Introduction
The objectives of this research were to assess skeletal and dental changes in patients with Class II malocclusion treated with the edgewise crowned Herbst appliance in the early mixed dentition and to measure the stability of treatment after a second phase of fixed appliance therapy.
Methods
Twenty-two patients (ages, 8.4 ± 1.0 years) with Class II Division 1 malocclusion treated consecutively with the edgewise crowned Herbst appliance in the early mixed dentition were studied. Lateral cephalograms were taken before Herbst treatment, immediately after Herbst treatment, and after a second phase of fixed appliance therapy. The results were compared with a control group of untreated Class II subjects selected from the Bolton-Brush study, matched by age, sex, and craniofacial morphology. A total of 37 sagittal, vertical, and angular cephalometric variables were evaluated. Changes in overjet and molar relationship were calculated. Changes due to growth were subtracted to obtain the net changes due to treatment. The data were analyzed by using analysis of variance (ANOVA) and the t tests.
Results
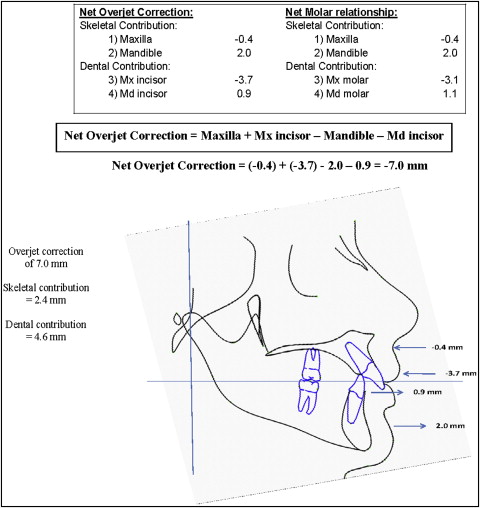
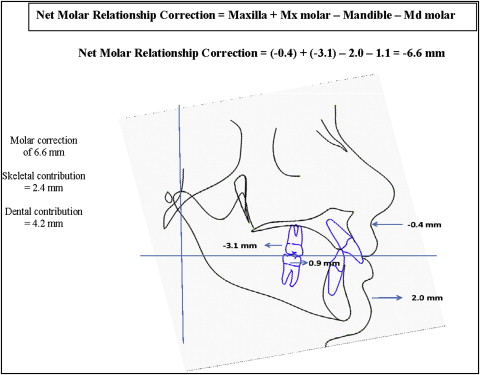
Overcorrection with the Herbst appliance resulted in an average reduction in overjet of 7.0 mm and a change in molar relationship of 6.6 mm. Several factors contributed to the change in overjet: restraint of the forward movement of the maxilla (0.4 mm), forward movement of the mandible (2.0 mm), backward movement of the maxillary incisors (3.7 mm), and forward movement of the mandibular incisors (0.9 mm). Skeletal changes together with a 3.1-mm backward movement of the maxillary molars and a 1.1-mm forward movement of the mandibular molars contributed to the changes in molar relationship. After the second phase of fixed appliance therapy, the change in overjet was reduced to 2.8 mm. Most of the remaining overjet corrections were contributed by the restraint of maxillary growth (2.8 mm). The mandible moved posteriorly by 1.6 mm, and the mandibular incisors moved forward by 0.2 mm. Change in molar relationship was reduced to 2.2 mm. The maxillary molars moved backward by 0.2 mm, and the mandibular molars moved forward by 0.8 mm.
Conclusions
Overcorrection of Class II malocclusion with the edgewise crowned Herbst appliance in the early mixed dentition resulted in a significant reduction in overjet and correction of the molar relationship. A portion of the correction was maintained after a second phase of fixed appliance therapy because of the continuous restraint of maxillary growth and the dentoalveolar adaptations.
