The intent of this article is to familiarize dental professionals with the polysomnogram (PSG). The evaluation of patients presenting with sleep disorders is complex, requiring an investigative approach that synthesizes information obtained through a detailed history, a focused physical examination, and appropriate confirmatory testing. The PSG is the only clinical tool that measures multiple physiologic variables to qualitatively and quantitatively evaluate sleep. A proper understanding of the role of the PSG and its measurements and interpretation allows for a proper diagnosis so as to provide an optimal range of treatments for individual patients.
The intent of this article is to familiarize dental professionals with the polysomnogram (PSG). Through a better understanding of the PSG as a diagnostic tool, dental professionals are able to provide a more comprehensive assessment of individual patients who present with a sleep disorder complaint, including sleep-related breathing disorders (SRBDs).
The initial assessment of patients with a sleep disorder may be extensive. Most sleep disorders are classified into disorders of insomnia, SRBDs, nocturnal movement or behavioral disorders, and disorders of hypersomnolence.
The clinical approach to patients presenting with a chief complaint of a sleep disorder begins with a comprehensive sleep history. Information, including the onset of symptoms, duration of symptoms, exacerbating and relieving factors, and whether complaints are from patients themselves or from a bed partner, is elicited. If a concern is a nocturnal behavior, such as snoring, irregular breathing patterns, excessive movement, or unusual behaviors, the descriptive detail provided by the patient, bed partner, or even audiovisual recordings is helpful. Additional details include a patient’s daily schedule, usual bedtime, time to fall asleep, nocturnal awakenings, time to return to sleep, awakening time, estimated sleep time, and sense of sleep quality. Environmental factors, including light, noise, temperature, comfort of the bed, use of electronic devices, and pets, are all potential exacerbating factors. Morning symptoms, such as dry mouth, headache, jaw discomfort, and level of alertness, may assist with better defining a sleep problem. The daytime schedule, including naps, meal times, caffeine and alcohol use, and level of alertness, are also valuable. Review of past medical illnesses, medications, and social and family history and a review of systems should be routinely performed. For disorders suggestive of SRBDs, a detailed examination that, at a minimum, includes the upper airway, pulmonary, cardiovascular, and neurologic systems is recommended.
Once an initial evaluation is complete, a differential diagnosis is created. The International Classification of Sleep Disorders, Second Edition , provides a comprehensive list of sleep diagnoses and presenting symptoms and is recommended for reference. Many sleep disorders may be easily identified and treated without additional testing. Use of sleep diaries, sleep questionnaires, overnight oximetry, laboratory testing, and imaging studies may be helpful in the appropriate clinical setting. Other disorders, such as SRBDs, require a more direct assessment of a patient’s sleep. This is best performed through the PSG.
The PSG is the most commonly used test in the diagnosis of SRBDs. The PSG is considered the gold standard for the diagnosis of SRBDs and is useful in the evaluation and diagnosis of other sleep disorders. The PSG is indicated in the following diagnostic evaluations :
- •
Diagnosis of SRBDs
- •
Positive airway pressure (PAP) and oral appliance therapy (OAT) titration in SRBDs
- •
Assessment of non-PAP treatment response of SRBDs
- •
Narcolepsy (PSG with multiple sleep latency test)
- •
Parasomnias that are complex or violent
- •
Seizure disorders (in circumstances where the clinical assessment or diagnostic electroencephalogram [EEG] is inconclusive)
- •
Periodic limb movement disorder.
PSG is not routinely recommended for disorders of insomnia, restless legs syndrome, circadian rhythm disorders, or depression.
PSG referral
Ordering a PSG requires referral to a designated sleep center. Referral may be directed first to a sleep specialist to provide further evaluation, diagnostic testing, education, and implementation of treatment. If PSG is indicated, the sleep specialist then may interpret the PSG with full knowledge of the patient who is evaluated and review the results with the patient before making treatment decisions. The sleep specialist may then provide longitudinal follow-up of the patient’s condition, including response and adherence to therapy.
