Introduction
The purpose of this retrospective cohort study was to assess the effects and efficiency of self-ligating brackets compared with conventional brackets. A secondary purpose was to identify the pretreatment factors associated with the choice of self-ligating or conventional brackets.
Methods
The subjects were treated by 2 private practitioners who used both self-ligating and conventional brackets in their practices. The self-ligating subjects were consecutively identified (treatment completed between January 2011 and April 2012), and then an age- and sex-matched control group was chosen from the same office. The outcome measures were changes in arch dimensions, changes in mandibular incisor inclinations, final peer assessment rating (PAR) scores, percentages of PAR reduction, overall treatment times, total number of visits, and number of emergency visits. All cast and cephalometric measurements were performed on digital records in a blinded manner. Two calibrated assessors measured the PAR scores.
Results
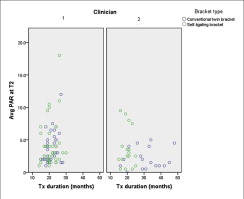
The final sample comprised 74 patients from clinician 1 and 34 patients from clinician 2. The practitioners had significant differences for several treatment parameters; therefore, the data from the 2 clinicians were analyzed separately. For clinician 1, no significant differences were observed between the self-ligating and conventional groups, other than increased arch length in the self-ligating group. The self-ligation patients treated by clinician 2 demonstrated significant increases in transverse dimensions, lower percentages of reduction in PAR scores, shorter treatment times, fewer visits, and more wire-sliding emergencies than the conventional bracket group.
Conclusions
Although some significant findings were observed, the small sample and the lack of consistent findings between the 2 clinicians made it difficult to draw strong conclusions.
Graphical abstract
Highlights
- •
We compared self-ligating and conventional brackets retrospectively.
- •
Parameters were arch dimension, incisor inclination, and occlusal outcome.
- •
Measurements were made at 2 times for 2 clinicians
- •
Bracket type did not affect the measurements or treatment efficiency.
- •
Variations depend more on patient characteristics or treatment choices.
Since the advent of self-ligating brackets, there have been assertions that they are more efficient and effective in treating malocclusions than conventional brackets. For example, it was asserted that low friction allows for sliding mechanics to be accomplished in the truest sense, thereby facilitating alignment, increasing appointment intervals, and reducing the overall treatment time. However, the evidence regarding the amount of friction with self-ligating brackets is limited. A systematic review that included 19 in-vitro studies concluded that self-ligating brackets produced less friction with small round archwires without tipping and malalignment. However, there was little evidence to claim an advantage with large rectangular wires.
Also, with less friction, the idea that less force is needed to move teeth has led to the presumption that self-ligating brackets produce more physiologic tooth movement by not interrupting the periodontal blood supply. Therefore, more alveolar bone generation, greater amounts of lateral expansion, less proclination of anterior teeth, and less need for extractions are claimed to be possible with self-ligating brackets. A meta-analysis investigating arch dimensions showed no significant differences between self-ligating and conventional brackets for intercanine and intermolar widths. Nevertheless, a few studies have suggested greater increases in intermolar widths with self-ligating brackets. Also, the evidence for incisor proclination from a recent meta-analysis indicated that self-ligating brackets resulted in slightly less mandibular incisor proclination (1.5°). Thus, evidence on the effects and advantages of self-ligation appears to be mixed, and additional well-conducted studies are needed to evaluate the various claims made by the proponents of self-ligation.
Clinical studies evaluating total treatment time have also shown mixed results. Some retrospective studies found significantly decreased total treatment times and fewer visits with self-ligating brackets. However, a large retrospective study and most prospective studies have found no measurable advantages in orthodontic treatment time, number of treatment visits, and time spent in initial alignment with self-ligating brackets over conventional brackets. A recent meta-analysis pooled the data from 3 retrospective studies and found no difference in terms of reduced overall treatment time. These systematic reviews indicated a lack of sufficient evidence to show that orthodontic treatment is more or less efficient with self-ligating brackets. An identical result was obtained for occlusal quality outcome in the meta-analysis of these 3 retrospective studies. These studies used different indexes to assess the quality of the occlusal finish. Thus, the interpretation of their results was not conclusive because of the heterogeneity of the measured outcomes. Other studies that compared percentages of reduction in peer assessment rating (PAR) scores found no significant differences between self-ligating and conventional brackets. Studies comparing the failure rates between self-ligating and conventional brackets have also shown conflicting results. Pandis et al found no significant differences between the 2 systems. However, other studies have shown more emergencies associated with self-ligating brackets. The meta-analysis mentioned above found no significant differences.