Class II skeletal malocclusions are commonly treated in 1 phase of fixed appliance therapy or with a functional appliance followed by a fixed appliance. The Herbst appliance can be used with a fixed appliance, and the treatment time is shorter. Patient cooperation is minimal, with a high success rate of treatment. Recent studies suggested that fixed functional appliances can be effective in correcting Class II skeletal abnormalities by promoting growth of the mandible and remodeling of the glenoid fossa. The timing of orthopedic intervention with functional appliances is also a subject of intense controversy. When determining the optimal time to initiate Class II treatment, factors such as the ability to use all potential growth, the likelihood of incisor trauma, the development of improper swallowing patterns, incomplete lip function, effects on the temporomandibular joint, and psychosocial concerns need to be considered. Successful treatments of Class II malocclusions in the early mixed dentition have been reported. However, data from randomized controlled clinical trials have shown that effective skeletal changes were better achieved in the late mixed dentition and early permanent dentition with more stable results. Other studies suggest that supplementary mandibular growth with functional appliance therapy appears to be greater if the functional treatment is performed during the pubertal growth period. The purpose of this study was to investigate the skeletal and dental changes of Class II patients treated in the early mixed dentition with the crowned Herbst appliance and the stability of these changes after a second phase of fixed appliance therapy. The null hypotheses were that there will be no significant differences in skeletal or dental changes with Herbst treatment in the early mixed dentition and after a second phase of fixed appliance therapy compared with the control group.
Material and methods
The experimental group included 56 Class II patients treated consecutively by an author (T.D.) with the edgewise crowned Herbst appliance in the early mixed dentition followed by fixed appliance therapy. The criteria for selection included (1) no previous orthodontic treatment, (2) Class II malocclusion in the mixed dentition with an ANB greater than 4°, and (3) completion of both phases of treatment (patients who did not require a second phase of treatment or did not complete the second phase of treatment were excluded), and (4) no craniofacial anomalies. The final sample that met the inclusion and exclusion criteria included 22 subjects.
Serial cephalometric radiographs of 22 untreated subjects with Class II malocclusion were obtained from the Case Western University’s Bolton-Brush study, Cleveland, Ohio, as the control group. They were matched in sex, age, and craniofacial morphology with the experimental subjects.
The Herbst appliance uses a bilateral telescope mechanism consisting of a tube, a plunger, 2 pivots, and 2 locking screws that function to keep the mandible in a continuously anterior jumped position ( Fig 1 ). The pivot for the tube was located on the maxillary second deciduous molar or the permanent first molar, and the pivot for the plunger was attached to the mandibular second deciduous molar or the permanent first molar. The length of the tube determined the amount of anterior displacement of the mandible. The appliance was designed to incorporate edgewise brackets and mechanics into the correction of Class II malocclusions.
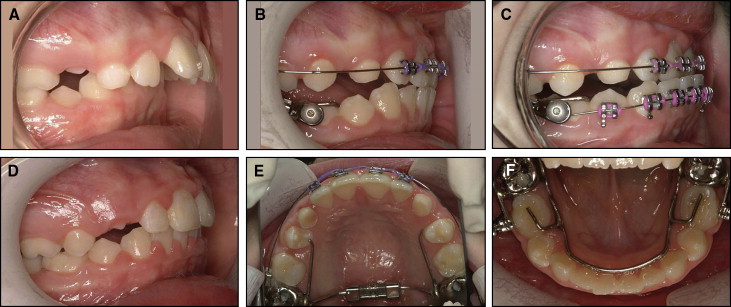
The mandibular incisor brackets incorporated a −10° inclination to minimize the proclination of the incisors during the Herbst treatment. Stainless steel crowns on the maxillary and mandibular second deciduous molars or the permanent first molar, anchored the Herbst appliance to the dentition. Double buccal tubes were placed on the molar crowns to permit an auxiliary archwire to intrude the maxillary or mandibular incisors as necessary. The maxillary arch was tied back to hooks on the molar tubes to prevent space from opening in the maxillary arch and the maxillary molars from distalizing. In addition, consolidation of the maxillary arch distributed the load applied to all teeth in an attempt to elicit the maximum orthopedic effect. In the mandibular arch, a 2-mm half-round cantilever was placed between the second deciduous molar and the interproximal area between the first deciduous molar and the canine. The axle was placed at the mesial end of the cantilever, and a 0.022 × 0.028-in archwire tube was placed above and below the axle.
