Orthodontic extrusion with multidisciplinary treatment can provide predictable outcomes in selected situations, reducing the costs and the adaptation times of gingival tissues after implant integration. Forced orthodontic extrusion is strongly related to interactions of teeth with their supportive periodontal tissues. This article reports a case of orthodontic extrusion of the maxillary incisors for later implant rehabilitation in a patient with periodontal disease. Slow forces were applied for 14 months. After this time, the teeth were extracted, and the implants were placed on the same day. Also in the same session, the provisional crown was fabricated for restoration of the anterior maxillary interdental papillae loss and for gingival contouring. Clinical and radiographic examinations at the 6-year follow-up showed successful tooth replacement and an improved esthetic appearance achieved by this multidisciplinary treatment. The decision to perform orthodontic extrusion for implant placement in adult patients should be multidisciplinary.
Periodontal disease is characterized by inflammation of the supporting tissues of the teeth, resulting in gingival recession and apical migration of the junctional epithelium with pocket formation and alveolar bone loss. In the maxillary anterior teeth, these conditions cause functional discomfort and compromise the esthetics.
Since the immune and inflammatory responses are critical factors in the pathogenesis of periodontitis and are related to countless aerobic and anaerobic bacteria, the rehabilitation of these patients becomes a challenge to the professional because of the need to restore function and especially esthetics. Unfortunately, periodontal regeneration procedures, onlay bone grafts, and mucogingival therapy do not have entirely predictable outcomes, especially when systemic disease such as diabetes mellitus is present because this condition impairs the bone healing around dental implants, mainly in relation to bone and tissue height gain in the anterior maxilla.
Orthodontic extrusion to correct periodontal infrabony defects can be successful when there is no inflammation and with adequate control of dental plaque. According to Taba et al, the success of periodontal regeneration depends on 4 elements: cells, appropriate signals, scaffold, and blood supply. The establishment of a new vascular supply is essential for periodontal regeneration because this provides nutrients for cell growth. During orthodontic extrusion, mechanical stresses exerted on the alveolar bone lead to activation of angiogenic growth factors, which would contribute to the formation of new supporting tissues. The regeneration of periodontal tissue support allows implant placement and predictable treatment results. However, it is recommended that in patients with periodontal disease, orthodontic treatment should start 2 to 6 months after periodontal therapy to allow for periodontal healing and stabilization. At the same time, light continuous forces should be implemented for efficient tooth movement in a compromised periodontium: ie, the ideal constant orthodontic forces during extrusion should allow movement of ≥2 mm per month.
According to Gkantidis et al, the harmonious cooperation of a general dentist, a periodontist, and an orthodontist offers great possibilities for successful treatment. Although there are many studies in the scientific dental literature about orthodontic extrusion, only a few cases of placing dental implants after orthodontic extrusion have been reported. Therefore, we report on a case of orthodontic extrusion of the maxillary anterior incisors to facilitate implant placement in a patient with periodontal disease.
Diagnosis and etiology
A 56-year-old woman was seen in the prosthodontic clinic in the Department of Dental Materials and Prosthodontics at Araraquara School of Dentistry, São Paulo, Brazil, for extraction of her maxillary central incisors and replacement with endosseous implants. The patient had no systemic problems and did not smoke. However, she had periodontal disease characterized by loss of supporting alveolar bone and tissue, mainly around the maxillary anterior teeth. This condition prevented the rehabilitation before a new treatment plan was considered.
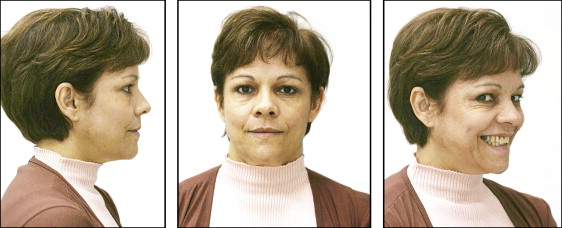
The initial facial photographs showed a Class I pattern with good facial relationships and a normal profile ( Fig 1 ). In the clinical examination, the probing pocket depth was 8 mm around the maxillary central incisors. In the other areas, probing depths ranged from 3 to 5 mm. The periodontal examination showed gingival recession of the maxillary right central and lateral incisors, canine, and first premolar, and the maxillary left central and lateral incisors, canine, and first molar ( Fig 2 ). The first appointment was scheduled for orthodontic documentation for multidisciplinary planning.

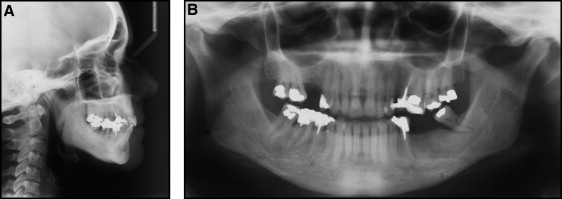
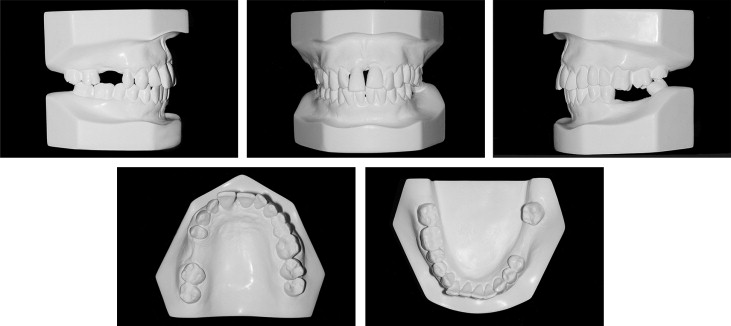
The cephalometric characteristics were normal without clinically significant skeletal deviations ( Fig 3 , A ). The panoramic radiograph showed generalized horizontal bone loss and vertical bony defects on the distal aspect of the maxillary right first premolar, the distal aspect of the mandibular right first molar, and the mesial aspect of the mandibular left third molar ( Fig 3 , B ). However, the dental casts showed a complete Class II molar relationship on the left side ( Fig 4 ).