The purpose of this retrospective cohort study was to assess the effects and efficiency of self-ligating brackets compared with conventional brackets. A secondary purpose was to identify any pretreatment malocclusion characteristics associated with the choice of self-ligating or conventional brackets.
Material and methods
This retrospective cohort study was approved by the institutional review board at the University of Washington. The subjects were obtained from the private practices of 2 clinicians, who are faculty members in the University of Washington’s Department of Orthodontics. These practitioners were chosen to participate in this study because they had been treating approximately equal numbers of patients in their practices with conventional and self-ligating systems for the past few years. The self-ligation group (Damon Q; Ormco, Orange, Calif; used by both clinicians) included consecutively treated patients from both offices. The self-ligating subjects were selected first, and for each subject, an age- and sex-matched control subject (Mini Uni-twin; 3M Unitek, Monrovia, Calif; used by clinician 1; and Victory series; 3M Unitek; used by clinician 2) was chosen from the same office. All bracket systems had 0.022-in slots. The study included adolescents and young adults (11-25 years old) who had completed comprehensive fixed appliance therapy between January 1, 2011, and April 30, 2012. Patients who had previously received interceptive treatment or extractions were included. Any patients with craniofacial anomalies, surgical treatment, treatment with arch expansion with expanders, interdisciplinary treatment, and incomplete records were excluded.
Initial (T1) and final (T2) records consisting of digital or plaster study models, lateral cephalometric radiographs, and treatment notes were obtained from both offices. All patient identifiable information was replaced by random study identification numbers. The digital study models from 1 office were exported from OrthoCAD (version 3.5; Cadent, Carlstadt, NJ) to Ortho Insight 3D software (Motion View, Hixson, Tenn). Plaster models from the other practice were scanned using the Ortho Insight 3D scanner (Motion View). All digital or scanned lateral cephalometric radiographs were imported to Dolphin software (Dolphin Imaging & Management Solutions, Chatsworth, Calif).
Arch dimensions and irregularity index as measures of crowding, overjet, and Angle molar classification were measured on digital models by the primary investigator (M.A.). The PAR was also used on the digital models by the primary investigator and a second assessor (K.S.J.) independently, and the scores were averaged. Both examiners were calibrated for the PAR index before performing the measurements for the study. The contact displacement component of the PAR score was measured using a millimeter ruler with the digital models positioned in the occlusal view. The buccal occlusion assessment was accomplished by positioning the study casts in the right or left buccal position without moving them. Overjet, overbite, and centerline were measured using a linear measurement tool available with the digital software, being careful to measure in the appropriate plane of space. The primary investigator traced all cephalograms on the Dolphin software to measure the mandibular incisor inclination. Treatment notes from digital charts were reviewed in the offices of the orthodontists by the primary investigator to determine treatment time, total number of visits during treatment, emergency visits, and reasons for the emergencies. All data measurements on digital models and radiographs were performed in a blinded manner. Data abstraction from digital treatment charts could not be blinded because the appliance system appeared on every page of the treatment notes.
The following outcomes were measured for T1 and T2.
- 1.
Arch dimensions: intercanine width, the distance between the tips of the mandibular and maxillary canines; intermolar width, the distance between the central grooves of the mandibular and maxillary first molars; and arch length, the sum of the distances of the 2 lines from the mesial surface of each first molar to the contact point between the central incisors.
- 2.
Mandibular incisor inclination: the angle between the long axis of the most prominent mandibular incisor and the line passing through gonion and menton (mandibular plane).
- 3.