A transpalatal arch was not included in the appliance to allow the first molars to rotate as the Class II relationship was corrected. A lingual arch was not included to allow easier placement of the appliance and prevent possible tipping of the mandibular anterior incisors. Both arches were free to accommodate expansion during treatment, if necessary. An occlusal stop off the cantilever arm or directly soldered to the stainless steel crowns extended into and rested on the distal central fossa of the first deciduous molar to prevent tipping of the cantilever arm and impingement into the buccal mucosa and to minimize tipping and rotation of the mandibular second deciduous molar.
The Herbst appliance was activated initially to an edge-to-edge incisor relationship with the skeletal midlines in alignment. Brackets were bonded to the maxillary and mandibular incisors and deciduous canines as needed. Heat-treated copper-nickel-titanium archwires were used to control incisor inclination and mandibular molar movement. The archwire sequence began with a 0.014-in copper-nickel-titanium wire. Then a 0.016 × 0.025-in copper-nickel-titanium wire was used with the maxillary wire tied back to the hook on the maxillary molar, and the mandibular wire was annealed and cinched to prevent anterior movement. Next, a mandibular 0.019 × 0.025-in reverse curve nickel-titanium archwire was placed when more leveling was necessary, and a maxillary 0.019 × 0.025-in beta-titanium alloy wire was placed if more leveling or torque was desired.
To achieve the maximum orthopedic effect, the maxillary archwire was tied back to prevent distalization of the maxillary molars. The appliance was activated in a step-by-step fashion at a distance of 4 mm every 12 weeks until the maxillary canine achieved an end-to-end or full-tooth overcorrected relationship with the mandibular first premolar or first deciduous molar. The overcorrected position was held for 12 weeks. Corrected sagittal tomograms were taken before placement of the Herbst appliance and before its removal to confirm the condylar position. If the condyles were reasonably centered in the glenoid fossa, then a lateral cephalogram was taken, and the patient was scheduled for Herbst removal as soon as possible.
In the mixed dentition treatment after Herbst removal, the first permanent molars were banded, and 2 × 4 appliance treatment continued until the anterior occlusion was corrected, overbite was corrected, and there was proper torque on the incisors. Also, the maxillary and mandibular first permanent molar width was coordinated. If more arch length was necessary, molar bands with 0.022 × 0.028-in extension tubes soldered in the archwire slots were placed, and open-coil springs were used to create more arch length. Appliance removal occurred in 2 appointments. At the first appointment, maxillary and mandibular alginate impressions were taken, and sectional archwires were placed. At the second appointment, the incisor brackets were removed, and maxillary and mandibular lingual holding arches were placed. The lingual arches helped to prevent overbite relapse, saved leeway space, and maintained the arch form. The patients were instructed that the holding arches would remain in place until all permanent teeth had erupted. At that time, the patients were reevaluated for comprehensive orthodontic treatment to finalize the occlusion.
Institutional review board approval was obtained from West Virginia University before the study. Approval was also obtained from the author’s office (T.D.) and the Bolton-Brush Center for the use of the orthodontic records and radiographs, respectively.
Lateral cephalograms were scanned into digital format with a scanner (Expression 1680, Epson America, Long Beach, Calif) and printed on a printer (C510, Lexmark International, Lexington, Ky). Each printout was superimposed on the original radiograph to ensure a 1:1 conversion with no distortion. Digital radiographs obtained from the Bolton-Brush study were scanned at 12-bit gray-scale resolution with a spatial resolution of 0.1 mm per pixel and stored in uncompressed TIFF format. The images were converted to JPEG format with software (Irfan View, version 4.0; http://www.irfanview.com /) and loaded into Photoshop (version 6.0, Adobe Systems, San Jose, Calif) for size analysis. All original radiographs from the Bolton-Brush study were indexed with 4 corner fiduciary points by using a template according to the method described by Baumrind and Miller. In Photoshop, the resolutions of the images were verified (600 dpi), and the images were resized to the original dimensions of the unscanned radiographs. Printouts were then made, and the fiduciary points were measured with an electronic digital calipers to ensure a 1:1 conversion with no distortion from the original radiographs.
