Introduction
Autotransplantation has become a major therapeutic option for replacing missing teeth in adult orthodontic patients. However, little systematic information is available about the long-term stability of autotransplanted teeth with complete root formation after the application of an orthodontic force. The objective of this study was to investigate the outcomes of autotransplanted teeth with complete root formation that underwent orthodontic treatment.
Methods
One hundred teeth, autotransplanted in 89 patients, were examined over a mean observation period of 5.8 years. Orthodontic force was applied with nickel-titanium wires 4 to 8 weeks after autotransplantation. Root resorption, ankylosis, mobility, pocket depth, and inflammation at the recipient site were investigated clinically and with radiographs.
Results
The survival rate of the autotransplanted teeth was 93.0%. Abnormal findings were found in 29 teeth, including 7 lost teeth, for a success rate of 71.0%. Donor tooth type and occlusal condition of the donor tooth before transplantation were associated with abnormal findings.
Conclusions
The early application of orthodontic force may increase the success rate of autotransplanted teeth, and the type and presurgical occlusal condition of donor teeth affect the success rate.
Highlights
- •
We investigated the outcomes of autotransplanted teeth with complete root formation.
- •
The survival rate of autotransplanted teeth was 93.0%; the success rate was 71.0%.
- •
Early application of orthodontic force may increase autotransplanted tooth success.
- •
The type and presurgical occlusal condition of donor teeth affect the success rate.
Orthodontic treatment of adolescents and adults with missing teeth is challenging. Treatment options include prosthetic replacements, orthodontic closure, autotransplantation, and maintaining the deciduous teeth in cases of permanent tooth agenesis. However, autotransplantation is now a common tooth replacement procedure, especially in adolescents, in whom implants and other prosthetic replacements are contraindicated for various reasons. A fundamental and definitive difference between autotransplantation and other dental prostheses is that the periodontal ligament (PDL) of autotransplanted teeth is retained as an active interface with surrounding tissues, whereas an artificial substitute is used with other methods.
Teeth are occasionally extracted in orthodontic practice to solve discrepancy problems. Such teeth can be used as donors at the recipient region, and autotransplantation has become a major therapeutic option to replace missing teeth. In contrast to osseointegrated implants, transplanted teeth offer the benefit of functional adaptation and preservation of the alveolar ridge. With successful presurgical and postsurgical procedures, the transplanted tooth usually recovers its proprioceptive function and normal PDL. Consequently, autotransplantation is a useful technique for orthodontists because the transplanted tooth can be moved with orthodontic force.
Considerations when choosing autotransplantation in adult orthodontic treatment include root formation and presurgical condition. Previous studies have reported high survival rates of transplanted teeth with complete root formation. However, little systematic information is available about the long-term stability of autotransplanted teeth with complete root formation with the application of orthodontic force. In addition, it has been reported that hypofunctional teeth (teeth not in intercuspation), such as impacted teeth, are likely to develop ankylosis. In contrast, another study found that the occlusal condition of the donor tooth had no statistically significant effect on the survival rate. Therefore, appropriate transplantation protocols are needed to improve prognosis.
The purpose of this retrospective study of autotransplanted teeth with complete root formation was to evaluate the effects of donor tooth type, donor tooth condition, and early orthodontic treatment on the overall success rate.
Material and methods
We retrospectively reviewed the records of all patients (89 total; 20 male, 69 female) who had autotransplantation of teeth with complete root formation (100 teeth) at our institution from 1995 to 2012. All patients received orthodontic treatment with an edgewise appliance at the Department of Orthodontic Science of Tokyo Medical and Dental University in Japan. The study was approved by the ethical committee of the Faculty of Dentistry of Tokyo Medical and Dental University (approval number: 1022).