Treatment objectives
The treatment plan consisted of 4 stages. In the first stage, periodontal therapy was provided, and plaque control was encouraged. In the second stage, orthodontic extrusion was to gain bone in the vertical direction. Therefore, it was possible to reduce the vertical bone defects around the maxillary central incisors before implant placement. The third stage consisted of extraction of the maxillary central incisors and immediate implant placement. In the fourth stage, the definitive restoration of the maxillary central incisor implants was completed.
Treatment objectives
The treatment plan consisted of 4 stages. In the first stage, periodontal therapy was provided, and plaque control was encouraged. In the second stage, orthodontic extrusion was to gain bone in the vertical direction. Therefore, it was possible to reduce the vertical bone defects around the maxillary central incisors before implant placement. The third stage consisted of extraction of the maxillary central incisors and immediate implant placement. In the fourth stage, the definitive restoration of the maxillary central incisor implants was completed.
Treatment alternatives
An alternative to orthodontic extrusion would be extraction of the anterior teeth, then implant placement followed by compensation of the defect with soft tissue and/or increasing the prosthetic crown length. This hypothesis, although immediate and without orthodontic treatment, was rejected because of the risk of marked bone loss and the possibility of unfavorable esthetic results related to papillae leveling.
The second option would be block bone graft surgery to increase the alveolar bone thickness. This procedure would favor the implant surgery and esthetics. In this case, the patient would have 2 surgeries, with the additional risk of worsening the bone loss.
Another option of more conservative treatment would be to keep the maxillary central incisors and to rehabilitate with facets. However, the esthetics in this patient would have been compromised.
Treatment progress
The initial treatment stage comprised plaque control and gingival inflammation reduction. For this patient, periodontal treatment and oral hygiene instructions were performed according to the study of Gkanditis et al. After 4 months, a careful clinical examination was performed before the orthodontic treatment.
The orthodontic treatment began by placement of fixed appliances in the maxillary arch with brackets and archwires. The maxillary right and left second molars received bonded tubes, providing comfort and the possibility of complete individualization of bonding. The maxillary right and left central incisor brackets were placed more apically to facilitate the extrusive movement. The incisal and distal surfaces of the maxillary right central incisor and the distal surface of the maxillary left central incisor were equilibrated. On the same day, a 0.014-in Nitinol wire (3M Unitek, Monrovia, Calif) was placed. One month later, treatment began in the mandibular arch with direct bonding of brackets, including the mandibular right first molar and left third molar. The mandibular central and lateral incisors did not receive brackets to prevent protrusion ( Fig 5 , A ).
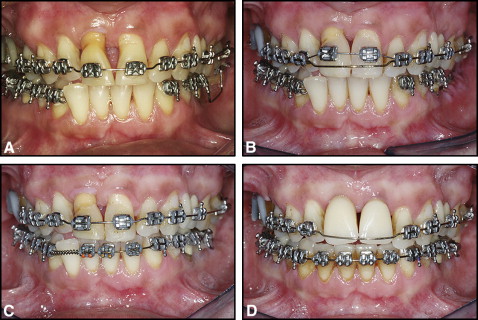
After 7 months, the mandibular left third molar became mobile and was extracted; 2 implants were placed in the region of the mandibular left first and second molars. In the next month, the brackets on the maxillary right and left central incisors were repositioned cervically, and a 0.014-in Nitinol wire was placed to potentiate the extrusion mechanics. To prevent intrusion of the anchorage teeth, an 0.018-in stainless steel auxiliary arch was used to stabilize the segmented wire ( Fig 5 , B ).
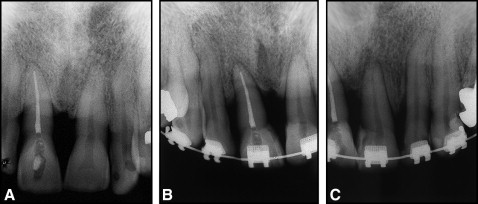
In the tenth month, implant surgery was performed in the region of the maxillary right second premolar. The periapical radiographs showed bone gain achieved by the vertical mechanical extrusion. At this time, the patient was referred for implant evaluation.
The patient was seen 2 weeks later for reduction of the incisal surfaces of the extruded teeth and apical repositioning of the lateral incisor bracket along the root surface. After 10 weeks, the segmented arch had stabilized. This eruptive stage was followed by 4 weeks of stabilization ( Fig 5 , C ). Orthodontic treatment was completed after 14 months. Radiographic examinations showed the preorthodontic and postorthodontic extrusion treatment ( Fig 6 ).