Tracings were made by an operator (T.G.W.) using a #2 HB mechanical lead pencil (Pentel 0.5 mm lead; Torrance, Calif), an orthodontic protractor, and 0.003-in matte cephalometric acetate tracing film (3M Unitek, Monrovia, Calif). A custom cephalometric analysis was performed by using landmarks described by published cephalometric systems. The data were normalized to account for magnification differences between the cephalometric machine used for the Bolton-Brush study (5.6%) and the cephalometric machine at the author’s office (10%).
Each angular variable was measured with a cephalometric protractor and evaluated to the nearest 0.5°. Each sagittal and vertical measurement was made with electronic digital calipers and evaluated to the nearest 0.1 mm.
The reliability of the cephalometric measurements was tested by investigating the errors in locating, superimposing, and measuring the changes of all landmarks. Pretreatment and posttreatment lateral cephalograms of 10 randomly selected patients were retraced at least 2 weeks after the initial tracing and analyzed to evaluate errors. For all cephalometric variables, differences between the measurements recorded at the first and second tracings were compared for each subject before treatment (T1), immediately after treatment (T2), and after the second phase of fixed appliance therapy (T3). A matched-pairs t test was performed to compare the 2 registrations. A correlation coefficient was established for each variable at each time point to determine the reliability. Overall, the method of cephalometric analysis used in this study, including landmark identification, superimposition of radiographs, and measurements, was determined to be reliable, with most correlation coefficients above 0.9.
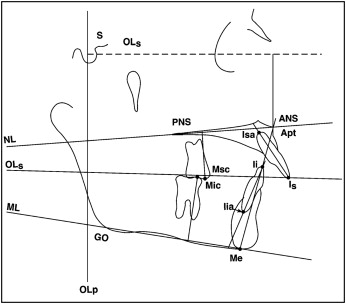
Analyses of the sagittal skeletal and dental changes were performed by constructing a reference grid based on the occlusal line (OL) and the occlusal line perpendicular (OLp), obtained from the T1 lateral cephalogram ( Fig 2 ). This reference grid was used for all sagittal measurements between OLp and the cephalometric landmarks. The reference grid from T1 was transferred to the T2 and T3 radiographs by superimposition on the anterior cranial base.
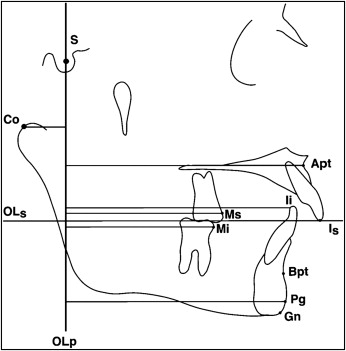
The reference lines that were used for the vertical measurements included OLs, NL, and ML, and OL. OLs was obtained from the T1 radiograph and transferred by superimposition on the anterior cranial base to the T2 and T3 radiographs. A measurement from ANS to Me (ANS-Me) was also included ( Fig 3 ).
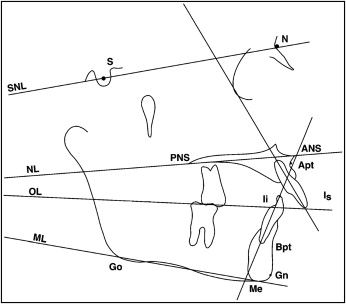
Angular measurements were used to identify changes in the dentofacial complex. Cephalometric landmarks and reference lines for the angular measurements are illustrated in Figure 4 .
