Introduction
Class III relationships can be corrected with single-jaw or bimaxillary surgery. The purpose of this research was to assess patient satisfaction after bimaxillary surgery, compared with setback surgery alone, for Class III corrections. Identifying patients’ relative levels of satisfaction will provide guidance for the selection of surgical options.
Methods
The cephalometric outcomes for 25 patients who underwent 2-jaw surgery were compared with the outcomes in 40 patients who had mandibular setback. Soft and hard tissue changes were evaluated using initial and postsurgical lateral cephalograms. The patients were asked to complete self-administered questionnaires after orthognathic treatment. Correlations between cephalometric improvement and patient satisfaction were evaluated.
Results
The patients in the 2-jaw group reported significantly higher satisfaction in the appearance of the mouth ( P <0.05), smile ( P <0.05), and treatment outcome ( P <0.001). These item scores and the changes in ANB, ANS-M, and nasolabial angle showed strong correlations in the 2-jaw group and moderate correlations in the 1-jaw group.
Conclusions
ANS-M and nasolabial angle should be considered in the conventional diagnosis of skeletal Class III orthognathic surgery to obtain adequate correction of facial esthetics and patient satisfaction. Esthetic needs contribute to surgical decisions when treating patients with skeletal Class III malocclusions and dentofacial deformities such as maxillary deficiency and long facial height that causes a turned-up upper lip.
Highlights
- •
We compared Class III patient satisfaction with bimaxillary and setback surgeries.
- •
Correlations between cephalometric improvement and patient satisfaction were evaluated.
- •
Bimaxillary patients reported significantly greater satisfaction.
- •
Decreasing ANS-M and increasing nasolabial angle increases patient satisfaction.
Skeletal Class III malocclusions have been treated by isolated mandibular setback surgery. Some researchers have reported that bimaxillary procedures are an appropriate therapy for patients with such dentofacial deformities, although there are some risks and possible complications. Thus, 2-jaw surgery has become more popular.
Concerns about airway reduction have been raised when the setback is large. Kobayashi et al stated that although the issue of relapse was not simple, a significant relapse was possible when the amount of correction exceeded 10 mm in a sagittal ramus osteotomy. Kitagawa et al suggested that the risk of sleep-disordered breathing later in life was increased in those who had had large-magnitude mandibular setback surgery.
The facial appearance was better if concurrent maxillary advancement allowed a smaller mandibular setback. Proffit et al stated that to ensure postoperative stability, the amount of mandibular setback should be restricted because of simultaneous maxillary advancement, even if this does not appear to provide a harmonious facial appearance. Jakobsone et al evaluated bimaxillary surgery stability at the 3-year recall. Noting that mandibular stability was not as good as maxillary stability, they suggested that the major risk factors for mandibular relapse were large setback and inferior repositioning of the posterior maxilla. The surgical option should be selected to achieve ideal soft tissue changes, considering esthetics, in addition to achieving adequate skeletal correction.
However, addressing patients’ complaints regarding their facial appearance is also an important objective in orthognathic surgery. Correction of the dentofacial deformity is directly related to patient satisfaction after treatment because it affects esthetics, performance, and function. Previous studies have indicated that patients may acquire a number of psychosocial benefits from orthognathic surgery. According to Pahkala and Kellokoski, skeletal Class III patients who underwent mandibular setback surgery were more satisfied than those who had mandibular advancement. Espeland et al and Mobarak et al stated that mandibular advancement surgery might be more prone to relapse vs setback, and family members might not notice a change in appearance after mandibular advancement. This may be why an inferiority complex was not eliminated in sensitive patients, especially females, according to Trovik et al.
These authors used various questionnaires and found that patients scored higher on measures of body image (especially facial and dental images) and self-esteem after orthognathic surgery. Some studies also reported that patients’ subjective quality of life was improved at 6 months after surgery. However, the lack of consensus among the various scales and tools makes it difficult to quantify the psychosocial benefits.