Mean patient age at the time of autotransplantation was 29.1 years (males, 28.9 years; range, 18.7-50.8 years; females, 29.2 years; range, 12.3 [with completed root formation]-58.1 years) ( Table I ). The mean follow-up period was 5.8 years (range, 1.9-14.7 years). The donor teeth and the recipient sites are shown in Table II .
| Age group (y) | Male | Female | Total | |||
|---|---|---|---|---|---|---|
| Number of patients | Number of teeth | Number of patients | Number of teeth | Number of patients | Number of teeth | |
| 10-14 | 0 | 0 | 4 | 4 | 4 | 4 |
| 15-19 | 2 | 3 | 8 | 8 | 10 | 11 |
| 20-24 | 3 | 4 | 14 | 19 | 17 | 23 |
| 25-29 | 7 | 7 | 10 | 12 | 17 | 19 |
| 30-34 | 1 | 1 | 14 | 16 | 15 | 17 |
| 35-39 | 4 | 4 | 9 | 9 | 13 | 13 |
| >40 | 3 | 3 | 10 | 10 | 13 | 13 |
| Total | 20 | 22 | 69 | 78 | 89 | 100 |
| Donor teeth | Recipient sites | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incisors (n = 17) | Canine (n = 1) | Premolars (n = 41) | Molars (n = 41) | Total | ||||||||||
| Max central | Max lateral | Mand central | Mand canines | Max first | Max second | Mand first | Mand second | Max first | Max second | Max third | Mand first | Mand second | ||
| Incisors | ||||||||||||||
| Maxillary lateral | 2 (0-1-1) | 2 (0-1-1) | ||||||||||||
| Premolars | ||||||||||||||
| Maxillary first | 1 (0-0-1) | 1 (0-0-0) | 2 (0-0-0) | 14 (1-0-1) | 2 (0-0-0) | 1 (0-0-0) | 2 (1-1-0) | 2 (1-0-0) | 25 (3-1-2) | |||||
| Maxillary second | 2 (0-0-0) | 2 (2-0-0) | 1 (0-0-0) | 3 (0-0-1) | 3 (0-1-0) | 1 (0-0-0) | 12 (2-1-1) | |||||||
| Mandibular first | 6 (0-0-0) | 2 (1-0-0) | 2 (1-0-0) | 10 (2-0-0) | ||||||||||
| Mandibular second | 2 (0-0-0) | 2 (0-0-0) | 1 (0-0-0) | 1 (0-0-0) | 1 (0-0-0) | 7 (0-0-0) | ||||||||
| Molars | ||||||||||||||
| Maxillary second | 5 (1-0-1) | 1 (0-0-0) | 1 (0-0-0) | 1 (1-0-0) | 8 (2-0-1) | |||||||||
| Maxillary third | 1 (0-0-0) | 10 (4-3-1) | 2 (0-0-0) | 1 (0-0-0) | 5 (1-2-1) | 2 (0-0-0) | 21 (5-5-2) | |||||||
| Mandibular second | 1 (0-0-0) | 1 (0-0-0) | 2 (0-0-0) | |||||||||||
| Mandibular third | 1 (0-0-0) | 3 (0-0-0) | 1 (0-0-0) | 6 (1-2-0) | 11 (1-2-0) | |||||||||
| Supernumerary teeth | 1 (0-0-0) | 1 (0-0-0) | 2 (0-0-0) | |||||||||||
| Total | 9 (0-0-1) | 7 (1-1-1) | 1 (0-0-0) | 1 (0-0-0) | 0 | 4 (2-0-0) | 3 (0-0-0) | 34 (6-3-4) | 6 (0-0-0) | 6 (0-0-0) | 1 (0-0-0) | 19 (3-6-1) | 9 (3-0-0) | 100 (15-10-7) |
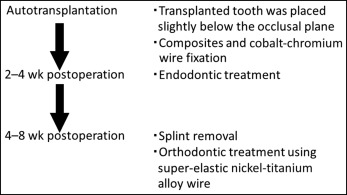
All transplantations were performed by experienced oral and maxillofacial surgeons according to the procedure described below ( Fig 1 ). To prevent excessive occlusal stimuli, the donor teeth were seated carefully into the socket without occlusal contact and splinted to adjacent teeth. Postoperative fixation was carried out with composites and cobalt-chromium wires. Two weeks after transplantation, endodontic treatment was performed with pulp extirpation and calcium hydroxide dressing, before root filling with gutta-percha and a sealer. Four to 8 weeks after transplantation, the splinting was removed, and alignment of the transplanted teeth began. Orthodontic treatment was carried out with 0.018 × 0.025-in slot preadjusted edgewise appliances; 0.016 × 0.022-in superelastic nickel-titanium alloy wires were used for the alignment.