To determine the amounts of skeletal and dental contributions to the overjet and molar relationship corrections, the dental changes in the maxilla and the mandible were calculated according to the method described by Pancherz.
Statistical analysis
A matched-pairs t test was used to compare the starting forms between the treatment and control subjects at T1. The differences between the treatment and control subjects for each variable across the 3 time periods (T1-T3) were analyzed for each sex and the pooled subjects. A repeated-measures analysis of variance (ANOVA) was performed to determine whether the differences between the treatment and control subjects were the same across the 3 time periods. A matched-pairs t test was performed for each variable to identify the treatment effects of the Herbst appliance (changes in the treatment group T2-T1) minus (changes in the control group t2-t1), and combined phase 1 and phase 2 treatment (T3-T1) minus (t3-t1). A significance level of P <0.05 was used.
Results
The final sample size consisted of 22 subjects (7 boys, 15 girls). The mean ages of the treatment and control groups at T1 of the pooled subjects were 8.4 ± 1.0 and 8.4 ± 1.1 years, respectively. The mean ages of the treatment and control groups at T2 were 9.3 ± 0.9 and 9.4 ± 0.8 years, respectively. The mean ages of the treatment and control groups at T3 were 14.6 ± 1.4 and 14.7 ± 1.5 years, respectively. No significant differences were found between the treatment and control groups at any time period.
Sex differences were analyzed for pretreatment craniofacial morphology and treatment changes. Because of the large quantity of data generated, only pooled data were reported.
Table I shows the pretreatment craniofacial morphology of the 2 groups. For the pooled subjects, significant differences were found in 4 of the 37 variables at T1. The variables OLp–A-point, Is-OLp, and ANB were greater in the treatment group than in the control group, and OLs–A-point was less in the treatment group than in the control group.
| Variable | Control | Treated | P value | Difference | Significance | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Sagittal (mm) | |||||||
| Olp–A-point | 68.3 | 4.2 | 70.6 | 3.3 | 0.0479 | 2.3 | ∗ |
| Olp-Pg | 71.0 | 5.5 | 71.9 | 4.5 | 0.5437 | 0.9 | NS |
| Olp-Co | 9.6 | 2.1 | 8.2 | 2.9 | 0.0738 | 1.4 | NS |
| Co–A-point | 78.3 | 4.3 | 79.7 | 4.9 | 0.3255 | 1.4 | NS |
| Co-Gn | 95.5 | 5.0 | 95.1 | 4.9 | 0.8154 | 0.4 | NS |
| Co-Gn minus Co–A-point | 17.1 | 2.9 | 15.8 | 3.8 | 0.2072 | 1.3 | NS |
| Wits | 1.1 | 1.6 | 1.1 | 1.9 | 0.983 | 0.0 | NS |
| Is-Olp | 73.5 | 5.6 | 76.6 | 4.3 | 0.0403 | 3.1 | ∗ |
| Ii-Olp | 68.8 | 4.4 | 71.0 | 3.5 | 0.0782 | 2.2 | NS |
| Overjet | 4.7 | 2.1 | 5.6 | 2.6 | 0.1694 | 0.9 | NS |