For disease-specific measurements, one of the most widely used questionnaires is the Oral Health Impact Profile (OHIP), which measures patients’ perceptions of the social impact of oral disorders on their well-being. The OHIP-14 questionnaire was developed as a shorter version of the OHIP-49 and covers especially oral health-specific aspects of functional limitations and physical disability, as well as psychological and social aspects of disability and handicaps. The OHIP is a reliable and valid instrument for detailed measurements of the social impact of oral disorders and has potential benefits for clinical decision-making and research.
We hypothesized that there would be no difference in satisfaction between the 1- and 2-jaw surgery groups. The aim of this study was to examine cephalometric measurements with the scales of patient satisfaction to develop a guide for the selection of 1- vs 2-jaw surgery.
Material and methods
The sample consisted of 65 Japanese skeletal Class III patients (34 female, 31 male; mean age, 24.5 years; SD, 11.1 years). This sample was selected consecutively from patients who were treated from 2008 to 2011 at Nihon University Dental Hospital in Tokyo. They were classified into 2 groups based on the following inclusion criteria.
- 1.
Mandibular setback surgery (1-jaw) group. All patients underwent a bilateral sagittal split osteotomy. There were 40 patients (21 female, 19 male; mean age, 25.6 years; SD, 9.3 years; range, 17.2-52.1 years).
- 2.
Bimaxillary surgery (2-jaw) group. All patients underwent LeFort I advancement and maxillary impaction combined with bilateral sagittal split osteotomy surgery. There were 25 patients (13 female, 12 male; mean age, 23.5 years; SD, 5.8 years; range, 18.6-38.2 years).
- 3.
All patients had surgical stabilization with internal rigid fixation using titanium mini-bone plates and monocortical screws.
- 4.
Exclusion criteria were patients with craniofacial syndromes, cleft lip and palate, or posttraumatic deformity, and patients scheduled to undergo orthognathic surgery without orthodontic treatment or with additional genioplasty or distractor devices.
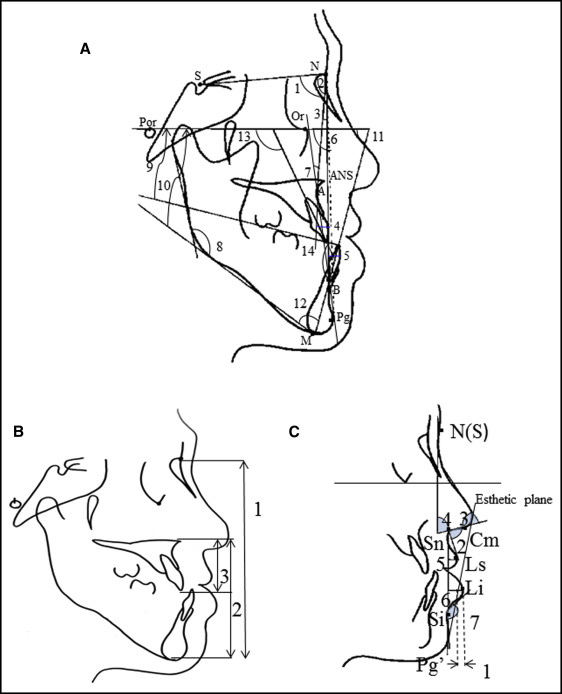
The criterion used to choose 1- or 2-jaw surgery was whether the degree of setback exceeded 10 mm at pogonion parallel to the occlusal plane in the preoperative simulation. Maxillary advancement supplemented the amount of setback if the isolated mandibular setback exceeded 10 mm. The position of maxillary Point A was determined with reference to the McNamara line. The Coben analysis was secondarily used for a proportion assay to determine the vertical position of pogonion. All patients had undergone presurgical orthodontic treatment, including leveling, space closing, and decompensation, with extraction of the 2 maxillary first premolars. The simulations involved moving the mandible or both jaws parallel to the occlusal plane until the first molars and front teeth were positioned correctly. The total setback distance was defined as the change in the anteroposterior and vertical positions of pogonion. The treatment involved 3 steps: presurgical orthodontics (T0-T1), surgery (T1-T2), and postsurgical orthodontics (T2-T3). Lateral cephalograms were taken at the initial visit (T0), before the presurgical orthodontics (T0-T1; mean, 21.0 months; SD, 5.1 months; range, 8.5-31.0 months), and after the postsurgical orthodontics (T3) at least 6 months after the surgery (T2-T3; mean, 16.5 months; SD, 4.3 months; range, 6.2-22.9 months). All radiographs were taken with the teeth in centric occlusion and the lips in repose. The initial and postsurgical cephalometric radiographs were digitized using WinCeph (version 8.0; Rise, Sendai, Japan) by one examiner (K.A.). The landmarks and reference planes are shown in the Figure . Variables were classified into angular and linear measurements ( Fig ). Modified soft tissue analyses according to the methods of Lew et al and Legan and Burstone et al were used.