Referral may also be made directly to the sleep center for PSG testing by a primary health care provider or dental professional. The PSG is reviewed in context of the history and physical findings reported by the referring provider. An interpretation of the PSG with treatment suggestions is made available. If a treatment regimen or follow-up is beyond the scope of practice for the referring provider, sleep specialist consultation or other specialty consultation is recommended.
Selecting a Sleep Laboratory
Laboratories that perform sleep studies are commonly referred to as sleep centers to indicate facilities that are capable of evaluating and treating a full range of sleep disorders. Sleep centers may be accredited or unaccredited. The American Academy of Sleep Medicine (AASM) is the largest accrediting organization for sleep centers at present. According to the AASM, there are currently more than 2200 sleep centers in the United States that are AASM accredited.
AASM accreditation requires adherence to specific standards in the areas of
- •
Personnel
- •
Policies and procedures
- •
Facility and equipment
- •
Patient evaluation and care
- •
Emergency procedures
- •
Data acquisition, scoring, and reporting
- •
Quality assurance.
An AASM-accredited sleep center must have a certified sleep specialist as medical director and must employ at least one registered sleep technologist. Accredited centers may be affiliated with a hospital or be independent, freestanding facilities. The AASM also offers accreditation for facilities that perform out-of-center sleep testing (ie, in-home testing) and for centers that offer durable medical equipment services (eg, continuous PAP [CPAP] equipment).
Role of the Sleep Technologist
The PSG is a time-intensive and technically demanding diagnostic test. These recordings are performed by PSG technologists, commonly referred to as sleep technologists. Working under the supervision of a licensed physician, a sleep technologist assists in the clinical assessment of patients by means of screening questionnaires, physiologic monitoring, and testing (PSG); treatment of sleep disorders using various therapeutic tools, including PAP devices; and providing education and instruction to patients in their care.
Since 1979, the Board of Registered Polysomnographic Technologists has been the primary credentialing program for sleep technologists employed in the United States and many other countries around the world. The registered polysomnographic technologist (RPSGT) credential is held by more than 16,000 individuals and is widely recognized in the field of sleep technology. The RPSGT designation is obtained through completion of a formal training program, hands-on training experience in a sleep center, and successful completion of the certification examination.
In 2007 the National Board for Respiratory Care developed a sleep disorders specialty credential (registered respiratory therapist-sleep disorder specialist [RRT-SDS]), and in November of 2011, the AASM began offering an registered sleep technologists (RST) credentialing examination.
Role of the Sleep Specialist
Sleep specialists receive specialized education in the diagnosis and management of sleep disorders. Accreditation previously was obtained through the American Board of Sleep Medicine. In 2007, member boards of the American Board of Medical Specialties began administration of a subspecialty certification examination for sleep medicine. Member boards include the American Board of Anesthesiology, American Board of Family Medicine, American Board of Internal Medicine, American Board of Pediatrics, American Board of Psychiatry and Neurology, and the American Board of Otolaryngology. Currently, subspecialty certification may only be obtained through successful completion of a 12-month formal sleep medicine training program and acceptable performance on the sleep medicine certification examination. This is a time-limited certification and requires continuing medical education and periodic renewal every 10 years with a recertification examination.
Additional training provides sleep specialists with the knowledge base necessary for comprehensive PSG analysis and interpretation. The field of sleep disorders crosses many different specialties and thus makes necessary a diverse spectrum of treatment options.
The polysomnogram
A PSG is the continuous recording of multiple physiologic variables over a sleep period that provides quantitative and qualitative measures of sleep. In the early days of sleep technology, the PSG recording was made on paper using a multichannel polygraph machine. PSGs are now routinely recorded using digital amplifiers and stored electronically ( Fig. 1 ).

In-Center Polysomnogram
In-center PSGs are typically recorded during an overnight stay at the sleep center and monitored by a sleep technologist stationed in a nearby control room. When a patient sleeps during the day due to shift work, a PSG may be performed during the patient’s usual bedtime hours.