| Ms-Olp | 46.0 | 3.7 | 47.9 | 2.7 | 0.0524 | 1.9 | NS |
| Mi-Olp | 45.7 | 4.3 | 47.1 | 2.9 | 0.1894 | 1.4 | NS |
| Molar relationship | 0.3 | 0.9 | 0.8 | 2.0 | 0.3244 | 0.5 | NS |
| Vertical (mm) | |||||||
| OLs–A-point | 25.2 | 2.2 | 22.8 | 4.1 | 0.0215 | 2.4 | ∗ |
| ANS-Me | 57.0 | 4.6 | 56.9 | 3.2 | 0.9324 | 0.1 | NS |
| Is-NL | 23.7 | 4.1 | 23.6 | 2.8 | 0.9635 | 0.1 | NS |
| Ii-ML | 34.1 | 3.2 | 33.2 | 2.4 | 0.3418 | 0.9 | NS |
| Overbite | 1.6 | 3.0 | 1.4 | 3.4 | 0.8021 | 0.2 | NS |
| Msc-NL | 16.7 | 3.0 | 17.0 | 1.9 | 0.7502 | 0.3 | NS |
| Mic-ML | 25.7 | 1.9 | 25.6 | 2.1 | 0.8807 | 0.1 | NS |
| Angular (°) | |||||||
| SNA | 79.9 | 3.2 | 81.4 | 3.9 | 0.1633 | 1.5 | NS |
| SNB | 75.3 | 3.0 | 75.0 | 3.6 | 0.8058 | 0.3 | NS |
| ANB | 4.6 | 1.3 | 6.4 | 2.1 | 0.0018 | 1.8 | ∗ |
| SNL-NL | 7.5 | 3.2 | 8.3 | 3.6 | 0.459 | 0.8 | NS |
| SNL-ML | 34.1 | 4.6 | 34.4 | 7.9 | 0.8803 | 0.3 | NS |
| SNL-OL | 20.3 | 3.5 | 22.3 | 4.2 | 0.1057 | 2.0 | NS |
| Is/NL | 111.0 | 5.9 | 109.6 | 6.0 | 0.4226 | 1.4 | NS |
| Ii/ML | 94.6 | 5.7 | 96.0 | 9.3 | 0.5413 | 1.4 | NS |
| Interincisal angle | 127.6 | 7.9 | 126.7 | 10.3 | 0.7386 | 0.9 | NS |
Table II compares the skeletal and dental changes (T2-T1) between the treatment and control groups for the pooled subjects.
| Variable | Control (t2-t1) | Treated (T2-T1) | Difference | P value | Significance | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Age (y) | 13.5 | 6.9 | 12.2 | 6.8 | −1.3 | 0.6304 | NS |
| Sagittal (mm) | |||||||
| Olp–A-point | 1.4 | 0.6 | 1.0 | 1.9 | −0.4 | 0.4206 | NS |
| Olp-Pg | 0.8 | 2.8 | 2.8 | 3.5 | 2.0 | 0.1221 | NS |
| Olp-Co | 0.7 | 1.6 | −0.8 | 1.9 | −1.5 | 0.0396 | ∗ |
| Co–A-point | 2.1 | 1.7 | −0.5 | 3.4 | −2.6 | 0.0205 | ∗ |
| Co-Gn | 2.7 | 2.5 | 3.4 | 2.3 | 0.7 | 0.4778 | NS |
| Co-Gn minus Co–A-point | 0.6 | 2.1 | 3.2 | 2.9 | 2.6 | 0.0159 | ∗ |
| Wits | −0.7 | 1.6 | −4.4 | 3.0 | −3.7 | 0.0009 | ∗ |
| Is-Olp | 2.5 | 1.9 | −1.6 | 4.5 | −4.0 | 0.0065 | ∗ |
| Ii-Olp | 1.9 | 1.5 | 4.8 | 3.0 | 3.0 | 0.0041 | ∗ |
| Overjet | 0.6 | 1.6 | −6.4 | 3.9 | −6.9 | 0.0001 | ∗ |
| Ms-Olp | 1.6 | 1.3 | −1.9 | 2.2 | −3.4 | 0.0001 | ∗ |
| Mi-Olp | 1.7 | 1.4 | 4.8 | 1.9 | 3.1 | 0.0001 | ∗ |
| Molar relationship | −0.2 | 0.9 | −6.6 | 2.8 | −6.4 | 0.0001 | ∗ |
| Vertical (mm) | |||||||
| OLs–A-point | 1.4 | 1.2 | 2.0 | 1.6 | 0.6 | 0.3174 | NS |
| ANS-Me | 1.7 | 1.4 | 1.3 | 1.7 | −0.4 | 0.5006 | NS |
| Is-NL | 1.8 | 3.1 | 0.9 | 3.0 | −0.9 | 0.4766 | NS |
| Ii-ML | 1.0 | 0.8 | −0.8 | 2.5 | −1.8 | 0.0175 | ∗ |
| Overbite | 1.3 | 2.9 | −1.1 | 3.6 | −2.4 | 0.0821 | NS |
| Msc-NL | 1.3 | 2.0 | −1.3 | 1.2 | −2.7 | 0.0005 | ∗ |
| Mic-ML | 0.6 | 1.0 | 1.2 | 1.3 | 0.7 | 0.1517 | NS |
| Angular (°) | |||||||
| SNA | 0.6 | 1.4 | −0.3 | 2.4 | −1.0 | 0.2269 | NS |
| SNB | 0.6 | 1.6 | 1.6 | 2.1 | 1.0 | 0.1745 | NS |
| ANB | 0.0 | 1.2 | −2.0 | 2.4 | −2.0 | 0.0141 | ∗ |