All patients gave written informed consent. The study was approved by the ethics committee of Nihon University Dental Hospital (2011-3).
This study was based mainly on a specific OHIP questionnaire, the OHIP-14, with additional questions regarding paralysis and esthetics to quantify patient satisfaction after 2-jaw surgery. The satisfaction scales were then compared with those of patients who had 1-jaw surgery. Each questionnaire consisted of 14 items (Q1-Q14) to capture measures of 7 domains: functional limitations (Q1, Q2), physical pain (Q3, Q4), psychological discomfort (Q5, Q6, Q10), physical disability (Q7, Q8, Q14), psychological disability (Q9), social disability (Q11, Q12), and handicap (Q13). The questionnaire was supplemented with 2 additional items (AD-1 and AD-2), covering esthetics and loss of sensitivity postoperatively ( Table I ). Each item was scored with a 5-point Likert scale as follows: dissatisfied, 1; rather dissatisfied, 2; neither, 3; reasonably satisfied, 4; and very satisfied, 5. The higher the scores, the greater the patient’s level of satisfaction. For analysis, mean scores were derived from the scores of the individual questions. Only the question item AD-2, “loss of sensitivity,” was answered “yes” or “no.” The Mann-Whitney U test was used to evaluate questionnaire satisfaction item scores.
| Question number | Question |
|---|---|
| Q1 | How satisfied are you with your chewing ability? |
| Q2 | How satisfied are you with your pronunciation? |
| Q3 | How satisfied are you with the problems with your temporomandibular joints? |
| Q4 | How satisfied are you with your headaches because of problems with your teeth or mouth? |
| Q5 | How satisfied are you with your self-consciousness because of your teeth or mouth? |
| Q6 | How satisfied are you with the appearance of your teeth or mouth? |
| Q7 | How satisfied are you with eating your meals? |
| Q8 | How satisfied are you with your smile? |
| Q9 | How satisfied are you with your relaxation? |
| Q10 | How satisfied are you with the change in embarrassment because of problems with your teeth or mouth? |
| Q11 | How satisfied are you with the change of being irritable with other people because of problems with your teeth or mouth? |
| Q12 | How satisfied are you with doing your usual jobs? |
| Q13 | How satisfied are you with your treatment outcome? |
| Q14 | How satisfied are you with your ability to function? |
| AD-1 | How satisfied are you with your facial esthetics? |
| AD-2 ∗ | Do you have a loss of sensitivity in your lips, tongue, or other facial area? |
Statistical analysis
A pretest was conducted on 30 patients to evaluate whether they fully understood the questions and whether any terms or expressions needed to be changed. Within 3 months after active treatment, the patients were asked to complete the self-administered questionnaires regarding the impact of the surgery and the influence of the treatment on their satisfaction.
