Introduction
The aim of this study was to evaluate the reparative potential of cementum histologically after intentional root contact with a temporary skeletal anchorage device.
Methods
Seventeen patients (8 male, 9 female; mean age, 16.2 years; range, 13.5-21.6 years) who were scheduled for extraction of 4 first premolars as part of their orthodontic treatment participated in this study. The roots of the premolars were intentionally injured with a temporary skeletal anchorage device. The teeth were extracted at 4, 8, or 12 weeks after the injury. Root contact with the temporary skeletal anchorage device was confirmed by using a stereomicroscope. Histologic samples were prepared. Demineralized serial sections were stained with eosin and hematoxylin, and cementum repair was assessed histomorphometrically.
Results
Despite varying depths of the injuries, including involvement of dentin, reparative cementum formation was observed in all sections. Healing cementum was almost exclusively of the cellular type; 70% of all the teeth exhibited good repair by the end of week 12.
Conclusions
This study established that healing of cementum takes place after an injury with a temporary skeletal anchorage device, and it is a time-dependent phenomenon.
Temporary skeletal anchorage devices have become popular adjuncts in clinical orthodontics because they offer several advantages, including sufficient anchorage for noncompliant patients, simplicity of insertion and removal, relatively low cost, and versatility in clinical applications.
The ability to obtain absolute anchorage through bone-anchored devices has enabled orthodontists to eliminate the unwanted side effects associated with conventional approaches and to correct malocclusions that previously required complicated biomechanics or orthognathic surgery.
Although these devices are available in several sizes and shapes, the most popular and widely used temporary skeletal anchorage device appears to be the miniscrew. They can be placed in several convenient locations, and the most preferred site appears to be the interradicular bone between the roots of adjacent teeth; however, placement carries with it the risk of iatrogenic damage to the adjacent roots. Root damage can occur from either improper placement of the temporary skeletal anchorage device, migration after loading, axial deviation during insertion, anatomic variation in root form, or tooth contact with the temporary skeletal anchorage device during orthodontic treatment. Although the literature includes case reports highlighting various clinical applications of temporary skeletal anchorage devices, there is little information regarding iatrogenic damage to tooth roots that are injured during their placement or use.
Asscherickx et al conducted experiments on beagle dogs and reported that healing takes place in approximately 12 weeks after root damage with temporary skeletal anchorage devices, and healing was nearly complete after 20 weeks. In a classic animal study, Chen et al found higher failure rates when temporary skeletal anchorage devices contacted the roots. They also reported repair of roots by cementum deposition and bone regeneration when the temporary skeletal anchorage devices were removed and the roots were allowed to heal. Both of these studies were in animals, and it is questionable whether the same outcomes can be extrapolated to humans. The best information on root damage and subsequent healing in human subjects emanates from studies pertaining to the use of small screws for the fixation of mandibular fractures and osseous segments placed during maxillofacial surgery. Although fixation screws are similar to the temporary skeletal anchorage devices used in orthodontics, they are usually not placed in interradicular areas.
Few clinical studies have addressed damage to the roots either during or after temporary skeletal anchorage device placement. This information is limited to case reports or case-series studies, often without sufficient sample sizes. To our knowledge, no study has assessed cementum repair after root contact with temporary skeletal anchorage devices in humans. In view of the current evidence, it is logical to assume that only partial repair occurs after injury with temporary skeletal anchorage devices. This research was designed to validate this hypothesis.
The aims of this prospective study were to establish the healing potential of the root cementum histologically and histomorphometrically after intentional root damage with a temporary skeletal anchorage device, and to determine the differences in healing potential after 4, 8, and 12 weeks in human subjects. We hypothesized that there would be no marked difference in healing between the various phases of healing after damage to the roots, and at best the repair would be incomplete or partial.