Final PAR score and percentage of reduction in PAR scores: measured according to the PAR index. The percentage of PAR reduction was calculated as follows:
- 4.
Total treatment time: calculated in months from the placement of the fixed appliances to their removal.
- 5.
Number of visits during treatment, excluding emergencies.
- 6.
Emergency rate: number of emergency visits with reasons, including sliding or poking wire, broken brackets, loss of ligation from a broken door, or a loose elastomeric tie.
- 7.
Pretreatment crowding: assessed by measuring Little’s incisor irregularity index in the mandibular arch.
- 8.
Overjet: distance from the incisal edge of the maxillary incisors to the labial surface of mandibular incisors.
- 9.
Angle molar classification.
- 10.
Extractions.
Measurement error was assessed by randomly selecting 10 study casts and lateral cephalometric radiographs. The radiographs were retraced with the Dolphin software to determine the mandibular incisor inclination in relation to the mandibular plane, and the digital models were remeasured for intermolar width, intercanine width, arch length, and Little’s incisor irregularity index. These measurements were made 2 weeks apart. Dahlberg’s formula ( s = ∑ d 2 / 2 n , where d is the difference between the first and second measurements) was used to evaluate the magnitude of the error for each variable. Additionally, the PAR scores were managed according to a predetermined protocol. If the examiners’ independent measurements for the PAR score were 5 points or fewer apart, the mean score was used. If the scores differed by more than 5 points, the casts were rescored independently, and the mean was used if the new scores were 5 points or fewer apart. If the scores were still more than 5 points apart, the 2 examiners measured the models together, coming to a consensus score.
A priori power analyses based on 80% power were conducted using the power and sample size online calculator of Lenth. For 80% power, a clinically significant mean difference of 3 months was hypothesized, and a standard deviation of 5.2 months was estimated for treatment duration to achieve the required sample size. Other variables such as intercanine width and mandibular incisor proclination were also assessed for sample size calculation. However, all of these variables required fewer subjects. Hence, it was determined that a sample size of 47 patients in each group was needed. The level of statistical significance was set at 0.05.
Statistical analysis
The data were entered into an Excel spreadsheet (Microsoft for Mac, 2008 version; Microsoft, Redmond, Wash) and then imported into SPSS software (version 19; IBM, Armonk, NY) for statistical analysis. Descriptive statistics for both bracket groups were calculated for all variables. Independent t tests or chi-square or Fisher exact tests were performed for all variables to assess the differences between self-ligating and conventional brackets without adjusting for effect modifiers or confounders. General linear regression models were created to assess the differences between the bracket types for final mandibular incisor inclinations, final PAR scores, percentages of reduction in PAR scores, treatment durations, and total numbers of visits after adjusting for potential confounding variables such as initial incisor inclination, low-torque brackets, Angle classification, initial PAR score, and SureSmile (Orametrix, Richardson, Tex) treatment. Independent sample t tests were used to determine whether any pretreatment malocclusion traits such as crowding, initial overjet, Angle molar classification, initial mandibular incisor inclination, or extractions were associated with the choice of self-ligating or conventional brackets. Analyses were performed separately for each clinician. To account for the fact that 2 tests were done for each hypothesis, all P values and confidence intervals were adjusted with the method of Šídák.
Results
The magnitudes of the errors were small: from 0.25 to 0.66 mm for the linear measurements, and 1.84° for mandibular incisor inclination. The PAR scores between the 2 assessors were different by more than 5 points in 37 of the 216 sets of study casts (17%). After each of these 37 casts was independently rescored, the scores of only 15 sets of casts were still different by more than 5 points. These remaining casts were scored by consensus.
A total of 122 subjects from both offices (84 from clinician 1 and 38 from clinician 2) were selected. However, on initial inspection of the patient characteristics, it was noted that both practitioners treated only about 5% of their patients with extractions. Because extractions can be quite influential on treatment time, we decided to remove all pairs of patients in which either subject had undergone extractions. The final sample comprised 74 patients from clinician 1 and 34 patients from clinician 2. Although the characteristics of the subjects within and between the offices were relatively similar, the 2 clinicians exhibited significant differences in several treatment parameters, such as use of interproximal reduction, the SureSmile technique, and the rate of prior phase 1 orthodontic treatment. Therefore, the decision was made to analyze the data from the 2 offices separately.
