Treatment of children with several congenitally missing teeth is challenging, because growth and development of the oral structures must be considered. The treatment options include retaining the deciduous teeth and postponing treatment until later or extracting the deciduous teeth and doing one of the following: allowing the space to close spontaneously, closing the space orthodontically, or in patients whose growth is finished, using a prosthetic or implant replacement. One other viable option, if donor teeth are available, is autotransplantation. The treatment plan for patients with missing teeth should be based on a comprehensive evaluation of the patient’s age, occlusion, and space requirements as well as on the size and shape of the adjacent teeth. This case report presents the management of a patient in the early mixed dentition with multiple missing teeth. The treatment consisted of a combination of autotransplantation of the maxillary right first premolar to the mandibular right first premolar region and orthodontic treatment with a 5-year follow-up after autotransplantation.
Congenitally missing premolars are often a diagnostic challenge to the orthodontist. With autotransplantation, it is possible to solve complicated treatment problems in the dental arches. Autotransplantation of immature premolars is a viable method of restoring edentulous areas in young patients whose alveolar growth is not yet complete. This method can potentially replace a missing tooth with a natural tooth rather than with a prosthesis or an osseointegrated implant.
Autotransplantation of premolars with partly formed roots has been reported to be a predictable treatment modality. This is because transplanted teeth also have the capacity for functional adaptation and preservation of the alveolar ridge. Premolars can be transplanted from 1 site in a crowded arch to another site to replace congenitally absent premolars.
This case report presents the management of a patient with multiple missing teeth in the early mixed dentition. It describes a conservative treatment approach: autotransplantation of the maxillary right first premolar to the mandibular right first premolar region was combined with orthodontic treatment.
Diagnosis and etiology
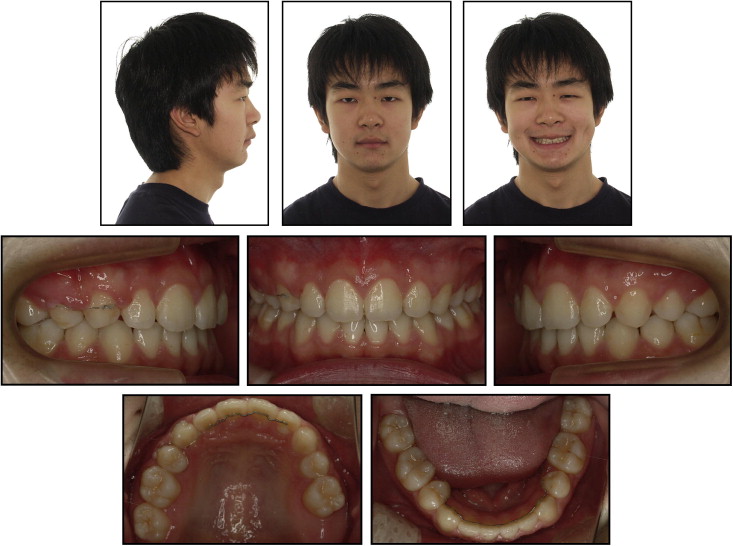
The patient was a 9-year-old boy with an unremarkable medical history. No signs or symptoms of temporomandibular disorders were reported. His general dentist referred him for orthodontic consultation. Pretreatment records showed that the patient had normal vertical facial proportions and good facial symmetry.
His profile was convex. On clinical examination, the boy was found to be in the early mixed dentition stage. Analysis of the study models disclosed a mesial-step molar occlusion on both sides. The erupting maxillary left central incisor had a 3.7-mm overjet and a 3.2-mm overbite. No crossbites were noted. The dental midline was coincident with the facial midline ( Figs 1-3 ). A pretreatment panoramic radiograph showed agenesis of the maxillary left second premolar, the mandibular right first premolar, and the mandibular left and right second premolars. Considering his age, the maxillary right second premolar tooth bud was developing slowly, and the maxillary first molars were erupting slowly. There were no radiographic signs of the maxillary second and third molars in the initial records ( Fig 3 , A ).