Material and methods
Patients who reported to the Department of Orthodontics at Ragas Dental College and Hospital, Chennai, India, between January and June 2009 were screened for the study. Seventeen patients (8 male, 9 female; mean age, 16.2 years; range, 13.5-21.6 years) who had a severe arch length-tooth size discrepancy warranting first premolar extractions for routine orthodontic fixed appliance treatment were considered for the study. Patients on medication for systemic disorders, pregnancy, or steroid therapy were eliminated from the study. All such adult patients and the parents of those under the age of 18 years received explanations about the study protocol, and their consent was obtained.
The study protocol was approved by the institutional research ethics committee. The ethical consideration in this study was of intentionally inserting a temporary skeletal anchorage device on the first premolar roots in clear-cut extraction cases. This study should be comparable with experimental setups in recent histologic and scanning electron microscope studies on the incidence and repair of root resorption after the application of heavy forces with orthodontic springs to move the teeth against compact cortical bone and in caries studies when premolars were used as in-vivo cariogenic models.
Selection criteria included children and adolescents in the permanent dentition with no history of orthodontic treatment, no caries lesions, and no periodontal breakdown or periapical pathology of the first premolar to be contacted with the temporary skeletal anchorage device, and in which root formation was complete.
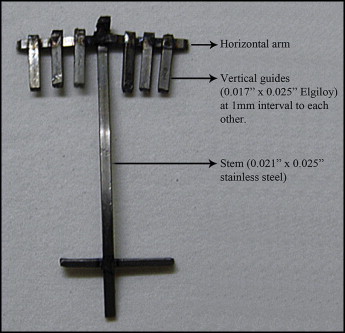
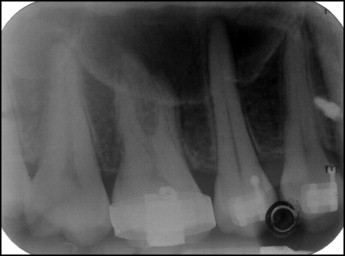
A periapical radiograph (paralleling cone technique) was taken to assess the length of the first premolar for the fabrication of a custom-made wire guide ( Fig 1 ). The guide comprised a stem of 0.021 × 0.025-in stainless steel to one end of which a horizontal arm was welded. The horizontal arm carried a series of vertical guides made of 0.017 × 0.025-in cobalt-chromium alloy wire welded at intervals of 1 mm to each other.
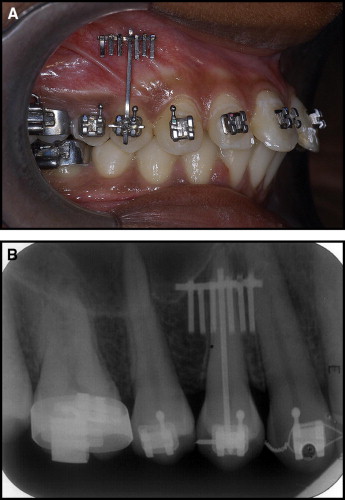
The wire guide permitted the seating of the stem in the first premolar bracket to stabilize it and allowed the horizontal arm to rest in the gingival sulcus ( Fig 2 , A ). A periapical radiograph (paralleling cone technique) was taken again after the wire guide was stabilized in the first premolar bracket to determine the placement of the temporary skeletal anchorage device, if necessary adjustments were made in the wire guide to ensure root contact ( Fig 2 , B ). The image of the wire guide on the periapical radiograph for root contact was verified clinically with the vertical guides facilitating the required mesiodistal positioning of the temporary skeletal anchorage device ( Fig 3 ).