Pretreatment demographics were similar for the self-ligating and conventional bracket groups because the samples were matched for age and sex. The mean age for clinician 1’s sample was 13.5 years for both groups. Clinician 2’s sample was also comparable, with mean ages of 13.8 and 13.7 years for the self-ligating and conventional groups, respectively. For clinician 1, the initial PAR scores differed between patients selected for the 2 bracket types, but the self-ligating and conventional samples from clinician 2 were not significantly different for all clinical factors ( Table I ). Table II demonstrates some differences in treatment strategies between the 2 practitioners.
| Clinician 1 | Clinician 2 | |||
|---|---|---|---|---|
| Self-ligating brackets (n = 37) | Conventional brackets (n = 37) | Self-ligating brackets (n = 17) | Conventional brackets (n = 17) | |
| Malocclusion, n (%) | ||||
| Class I | 12 (32.4) | 13 (35.1) | 9 (52.9) | 6 (35.3) |
| Class II | 19 (51.4) | 23 (62.2) | 8 (47.1) | 11 (64.7) |
| Class III | 6 (16.2) | 1 (2.7) | 0 (0) | 0 (0) |
| Crowding (mm), mean (SD) | 5.6 (3.6) | 4.5 (3.1) | 4.9 (2.9) | 4.6 (3.3) |
| Overjet (mm), mean (SD) | 3.1 (2.1) | 3.6 (1.5) | 3.2 (1.6) | 4.3 (2.4) |
| Mandibular arch dimensions (mm), mean (SD) | ||||
| Intercanine width | 25.9 (2.2) | 25.7 (1.7) | 26.5 (2.7) | 26.2 (2.3) |
| Intermolar width | 41.9 (3.1) | 41.6 (2.2) | 41.5 (2.2) | 41.8 (3.0) |
| Arch length | 59.6 (4.0) | 60.6 (3.3) | 62.6 (4.0) | 60.3 (4.5) |
| Maxillary arch dimensions (mm), mean (SD) | ||||
| Intercanine width | 34.2 (3.1) | 34.7 (1.9) | 35.1 (2.4) | 34.4 (1.8) |
| Intermolar width | 46.3 (3.4) | 47.3 (2.5) | 46.8 (2.0) | 46.4 (2.9) |
| Arch length | 69.2 (4.6) | 70.6 (3.8) | 72.2 (4.5) | 69.7 (4.0) |
| Mandibular incisor inclination (°), mean (SD) | 90.8 (6.8) | 94.4 (6.9) | 95.2 (4.7) | 92.7 (5.0) |
| PAR score, mean (SD) | 24.0 (10.9) | 17.4 (7.7) ∗ | 15.6 (9.7) | 20.4 (9.3) |
| Clinician 1 | Clinician 2 | |||
|---|---|---|---|---|
| Self-ligating brackets (n = 17) | Conventional brackets (n = 37) |
Self-ligating brackets (n = 17) |
Conventional brackets (n = 17) |
|
| IPR | 3 (8.1) | 2 (5.4) | 4 (23.5) | 4 (23.5) |
| SureSmile | 9 (24.3) | 1 (2.7) ∗ | 0 (0) | 0 (0) |
| Phase 1 treatment | 18 (48.6) | 21 (56.8) | 3 (17.6) | 4 (23.5) |
| Low-torque brackets | 6 (16.2) | 0 (0) ∗ | 0 (0) | 0 (0) |
The arch dimensions in the self-ligation patients had a greater increase in arch length (about 2 mm for both arches) for clinician 1’s sample ( Table III ). Clinician 2’s self-ligation sample showed greater changes in mandibular intermolar width.