The reproducibility of the measurements was determined by selecting 10 cephalograms at random and repeating the tracing by the same examiner 1 month after the initial tracing. The Kolmogorov–Smirnov test was used to assess whether the samples had a normal distribution. The effects of age (years) and sex (1, male; 2, female) were also considered.
Descriptive statistics were generated for both the initial and the postsurgical cephalometric measurements using SPSS software (version 16.0; SPSS Japan, Tokyo, Japan). Initial tests for normality were performed to determine whether parametric or nonparametric univariate analysis for the continuous variables was appropriate. Differences between the 2 groups in each cephalometric measurement were evaluated using paired t tests. The results were considered significant if P <0.05 and highly significant if P <0.001.
The Wilcoxon rank sum test (Mann-Whitney U test) was performed to examine differences in the satisfaction scores between the 1- and 2-jaw groups because the questionnaire could not determine a normal distribution. Then Spearman correlation analysis was used to assess the degree of correlation between the postsurgical satisfaction scores and the soft and hard tissue changes. In all comparisons, P values <0.05 were considered to indicate statistical significance.
The magnitudes of the statistical differences in the cephalometric measurements and satisfaction scores were calculated for effect sizes and power using the means and standard deviations of the pooled scores.
Results
The distribution of subjects by primary diagnosis is shown in Table II . Maxillary hypoplasia was present in 16% of the 2-jaw group and 7.5% of the 1-jaw group. There were no significant differences between the 2 groups related to the number of subjects who were diagnosed with maxillary hypoplasia and mandibular hyperplasia. No intraexamination error was found in the 10 selected subjects. The participation rate was 100%. In total, 65 adults who underwent 1- or 2-jaw surgery agreed to participate in the study; no Class III patient undergoing maxillary or mandibular surgery during the actual period either refused to take part in the study or had insufficient medical records.
| One-jaw group (n = 40) | Two-jaw group (n = 25) | |||
|---|---|---|---|---|
| Maxillary | Mandibular | Maxillary | Mandibular | |
| Hypoplasia | 7.5 | 0 | 16 | 0 |
| Hyperplasia | 37.5 | 87.5 | 4 | 80 |
| Within ±1 SD | 55 | 12.5 | 80 | 20 |
There were no differences in the SNB angles between the 2 groups at T0 and T3 ( Table III ). There were also no significant differences in the facial angle and convexity angle between the groups at T0 and T3, showing similar changes in accordance with the mandibular setback procedure.
| Variable | Initial (T0) | P | Postoperatively (T3) | P | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| One-jaw group (n = 40) | Two-jaw group (n = 25) | One-jaw group (n = 40) | Two-jaw group (n = 25) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Hard tissue variables | ||||||||||