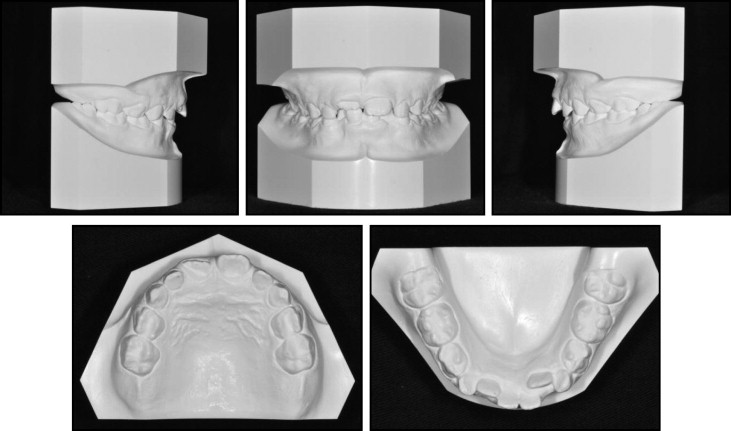
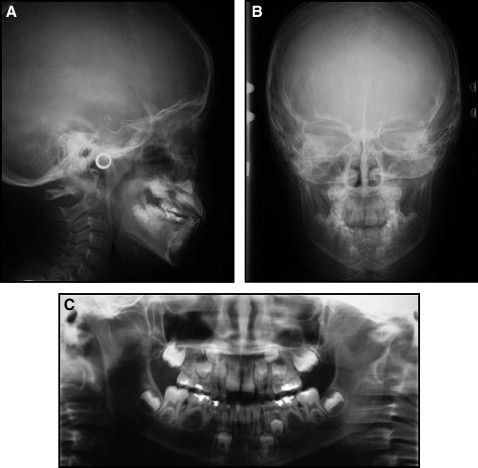
Cephalometric analysis indicated a Class II skeletal pattern (ANB, 7.7°) with a hyperdivergent growth pattern (SN-MP, 39.9°). The maxillary incisors were normally inclined, and the mandibular incisors showed a slight proclination ( Table ; Fig 3 , B ). The etiology of the patient’s malocclusion and missing teeth was probably genetic, because no history of trauma or infection to the mouth, teeth, or jaws was reported.
| Measurement | Japanese norm | Pretreatment | Posttreatment | 26 mo posttreatment |
|---|---|---|---|---|
| SNA (°) | 82.0 | 83.7 | 85.2 | 84.5 |
| SNB (°) | 80.0 | 76.0 | 80.9 | 80.6 |
| ANB (°) | 2.0 | 7.7 | 4.3 | 3.9 |
| Wits (mm) | 1.1 | −3.6 | 2.0 | −3.4 |
| SN-MP (°) | 32.0 | 39.9 | 38.1 | 39.5 |
| FH-MP (°) | 25.0 | 28.2 | 28.4 | 28.6 |
| LFH (ANS-Me/N-Me) (%) | 55.0 | 57.6 | 57.3 | 57.5 |
| U1 to SN (°) | 104.0 | 103.4 | 96.5 | 97.0 |
| U1 to NA (°) | 22.0 | 19.7 | 12.3 | 12.4 |
| IMPA (°) | 90.0 | 94.4 | 87.2 | 86.5 |
| L1 to NB (°) | 25.0 | 30.3 | 23.6 | 23.4 |
| U1/L1 (°) | 124.0 | 122.3 | 137.5 | 137.7 |
| Upper lip (mm) | 1.2 | 3.9 | 1.0 | 2.0 |
| Lower lip (mm) | 2.0 | 1.3 | −2.1 | −1.3 |
Treatment objectives
Autotransplantation of teeth can significantly reduce treatment time in certain patients with aplasia, tooth loss, or ectopia when a suitable tooth is available and the anatomic conditions allow for it. In this study, the treatment plan included transplanting the maxillary right first premolar in the mandibular right first premolar region, extracting all retained deciduous teeth and closing the space. The objective was to achieve Class I molar and canine relationships on both sides and normal overjet and overbite.
Due to skeletal discrepancies that resulted from an unfavorable growth pattern, surgical treatment could be an option in the future, including genioplasty, after the patient’s growth is complete.
Treatment objectives
Autotransplantation of teeth can significantly reduce treatment time in certain patients with aplasia, tooth loss, or ectopia when a suitable tooth is available and the anatomic conditions allow for it. In this study, the treatment plan included transplanting the maxillary right first premolar in the mandibular right first premolar region, extracting all retained deciduous teeth and closing the space. The objective was to achieve Class I molar and canine relationships on both sides and normal overjet and overbite.
Due to skeletal discrepancies that resulted from an unfavorable growth pattern, surgical treatment could be an option in the future, including genioplasty, after the patient’s growth is complete.
Treatment alternatives
There are several treatment alternatives for patients with congenitally missing teeth. Extracting the deciduous teeth to allow spontaneous space closure is a conservative treatment option that can be considered for missing teeth. According to Bjerklin and Bennett, retaining the deciduous teeth is also a possible option for dental aplasia. They reported that the rate of resorption of the deciduous teeth diminishes with age; clinically, no further root resorption is evident after age 20.