Each transplanted tooth was clinically and radiographically assessed by the same examiner (Z.K. or S.K.). As part of the standard protocol, the following baseline information was retrieved from the medical records and dental casts before transplantation: date of transplantation, donor tooth type, the presence of donor tooth occlusal contacts, and the cause of tooth loss, if applicable. We divided the recipient sites into 3 groups according to the reason for transplantation: prolonged retention of deciduous tooth, missing tooth (including congenitally missing teeth), and permanent tooth with a poor prognosis.
The criteria for “success” were adapted from the studies of Czochrowska et al and Kallu et al. We defined a “successfully transplanted tooth” as one that met the following criteria: (1) normal soft periodontal tissues; (2) no progressive root resorption; (3) no ankylosis (ankylosis was defined as absence of radiolucency between donor tooth root and alveolar bone, high metallic sound of percussion test, and no physiologic mobility); (4) physiologic mobility; (5) no apical infection; and (6) a crown-to-root ratio less than 1, necessary to maintain tooth function (root length greater than half of tooth length). Teeth not fulfilling all criteria were classified as “tentative.” Teeth that were lost or extracted were designated as failures. Tentative and successful teeth were classified as “surviving.”
The total “success rate” was the number of teeth that met the aforementioned conditions, relative to the total number of transplanted teeth. The “survival rate” was the percentage of transplanted teeth still present and functioning well at the time of examination.
Clinical examination included assessments of tooth mobility, palpation, color, inflammation, percussion, probing pocket depth, gingivitis index, and occlusal contacts, according to the method of Denys et al. Tooth mobility was scored on a scale from 0 to 3 (0, no mobility, ankylosis; 1, normal mobility; 2, horizontal mobility; and 3, tooth could be intruded). Pocket probing was performed with a calibrated periodontal probe (CPITN-C; YDM, Tokyo, Japan) at 6 sites on the transplanted tooth: mesiovestibular, vestibular, distovestibular, distolingual, lingual, and mesiolingual regions. Pocket depth exceeding 3 mm was considered pathologic. The sulcus bleeding index proposed by Mühlemann and Son was used to assess gingivitis.
On radiological evaluation, ankylosis was defined as the disappearance of the periodontal space and root resorption without radiolucency relative to the resorption area. Root resorption was defined as resorption cavities on the root surface associated with similar resorption activity in the adjacent alveolar bone. Furcation lesions and periapical lesions were recorded as abnormal findings.
Statistical analysis
Statistical analyses of associations between observed variables (sex, age, donor tooth type, donor tooth condition, recipient site, and recipient site condition) and clinical and radiologic parameters (ankylosis, resorption, mobility, pocket depth, and inflammation) were performed with the Fisher exact test of independence ( P values <0.05 were considered significant). The cumulative survival rate was calculated with the Kaplan-Meier method. All analyses were performed with SPSS statistical software for Windows (version 13.0J; SPSS, Chicago, Ill).