| SNA (°) | 82.4 | 3.5 | 79.8 | 3.9 | ∗ | 82.5 | 3.3 | 82.8 | 2.1 | |
| SNB (°) | 85.4 | 3.4 | 84.4 | 3.9 | 81.0 | 3.4 | 80.1 | 2.9 | ||
| ANB (°) | −3.1 | 2.2 | −4.6 | 3.2 | ∗ | 1.5 | 2.7 | 2.7 | 2.4 | ∗ |
| U1-NA (mm) | 7.9 | 3.1 | 10.5 | 2.9 | † | 3.9 | 2.2 | 6.1 | 2.6 | † |
| L1-NB (mm) | 5.9 | 2.9 | 2.7 | 4.0 | † | 4.8 | 2.4 | 5.3 | 2.0 | |
| Facial angle (°) | 94.2 | 3.4 | 94.3 | 0.7 | 90.4 | 3.5 | 89.2 | 4.1 | ||
| Convexity (°) | −3.7 | 6.6 | −5.1 | 11.0 | −0.9 | 5.2 | 0.6 | 5.9 | ||
| Gonial angle (°) | 128.6 | 7.9 | 131.9 | 12.2 | 129.0 | 8.2 | 129.6 | 7.4 | ||
| Occlusal plane to FH (°) | 7.8 | 5.7 | 7.5 | 9.0 | 8.5 | 5.4 | 11.5 | 4.4 | ∗ | |
| FMA (°) | 26.2 | 6.0 | 31.3 | 5.6 | † | 27.7 | 5.4 | 32.5 | 6.0 | † |
| FMIA (°) | 73.1 | 5.9 | 66.3 | 7.8 | † | 69.6 | 7.9 | 63.1 | 11.1 | † |
| IMPA (°) | 80.6 | 6.2 | 82.4 | 11.3 | 82.4 | 6.4 | 84.0 | 5.5 | ||
| U1-FH (°) | 121.7 | 7.2 | 126.4 | 8.7 | ∗ | 116.9 | 7.3 | 115.5 | 5.3 | |
| Interincisal angle (°) | 134.4 | 8.8 | 128.7 | 9.9 | ∗ | 132.0 | 8.1 | 125.7 | 5.6 | ∗ |
| Vertical variables (mm) | ||||||||||
| N-M | 137.3 | 4.4 | 137.0 | 6.2 | 138.3 | 4.0 | 133.9 | 9.4 | ||
| ANS-M | 75.4 | 3.3 | 76.7 | 3.5 | 74.9 | 2.3 | 73.5 | 5.9 | ||
| ANS-U1 | 29.9 | 3.0 | 28.0 | 1.8 | ∗ | 29.8 | 2.7 | 28.2 | 3.6 | |
| Soft tissue variables | ||||||||||
| Lower lip–E-line (mm) | −3.8 | 1.5 | −5.0 | 2.0 | ∗ | −1.0 | 3.2 | 0.4 | 2.2 | |
| Nasolabial angle (°) | 94.8 | 7.3 | 91.3 | 5.9 | ∗ | 97.8 | 3.2 | 100.7 | 3.3 | † |
| Nasal tip (°) | 79.0 | 5.9 | 82.2 | 4.6 | ∗ | 78.1 | 8.8 | 86.8 | 11.4 | † |
| Nasal columella (°) | 65.9 | 7.0 | 68.5 | 2.6 | 65.4 | 9.0 | 62.8 | 4.5 | ||
| Upper lip distance (mm) | 5.7 | 1.4 | 5.3 | 1.2 | 5.3 | 2.4 | 6.4 | 1.4 | ∗ | |
| Lower lip distance (mm) | 7.2 | 1.9 | 8.7 | 1.1 | † | 4.2 | 1.8 | 5.4 | 2.4 | ∗ |
| Inferior labial sulcus angle (°) | 126.8 | 4.2 | 124.2 | 6.2 | 129.7 | 13.9 | 127.8 | 10.2 | ||
The 2-jaw group had a smaller SNA angle only at T0, indicating a maxillary deficiency that resulted in the smaller ANB angle ( P <0.05). In the initial cephalometric analysis (T0), patients in the 2-jaw group had more severe Class III skeletal discrepancies than did those in the 1-jaw group ( Table III ). The maxillary central incisor to Frankfort horizontal angle in the 2-jaw group at T0 was significantly greater ( P <0.05) than that in the 1-jaw group, so that the nasolabial angle was smaller ( P <0.05). By contrast, at T3, there were no significant differences between the 2 groups. Patients in the 2-jaw group at T0 had high-angle faces, with significantly greater FMA angles ( P <0.01); they still had a greater FMA angle at T3 ( P <0.01). The nasolabial angle in the 1-jaw group was greater at T0 than at T3 ( P <0.05), whereas in the 2-jaw group, it was greater at T3 ( P <0.01). The nasal tip increased greatly in the 2-jaw group after the surgery, so that the statistical significance of the difference between groups was greater at T3 ( P <0.01).