Prestudy procedures include review of the order and indications for PSG; review of recent history and examination as provided by the referring health care provider; review of recent sleep diary, sleep questionnaires, medications, caffeine or alcohol consumption; and any change in a patient’s overall health and schedule of activities in the days leading up to the PSG. Once the patient is ready, the hookup for PSG is initiated, during which various sensors are applied.
Electroencephalogram, Electro-oculogram, and Electromyography
EEG is the recording of surface electrical activity of the brain. Proper locations for EEG leads are determined by measuring a patient’s head using the International 10–20 System of Electrode Placement. A standard PSG may use 4 to 6 scalp electrodes, plus references, for recording brain activity. EEG recording assists with determining sleep staging and wakefulness. More detailed EEG recording is obtained when there is clinical concern for seizure disorder.
Electro-oculography (EOG) is a recording of eye movements during sleep and wakefulness. Eye movements are recorded as deflections in the EOG leads. EOG allows identification of phasic bursts in rapid eye movements (REMs) that characterize this stage of sleep. Slow lateral eye movements may be the first manifestation of drowsiness helping to better identify sleep onset.
Leads are also placed for the recording of electromyography (EMG) activity in the chin or submental region. Submental EMG is helpful in the assessment of snoring, bruxism, and sleep stage scoring. High chin EMG tone is generally observed with wakefulness, movement, snoring, and bruxism. Typically the chin EMG tone is lowest during REM sleep.
Bilateral leg EMG recordings are useful in the diagnosis of periodic limb movements of sleep (PLMS). Additional limb EMG recordings are obtained in special circumstances.
Electrocardiogram
A single channel of electrocardiographic (ECG) activity is generally recorded using the lead II placement (right arm to left hip) giving the technologist and sleep specialist the ability to identify common cardiac arrhythmias.
Respiratory variables
Airflow variables are measured with a thermal mouth/nose sensor and nasal pressure canula. Thoracic and abdominal belts are worn by patients to record respiratory effort. An oximetry probe is used to continuously measure oxygen saturation and may be affixed to a finger or ear lobe. In addition to these recording variables, additional devices can be used to monitor end-tidal CO 2 and/or esophageal pressure. Recording of airflow, respiratory effort, and oximetry is necessary in the diagnosis of SRBDs.
Audio and video monitoring
Breath sounds, body position, and unusual behaviors or movements occurring during sleep can be recorded by means of video and audio monitoring equipment in the patient bedroom or via first-hand observation and documentation by a sleep technologist.
Body position is particularly helpful in assessment of SRBDs. Frequently, these disorders are more severe while in supine sleep, likely related to jaw and tongue position and posterior displacement, resulting in more severe obstruction. In some cases, position retraining alone to avoid the supine position may be helpful in the treatment of an SRBD.
Pretest calibration
On completion of the sensor application, electrode impedances are checked to confirm proper site preparation and adequate contact with the skin before the start of the PSG recording. A sleep technologist performs a mechanical calibration of the recording equipment and then a physiologic calibration by giving a patient various commands to confirm the correct function of certain sensors. An example is the calibration of the EOG channels, which may include having a patient open and close the eyes and look left and right and up and down.
A typical recording montage for an attended, clinical PSG performed in a sleep center is shown in Table 1 .