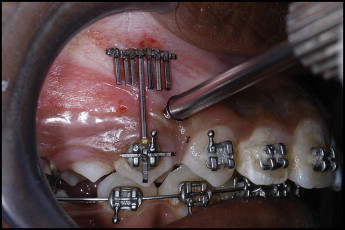
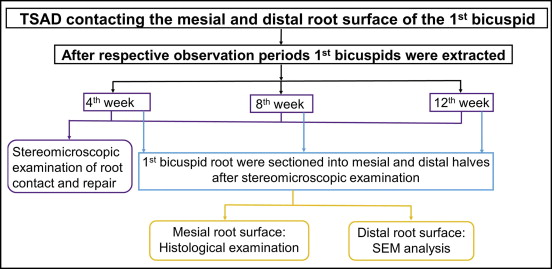
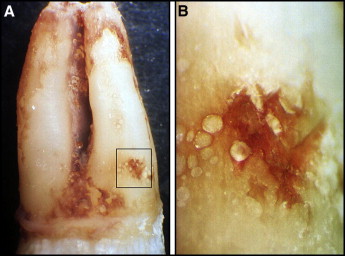
The temporary skeletal anchorage devices used for intentional root contact were a self-drilling design, 1.5 mm in diameter and 8 mm in length (Dentos, Daegu, Korea). For each patient, 1 temporary skeletal anchorage device was inserted on the mesial side and the other on the distal side of the buccal root surface of the first premolar. Both were inserted under local anesthesia (2% lignocaine with 1:100,000 epinephrine) on the same day based on the radiographic assessment. A hole of 0.9 mm in diameter was drilled with a number 2 round bur to make an indentation through the cortex with a slow-speed hand piece under continuous saline-solution irrigation. Care was taken to ensure that there was only 1 contact. The temporary skeletal anchorage devices were placed by using a manual torque tester. The resistance felt during placement indicated that contact with the root had occurred, and this was further confirmed with a periapical radiograph ( Fig 4 ). The temporary skeletal anchorage devices were immediately removed after establishing root contact. The repair of the periodontal apparatus and the root structure that was damaged was allowed to take place for varying lengths of time. Based on the healing period, the teeth were classified as 4, 8, or 12 weeks. The experimental design is shown in Figure 5 . Immediately after extraction, the damaged surfaces were identified on the mesial and the distal root surfaces of the first premolar by using a stereomicroscope (Laborlux B; Wetzlar, Germany) ( Fig 6 ).
The root was bisected into mesial and distal segments with a diamond-coated disk, taking necessary precautions to ensure that the intentional root defect caused by contact with the temporary skeletal anchorage device was not adjacent to the disk. The mesial segments were placed in 10% neutral buffered formalin and fixed for 48 hours. They were completely decalcified in 10% ethylenediaminetetraacetic acid. After ensuring complete decalcification, the roots were embedded in paraffin blocks. Serial sections 5 μm thick through the axiobuccolingual direction were stained with hematoxylin and eosin for histologic examination. The distal segment was stored and examined with a scanning electron microscope; this outcome will be reported separately.
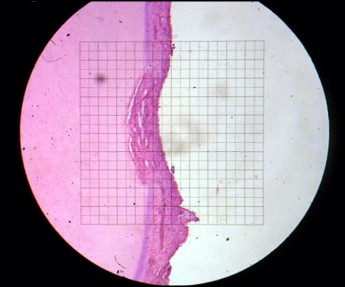
From the mesial root segment, approximately 300 μm of the mesiodistal width of the teeth was examined by an author (K.S.A.V.) by light microscopy ( Fig 7 ). The areas of damage and repair were histomorphometrically measured by using a previously published method. Histomorphometric analysis was carried out at 10 times magnification with a light microscope by using a 10-mm square grid that divided the field into 100 equal parts. The grid was placed over the area of damage. The intersecting squares of the damaged area were counted. Only squares that involved more than 50% were counted. Similarly, the numbers of squares in the areas of healing were calculated. For each section, the repair was expressed as a percentage of the ratio of the repaired area to the damaged area.