In the 2-jaw group, significant decreases in the hard tissue measurements were observed, including the facial angle ( P <0.05), maxillary incisor to Frankfort horizontal angle ( P <0.05), and ANS-M ( P <0.001), and in the soft tissue measurement of the nasal columella angle ( P <0.01) at T3-T0 ( Table IV ). Significant increases were also found in hard tissue parameters, including SNA angle ( P <0.05), ANB angle ( P <0.01), convexity angle ( P <0.01), and occlusal plane to Frankfort horizontal angle ( P <0.01), and in soft tissue measurements, including the lower lip to E-line ( P <0.01), nasolabial angle ( P <0.001), and nasal tip ( P <0.01) in the 2-jaw group. By contrast, the FMA angle did not differ significantly between the 2 groups.
| T3-T0 | P | Effect size d | Power 1-β | ||||
|---|---|---|---|---|---|---|---|
| One-jaw group (n = 40) | Two-jaw group (n = 25) | ||||||
| Mean | SD | Mean | SD | ||||
| Hard tissue variables | |||||||
| SNA (°) | 0.1 | 2.2 | 3.0 | 3.8 | ∗ | 0.93 | 0.98 |
| SNB (°) | −4.5 | 2.7 | −4.3 | 4.2 | 0.23 | 0.22 | |
| ANB (°) | 4.6 | 4.6 | 7.3 | 3.9 | † | 0.63 | 0.79 |
| U1-NA (mm) | −4.0 | 3.1 | −4.4 | 2.4 | 0.14 | 0.14 | |
| L1-NB (mm) | −1.2 | 2.8 | 2.6 | 4.5 | † | 1.01 | 0.98 |
| Facial angle (°) | −3.8 | 1.5 | −5.1 | 3.5 | ∗ | 0.48 | 0.59 |
| Convexity (°) | 2.8 | 5.5 | 5.7 | 3.1 | † | 0.64 | 0.8 |
| Gonial angle (°) | 0.4 | 4.3 | −2.3 | 8.9 | 0.31 | 0.33 | |
| Occlusal plane to FH (°) | 0.7 | 2.1 | 4.0 | 3.9 | † | 1.05 | 0.99 |
| FMA (°) | 1.5 | 4.8 | 1.2 | 4.5 | 0.06 | 0.08 | |
| FMIA (°) | −3.5 | 9.1 | −4.9 | 9 | 0.15 | 0.15 | |
| IMPA (°) | 1.8 | 8.8 | 1.6 | 10.2 | 0.18 | 0.57 | |
| U1-FH (°) | −4.8 | 5.2 | −10.9 | 4.3 | 0.63 | 0.79 | |
| Interincisal angle (°) | −2.4 | 5.1 | −2.9 | 6.1 | 0.44 | 0.7 | |
| Vertical variables (mm) | |||||||
| N-M | 1.0 | 4.9 | −3.1 | 8 | 0.61 | 0.77 | |
| ANS-M | −0.5 | 2.4 | −3.2 | 3.1 | ‡ | 1.01 | 0.98 |
| ANS-U1 | −0.1 | 4.2 | 0.2 | 4.2 | 0.17 | 0.16 | |
| Soft tissue variables | |||||||
| Lower lip–E-line (mm) | 2.8 | 3.6 | 5.4 | 3 | † | 0.78 | 0.91 |
| Nasolabial angle (°) | 3.0 | 4.5 | 9.4 | 4.5 | ‡ | 1.03 | 0.99 |
| Nasal tip (°) | −1.1 | 8.2 | 4.6 | 5.5 | † | 1.81 | 1 |
| Nasal columella (°) | −0.5 | 8.2 | −5.7 | 5.8 | † | 0.64 | 0.8 |
| Upper lip distance (mm) | −0.4 | 1.8 | 1.1 | 1.6 | † | 0.8 | 0.92 |
| Lower lip distance (mm) | −3.0 | 2.7 | −3.3 | 2 | 0.12 | 0.12 | |
| Inferior labial sulcus angle (°) | 2.9 | 8.7 | 3.5 | 7.9 | 0.7 | 0.8 | |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


