | 0.06 |
| Amount of mandibular incisor retraction | 1.75 | 1.62 | 1.76 | 1.58 | 0.13 | 0.77 |
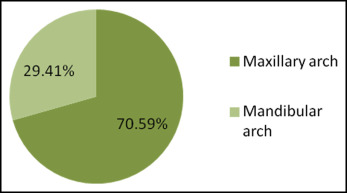
The results showed that 30.23% of the patients had at least 1 site that was fully closed at the end of treatment and reopened in the 1-year posttreatment period ( Fig 2 ). Nine patients had only 1 quadrant with reopening. Considering the number of quadrants, 13.7% of the closed sites reopened in the posttreatment period (17 of 124 quadrants). From these, 9.67% (12 of 124) were in the maxillary arch, and 4.03% (5 of 124) were in the mandibular arch. Therefore, extraction space reopening was more frequent in the maxillary arch ( Fig 3 ).
The frequency of open spaces significantly increased between the final and the 1-year posttreatment dental casts (except for the mandibular right site). However, the frequency of open spaces significantly decreased between the casts at 1 year and 5 years for the mandibular left site and for all sites ( Table II ).
| Site | Final | 1 year | 5 years | P | |||
|---|---|---|---|---|---|---|---|
| Open | Closed | Open | Closed | Open | Closed | ||
| Right maxilla | 0 | 34 | 5 | 29 | 2 | 32 | 0.02 ∗ |
| Left maxilla | 0 | 30 | 7 | 23 | 4 | 26 | 0.00 ∗ |
| Right mandible | 0 | 3 | 1 | 30 | 1 | 30 | 0.36 |
| Left mandible | 0 | 29 | 4 | 25 | 0 | 29 | 0.01 ∗ |
| Total | 0 | 124 | 17 | 107 | 7 | 117 | 0.00 ∗ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