| Channel No. | Category | Derivation or Device |
|---|---|---|
| 1 | Left frontal lobe EEG | F3–M2 |
| 2 | Right frontal lobe EEG | F4–M1 |
| 3 | Left central lobe EEG | C3–M2 |
| 4 | Right central lobe EEG | C4–M1 |
| 5 | Left occipital lobe EEG | O1–M2 |
| 6 | Right occipital lobe EEG | O2–M1 |
| 7 | Left EOG | LOC–M2 |
| 8 | Right EOG | ROC–M1 |
| 9 | Submental EMG | EMG leads on the chin/jaw |
| 10 | Left leg EMG | EMG leads on the left anterior tibialis |
| 11 | Right leg EMG | EMG leads on the right anterior tibialis |
| 12 | ECG | Lead II ECG |
| 13 | Oral/nasal airflow | Oral/nasal thermocouple |
| 14 | Nasal pressure | Nasal pressure transducer |
| 15 | Thoracic effort | Inductance plethysmography belt |
| 16 | Abdominal effort | Inductance plethysmography belt |
| 17 | Oxygen saturation | Pulse oximetry probe |
| 18 | Heart rate (bpm) | Pulse oximetry probe |
Split-Night PSG
A clinical PSG that combines a diagnostic study with a titration study in a single night is often called a split-night study. This type of study is performed when the first 2 or 3 hours of the PSG yields an elevated apnea hypopnea index (AHI) sufficient to begin therapy. The remainder of the sleep time is then used to titrate therapy in the form of PAP or oral appliance device. A recent clinical study has confirmed that the AHI obtained in the first few hours of sleep in patients suspected of having an SRBD is an accurate representation of the AHI from a full night PSG. Many sleep centers follow the current Centers for Medicare & Medicaid Services (CMS) guideline of an estimated AHI greater than or equal to 15 or a minimum of 30 scored apnea hypopnea events within 2 hours to initiate a split-night study. For most patients, PAP titration is performed unless prior fitting for an oral appliance device has been done. Split-night studies provide convenience for patients and may reduce the overall cost of care for treatment of SRBDs.
Out-of-Center PSG
An out-of-center PSG is an unattended study performed to confirm the diagnosis of SRBDs in medically stable patients with a high pretest probability of moderate to severe SRBDs. Some unattended PSG recording systems are able to obtain data similar to an attended, in-center PSG. But many out-of-center studies, for simplicity, limit data collection to respiratory-related signals, including nasal pressure, respiratory effort, pulse rate, and oxygen saturation.
Patients undergoing out-of-center PSG are given advance instruction on the self-application of the study sensors and are also responsible for starting and stopping the study on the recording device. The recording device is then returned to the sleep center for data analysis and interpretation.
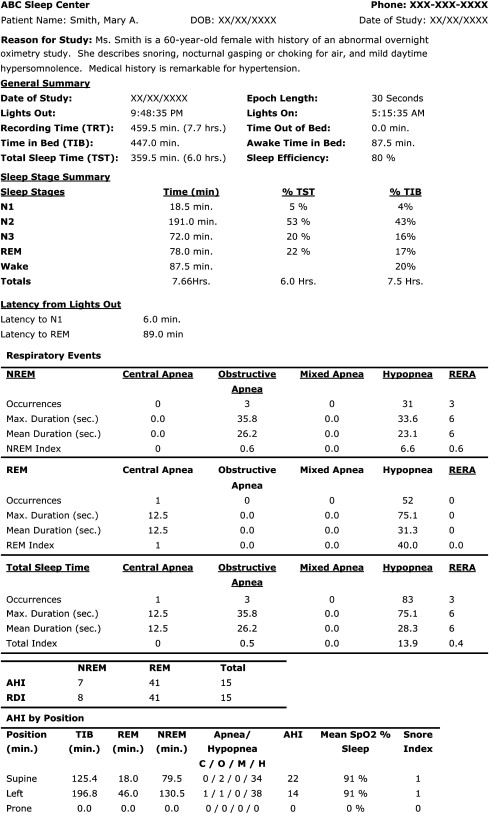
The PSG Report
An initial method for assessing the sleep cycle on a single night study is through review of the sleep hypnogram. This provides a graphic representation of the sleep stages and sleep cycles as well as a general overview of the scored sleep-related events. These may include SRBD events, arousals, and limb movements. This overview assists clinicians in obtaining an overall assessment of the PSG. Fig. 2 shows a sample PSG report, including a sleep hypnogram.