Results
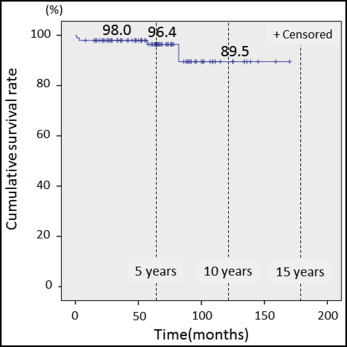
The survival rate of the 100 teeth transplanted in 89 patients was 93.0%; 7 teeth in 6 patients fell out. Of the 93 surviving teeth, 15 developed ankylosis, and 10 had root resorption (3 had both ankylosis and root resorption). The success rate was thus 71.0% because 29 autotransplanted teeth had abnormal findings, including the 7 that fell out ( Table III ). The cumulative survival rates when donor teeth had complete root formation were 96.4% at the 5-year mark and 89.5% at 10 years, as calculated with the Kaplan-Meier method ( Fig 2 ). According to donor tooth type, the survival and success rates were 75.0% (3 of 4) and 50.0% (2 of 4) for incisors, 94.4% (51 of 54) and 77.8% (42 of 54) for premolars, and 92.9% (39 of 42) and 64.3% (27 of 42) for molars at 5 and 10 years, respectively ( Table IV ). The donor teeth had occlusal contacts in 61 of the 93 surviving teeth.
| Male | Female | Total | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Surviving | ||||||
| Success | 16 | 72.8 | 55 | 70.5 | 71 | 71 |
| Ankylosis | 2 | 9.1 | 10 | 12.8 | 12 | 12 |
| Root resorption | 2 | 9.1 | 5 | 6.4 | 7 | 7 |
| Ankylosis + root resorption | 1 | 4.5 | 2 | 2.6 | 3 | 3 |
| Subtotal | 21 | 95.5 | 72 | 92.3 | 93 | 93 |
| Fell out | ||||||
| Ankylosis + root resorption | 0 | 0 | 2 | 2.6 | 2 | 2 |
| Ankylosis + root fracture | 0 | 0 | 2 | 2.6 | 2 | 2 |
| Attachment loss | 1 | 4.5 | 1 | 1.3 | 2 | 2 |
| Attachment loss + root resorption | 0 | 0 | 1 | 1.3 | 1 | 1 |
| Subtotal | 1 | 4.5 | 6 | 7.7 | 7 | 7 |
| Total | 22 | 100 | 78 | 100 | 100 | 100 |
| n | Ankylosis | Resorption | Mobility | Pocket depth | Inflammation | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surviving | Fell out | (+) | (−) | (+) | (−) | (+) | (−) | (+) | (−) | (+) | (−) | |
| Donor tooth type | ||||||||||||
| Incisors | 3 | 1 | 0 | 3 | 1 | 2 | 0 | 3 | 0 | 3 | 0 | 3 |
| Premolars | 51 | 3 | 7 | 44 | 2 | 49 | 2 | 49 | 5 | 46 | 3 | 48 |
| Molars | 39 | 3 | 8 | 31 | 7 | 32 | 4 | 35 | 8 | 31 | 4 | 35 |
| Donor tooth condition | ||||||||||||
| Occlusal contact (+) | 61 | 4 | 9 | 52 | 4 | 57 | 4 | 57 | 10 | 51 | 3 | 58 |
| Occlusal contact (–) | 32 | 3 | 6 | 26 | 6 | 26 | 2 | 30 | 3 | 29 | 4 | 28 |
| Recipient teeth site | ||||||||||||
| Incisors | 15 | 2 | 1 | 14 | 1 | 14 | 0 | 15 | 1 | 14 | 0 | 15 |
| Canines | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 |
| Premolars | 37 | 4 | 8 | 29 | 3 | 34 | 1 | 36 | 2 | 35 | 2 | 35 |
| Molars | 40 | 1 | 6 | 34 | 6 | 34 | 5 | 35 | 10 | 30 | 5 | 35 |
| Recipient site condition | ||||||||||||
| Prolonged retention of deciduous tooth | 24 | 3 | 4 | 20 | 3 | 21 | 1 | 23 | 4 | 20 | 2 | 22 |
| Missing tooth | 49 | 0 | 10 | 39 | 3 | 46 | 1 | 48 | 5 | 44 | 3 | 46 |
| Tooth with poor prognosis | 20 | 4 | 1 | 19 | 4 | 16 | 4 | 16 | 4 | 16 | 2 | 18 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