The mean repair was calculated for each tooth by using a software package (Excel; Microsoft, Redmond, Wash). Healing of the cementum was further graded as mild (≤33.33%), moderate (33.33%-66.66%), good (66.66%-90%), or excellent (≥90%). The patients’ ages were classified as above and below 16 years. Patient demographics of age, sex, healing period in weeks, and the mean repair were analyzed by using SPSS software (version 16.0; SPSS, Chicago, Ill). Descriptive statistics included age, standard deviation, range, sex, and frequency as percentages. The Kruskal-Wallis test was done to assess repair of the cementum by grades in the various phases. Comparisons of mean healing percentages for the different periods of the study were performed with one-way analysis of variance (ANOVA). The post-hoc test of Bonferroni was used to assess the mean difference. A P value of 0.05 or less was considered to be statistically significant.
Results
Seventeen subjects (68 teeth) fulfilling the inclusion and exclusion criteria were enrolled for this prospective study. No subject complained of undue pain after the trauma. Extraction of 1 first premolar was done in weeks 4, 8, and 12. Seventeen teeth were planned for extraction in weeks 4, 8, and 12. In weeks 4 and 8, 17 teeth were extracted as planned. However, it was possible to extract only 14 teeth in week 12. Premature extractions were required in the remaining 3 patients before week 12 for their orthodontic treatment to progress. The remaining first premolars were extracted according to the protocol and were not included in the study. Hence, 48 teeth were included in the study.
Stereomicroscopic examinations confirmed the root damage and subsequent healing in all the samples. Table I indicates the number of teeth and subjects who had extractions during the study period. Nearly 50% of the patients (n = 8) showed repair greater than 50% by weeks 4 and 8, whereas only 1 subject had repair less than 50%. These findings indicate that most of the repair took place by week 8 ( Figs 8 and 9 ).
| Week 4 | Week 8 | Week 12 | |
|---|---|---|---|
| Sex | |||
| Male | 8 | 8 | 7 |
| Female | 9 | 9 | 7 |
| Age group | |||
| <16 y | 6 | 6 | 5 |
| ≥16 y | 11 | 11 | 9 |
| Overall | 17 | 17 | 14 |
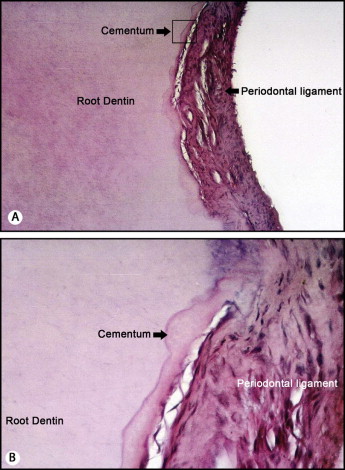
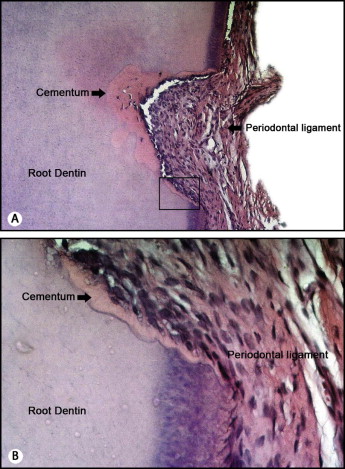
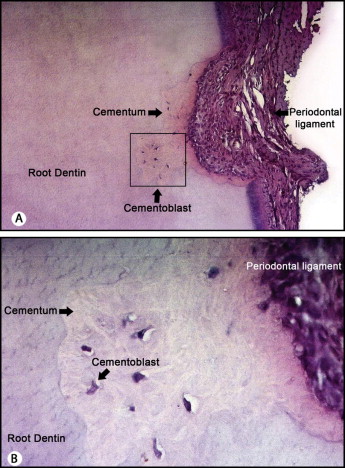
Of the 48 teeth evaluated histologically, it was evident that the dentin in all specimens was damaged, although the quanta of damage and repair were variable. No pulpal damage or evidence of root resorption (internal or external) was seen in any histologic section. There was no ankylosis as evidenced by extraction of the teeth and the clinical test of extrusion. The teeth exhibited a normal repair process by recruitment of cells that suggested cementoblasts (as evidenced by the processes of cementoblasts) ( Fig 10 ). The periodontium appeared to cover the defect area.