Another alternative for a patient with congenitally missing teeth is replacement with implants. In growing patients, however, implants impede normal growth of the alveolar process and are contraindicated. For this reason, if implant replacement is the treatment option of choice, lengthy space maintenance would be necessary and could be accomplished by using a conventional fixed bridge. However, in adolescents, preparation of the abutment teeth might need to be delayed because of the size of the pulp chamber. Alternative space maintenance with a removable prosthesis is also problematic because of its temporary nature and the need for periodic replacement caused by patient growth. Although a resin-bonded fixed bridge is another option, it also has disadvantages, because of the irreversible tooth preparation that is required and the uncertain longevity of this type of prosthesis. All treatment alternatives were explained to our patient and his parents.
Treatment progress
Tooth transplantation and an orthodontic approach were chosen to solve the occlusal problems and to close the spaces corresponding to the missing teeth. Informed consent was obtained. A panoramic film was taken with a metal ball in place to estimate the amount of magnification before the transplantation. The proper size of the recipient site was calculated when adjusted for magnification. The patient’s development was checked every 3 months to monitor tooth eruption. Autotransplantation was performed when he was 11 years 7 months old. The mandibular right first deciduous molar was removed under local anesthesia, and the socket was fully prepared with care to preserve the buccal and lingual alveolar bone during extraction. The intra-alveolar septum was trimmed with a chisel, and the socket was irrigated.
To allow for the physiologic mesial drift of mandibular permanent molars with congenitally missing mandibular second premolars, controlled slicing of the mandibular second molars was followed by hemi-section of the distal portion of the teeth. After the mandibular right first deciduous molar and the maxillary first and second deciduous molars were extracted, then the donor tooth (maxillary right first premolar) was carefully removed, keeping the root and remaining periodontal ligament intact and untouched to avoid separation of Hertwig’s epithelial root sheath. At this time, root development was about 75%.
Autotransplantation of tooth germs at 75% to 100% of the root length with a wide-open apical foramen (root development in stages 3 to 4 according to Moorrees et al ) is recommended. As quickly as possible, the transplanted tooth germ was placed in the socket prepared for it slightly below the occlusal plane. Inadequate buccolingual width of the alveolar process made it necessary to leave the transplant in a rotated position. The flaps were sutured with 4-0 nylon sutures, and the transplant was fixed with the same suture material crossing the occlusal surface. Occlusal adjustment of the implanted tooth was done to eliminate the possibility of premature contacts. Chlorhexidine rinse and amoxicillin were prescribed for a week, and the patient was not allowed to chew on the transplant side during the first month of the postoperation period.
After this period, the patient was allowed to start chewing soft foods for 1 month and gradually increase the chewing load to normal function within 3 months. He was examined on the first postoperative day to determine whether the transplant had retained its position. The stability and the position of the transplant were then inspected weekly. Sutures were removed a week after transplantation. After that, composite adhesives and a flexible stabilization wire were used to connect the transplanted tooth to the adjacent teeth. Clinical and radiographic examinations were conducted at 1, 4, and 12 weeks, and 6 months after surgery. Pulpal healing and signs of pulp canal obliteration were evaluated. Periodontal healing, root growth, and tooth eruption after the transplantation were also monitored by radiographic examinations. Nine months after the autotransplantation, the mesial portions of the mandibular second deciduous molars were extracted, and active orthodontic treatment was started before pulp canal obliteration. Little root growth was observed during this period, with the crown-to-root ratio steady at nearly 1:1. A periodontal ligament space and a lamina dura were observed.
After carefully observing the response of the transplanted tooth, 0.018 edgewise brackets (3M Unitek, Monrovia, Calif) were bonded in both arches. To minimize the extrusive effect of the maxillary first permanent molars and to correct the anteroposterior skeletal discrepancies during treatment, a high-pull headgear was used. At the end of active orthodontic treatment, the radiographic examination showed completed root growth with an intact lamina dura and a defined periodontal space with partial pulp obliteration in the transplanted tooth. The levels of the alveolar ridges were similar to those of the adjacent teeth, and the final crown-to-root ratio was greater than 1:1. The total treatment time was 34 months. After the treatment, a 0.0175-in Twistflex wire (Orthod-Care, Bradford, United Kingdom) was bonded from lateral incisor to lateral incisor in the maxillary arch, and from first premolar to first premolar in the mandibular arch ( Figs 4-7 ). The patient was last examined at age 16 years 7 months, 5 years after the transplantation procedure and 26 months after orthodontic treatment. The response of the transplant to electric pulp testing was positive. The mobility of the teeth was normal, and the sulcus depth was less than 3 mm ( Figs 8-10 ).