| SNL-NL | −0.7 | 2.0 | 1.0 | 1.8 | 1.7 | 0.0283 | ∗ |
| SNL-ML | −0.1 | 1.8 | 0.1 | 1.6 | 0.2 | 0.7347 | NS |
| SNL-OL | 0.6 | 2.1 | 3.4 | 3.8 | 2.8 | 0.0306 | ∗ |
| Is/NL | −0.3 | 3.4 | −7.3 | 7.3 | −7.0 | 0.0043 | ∗ |
| Ii/ML | −0.5 | 2.8 | 7.1 | 6.9 | 7.6 | 0.0012 | ∗ |
| Interincisal angle | −0.8 | 6.0 | 1.4 | 9.4 | 2.2 | 0.4922 | NS |
All sagittal variables showed a significant difference between the treatment and control group except for OLp–A-point, OLp-Pg, and Co-Gn. The position of the maxillary base (OLp–A-point) moved backward 0.4 mm compared with the control group. The position of the mandibular base (OLp-Pg) moved forward 2.0 mm compared with the control group. The position of the condyle (OLp-Co) moved anteriorly 1.5 mm relative to the control group. The effective maxillary length (Co–A-point) and mandibular length (Co-Gn) showed differences of −2.6 and 0.7 mm from the control group, respectively. The position of the maxilla relative to the mandible along the functional occlusal plane (Wits appraisal) showed a difference of −3.7 mm compared with the control group. The position of the maxillary incisor (Is-OLp) moved backwards 4.1 mm compared with the control group. The mandibular incisors (Ii-OLp) moved forward 2.9 mm compared with the control group. The maxillary molars (Ms-OLp) moved posteriorly 3.5 mm compared with the control group.
All vertical variables showed no significant differences between the treatment and control groups from T2 to T1, except for Ii-ML and Msc-NL. The mandibular incisor (Ii-ML) was intruded 1.8 mm compared with the control group. The maxillary molar was intruded 2.6 mm compared with the control group.
Significant differences in the angular variables between the control and treatment groups were found in the variables ANB, SNL-NL, SNL-OL, Is/NL, and Ii/ML. A net decrease in ANB of 2.0° was found in the treatment group relative to the control group. Net increases of 1.7° and 2.8° were found in the palatal plane angle (SNL-NL) and the functional occlusal plane angle (SNL-OL), respectively. The inclination of the maxillary incisor (Is/NL) decreased by 7.0° compared with the control group, but the mandibular incisor angle (Ii/ML) had a net increase of 7.6° compared with the control group.
Figures 5 and 6 show the calculation of net overjet and molar relationship corrections. The amount of skeletal and dental contributions to the changes in overjet and molar relationship are shown in Figure 7 . The net overjet reduction in the treatment group was 7.0 mm, with 2.4 mm (34%) of the correction contributed by skeletal change and 4.6 mm (67%) by dental change. The net molar correction was 6.6 mm, with 2.4 mm (36%) of the correction contributed by skeletal change and 4.2 mm (64%) by dental change.