| Outcome | Clinician 1 | Clinician 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Self-ligating brackets (n = 37) Mean (SD) |
Conventional brackets (n = 37) Mean (SD) |
Difference (95% CI) |
Adjusted (95% CI) |
Self-ligating brackets (n = 17) Mean (SD) |
Conventional brackets (n = 17) Mean (SD) |
Difference (95% CI) |
Adjusted (95% CI) |
|
| Mandibular intercanine width (mm) | 1.1 (1.9) | 1.0 (1.5) | 0.1 (−0.9 to 1.0) | 1.4 (1.4) | 0.2 (1.7) | 1.2 (0.0 to 2.5) | ||
| Mandibular intermolar width (mm) | 0.8 (2.3) | 0.6 (1.7) | 0.2 (−0.9 to 1.3) | 2.2 (1.4) | 0.5 (1.6) | 1.6 (0.4 to 2.8)* | ||
| Mandibular arch length (mm) | 2.3 (3.2) | 0.5 (2.3) | 1.8 (0.3 to 3.3)* | −0.2 (2.5) | 0.9 (3.8) | −1.1 (−3.8 to 1.5) | ||
| Maxillary intercanine width (mm) | 0.7 (3.0) | −0.3 (1.9) | 1.0 (−0.5 to 2.4) | 1.5 (3.4) | −0.8 (1.5) | 2.3 (0.0 to 4.5) | ||
| Maxillary intermolar width (mm) | 0.6 (2.1) | 0.3 (1.9) | 0.3 (−0.7 to 1.4) | 0.3 (3.2) | 0.7 (1.8) | −0.4 (−2.5 to 1.7) | ||
| Maxillary arch length (mm) | 2.0 (3.7) | 0.0 (2.6) | 2.0 (0.3 to 3.7)* | −0.5 (3.1) | 0.3 (4.0) | −0.8 (−3.4 to 1.7) | ||
| Mandibular incisor inclination (°) | 5.6 (6.3) | 4.9 (5.2) | 0.7 (−2.3 to 3.8) | 0.9 (−2.5 to 4.2)† | 1.5 (4.3) | 6.0 (7.4) | −4.5 (−9.5 to 0.6) | −3.0 (−7.4 to 1.4)‡ |
| Final PAR score | 4.2 (3.6) | 3.7 (2.4) | 0.5 (−1.1 to 2.1) | 0.4 (−1.3 to 2.1)§ | 3.6 (3.0) | 2.1 (1.6) | 1.5 (−0.4 to 3.4) | 1.6 (−0.4 to 3.7)§ |
| Percentage of PAR reduction | 74.3 (35.8) | 72.2 (26.2) | 2.2 (−14.5 to 18.8) | −9.8 (−24.8 to 5.3)§ | 70.3 (30.0) | 89.0 (7.9) | −18.7 (−36.4 to −1.0)* | −15.7 (−33.5 to 2.2)§ |
| Treatment duration (mo) | 20.7 (3.9) | 21.3 (3.2) | −0.6 (−2.5 to 1.3) | −0.3 (−2.3 to 1.7)‖ | 19.9 (3.1) | 31.2 (9.3) | −11.2 (−17.0 to −5.5)* | −10.8 (−16.7 to −5.0)§* |
| Total visits (n) | 14.8 (3.0) | 15.6 (2.4) | −0.8 (−2.3 to 0.6) | −0.4 (−2.0 to 1.1)‖ | 13.8 (2.0) | 21.2 (6.8) | −7.4 (−11.6 to −3.3)* | −7.0 (−11.1 to −2.8)§* |
| Emergency visits (n) | 2.3 (1.8) | 2.0 (2.3) | 0.3 (−0.6 to 1.3) | 3.1 (1.7) | 2.2 (2.7) | 0.8 (−0.8 to 2.4) | ||
| Broken brackets (n) | 1.2 (1.4) | 1.2 (1.7) | 0.0 (−0.8 to 0.7) | 1.9 (1.8) | 2.4 (3.6) | −0.5 (−2.5 to 1.5) | ||
| Wire-sliding events (n) | 18 (48.6) | 17 (45.9) | 2.7 | 12 (70.6) | 2 (11.8) | 58.8* | ||
| Loss of ligation (n) | 8 (21.6) | 3 (8.1) | 13.5 | 1 (5.9) | 1 (5.9) | 0 | ||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


