Introduction
The purposes of this study were to evaluate and compare the periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion devices using cone-beam computed tomography.
Methods
Twenty-five patients requiring maxillary expansion were randomly allocated into 2 groups. A tooth-borne hyrax appliance was used in the first group, consisting of 13 patients (8 girls, 5 boys; mean age, 14.3 ± 2.3 years), and a tooth-bone-borne hybrid hyrax appliance was used in the second group of 12 patients (6 girls, 6 boys; mean age, 13.8 ± 2.2 years). Cone-beam computed tomography records were taken before and 3 months after expansion, and periodontal, dentoalveolar, and skeletal measurements were made on the cone-beam computed tomography images with a software program. The 2 independent-samples t test and the Mann-Whitney U test were used to evaluate treatment changes for both groups. Paired-samples t test and Wilcoxon test were used to compare the measurements at 2 time points for variables.
Results
Significant skeletal changes and increases in interdental distances were observed in both groups. However, the distances between the first and second premolars increased more with the hyrax appliance (7.5 ± 4.2 and 7.9 ± 3.3 mm, respectively) than with the hybrid hyrax (3.2 ± 2.6 and 4.5 ± 3.8 mm, respectively) ( P <0.05). Similar reductions in buccal bone plate thickness and increases in palatal bone plate thickness of the anchored teeth occurred in both groups, whereas changes in buccal and palatal bone thicknesses of the left first premolars significantly differed between groups ( P <0.001). No significant intergroup difference was found in terms of absolute dental tipping.
Conclusions
Both tooth-borne and tooth-bone-borne rapid expansion are effective methods for treating a narrow maxilla. However, the hyrax appliance resulted in greater expansion in the premolar region. On the other hand, the hybrid hyrax appliance did not cause changes in the bony support of the first premolars.
Highlights
- •
The effects of tooth-borne and tooth-bone-borne expansion appliances were evaluated.
- •
Both tooth-borne and tooth-bone-borne rapid expansion are effective methods.
- •
The hyrax appliance results in greater expansion in the premolar region.
- •
Both appliances reduce the buccal bone thickness.
- •
The hybrid hyrax causes no periodontal changes for the first premolars.
Transverse maxillary deficiency is a common orthodontic problem often seen in children. Early treatment with different protocols and various appliances is recommended to correct maxillary constrictions. One common method, rapid maxillary expansion (RME), described by Angell, has been used for more than 150 years as a part of orthodontic treatment.
The purposes of RME are to produce hyalinization in the periodontal ligament of the anchor teeth using heavy forces and to achieve maximum orthopedic and minimum orthodontic effects with the opening of the midpalatal suture. Traditional tooth-borne RME devices are supported by the maxillary first premolars and first molars with bands or by the posterior teeth with acrylic. However, with tooth-supported expansion devices, it is not possible to obtain pure skeletal opening. Moreover, excessive buccal tipping of the posterior teeth, root resorption, gingival recession, buccal cortical bone thinning, and fenestration have been reported as undesirable effects. Recent computed tomography (CT) studies have demonstrated decreases in buccal alveolar bone thicknesses of the supporting teeth after RME. Garib et al reported that the greatest bone dehiscences among the banded teeth were found at the first premolars. To overcome these disadvantages of tooth-borne expansion, the use of bone anchored RME appliances (transpalatal distractors) was proposed. On the other hand, the application and removal of transpalatal distractors to the palatal bone require an invasive surgical procedure and increase the risk of infections.
A recently developed tooth-bone-borne appliance may be another option for RME. This hybrid hyrax device, anchored to the first molars at the posterior and to the palate at the anterior with miniscrews, provides several advantages such as eliminating the need for invasive surgery, being more cost-effective, and reducing buccal tipping. Furthermore, it can be used in patients with inadequate anterior dental anchorage (missing deciduous teeth or premolars with underdeveloped roots). A clinical study evaluating the effects of the hybrid hyrax combined with a facemask on 3-dimensional (3D) scans of dental models and also a finite element analysis showed its effectiveness for RME. However, there is lack of information on its periodontal and skeletal effects in the current literature.
Lateral cephalometric, posteroanterior, and occlusal radiographs and dental casts have been used to diagnose transverse anomalies and evaluate changes in dentofacial structures after RME. Factors including loss of data during the reduction of 3D objects into 2-dimensional (2D) images, superimposition of anatomic structures on radiographs, and internal and external orientation mistakes that influence the analysis of results render 2D radiologic methods inadequate in assessing the skeletal, dental, and periodontal effects of treatments. Three-dimensional volumetric imaging with cone-beam CT (CBCT) not only overcomes these limitations but also enables quantitative evaluation of alveolar bone thicknesses.
The aims of this study were to evaluate and compare the periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion methods with CBCT.
Material and methods
This prospective clinical study was carried out on patients who required maxillary expansion. The selection criteria were (1) unilateral or bilateral posterior crossbite and maxillary constriction; (2) no previous orthodontic treatment; (3) permanent dentition with no congenitally missing or extracted maxillary canines, premolars, and first molars; and (4) no systemic or genetic disease.
This study was approved by the institutional review board of Yeditepe University, Istanbul, Turkey (decision number 178). Informed consent was obtained from the parents.
Of 51 maxillary constriction patients referred to the orthodontic clinic at Yeditepe University during a 2-year period, 26 patients meeting the criteria and agreeing to participate were consecutively enrolled in the study. According to the order of referral with a randomization ratio of 1:1, they were randomly allocated to 2 groups by an orthodontist (D.G.-C.) who did not know in advance which treatment the next patient would get. One patient who lost the palatal miniscrews 2 days after insertion of the expander because of consuming hard foods was excluded from the study.
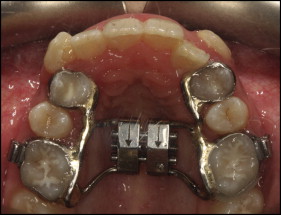
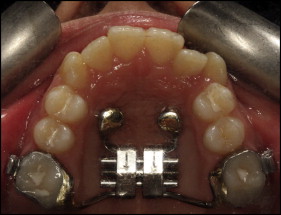
The mean ages and sex distributions of the groups are shown in Table I . The patients in the first group (8 girls, 5 boys; mean age, 14.3 ± 2.3 years) were treated with a traditional tooth-supported hyrax appliance attached to the maxillary first premolars and molars ( Fig 1 ). The patients in the second group (6 girls, 6 boys; mean age, 13.8 ± 2.2 years) were treated with a tooth-bone supported hybrid hyrax appliance ( Fig 2 ). Molar bands were fitted to the maxillary right and left first molars. Two miniscrews (Total Anchor; Trimed, Ankara, Turkey) with a 1.8-mm diameter and a 9-mm length were inserted using a physiodispenser after predrilling with a 1-mm drill at the level of the right and left first premolars, near the second and third palatal rugae, next to the midpalatal suture, under local anesthetic by the same operator (M.T.). Transfer caps were placed over the miniscrews, and a silicone impression was taken. After the laboratory analogs were inserted into the transfer caps, the model was obtained, and the hybrid hyrax was fabricated. The appliance was applied 7 days after placement of the miniscrews and bonded to the first molars by the bands and to the miniscrews by the caps (TTA S-cap; Trimed) using glass ionomer cement (Multi-Cure glass ionomer band cement; 3M Unitek, Monrovia, Calif). In both groups, the expansion screw was activated twice a day (a quarter turn in the morning and another quarter turn in the evening). In both groups, all patients showed a midpalatal suture split that was clinically detected. When the palatal cusp tips of the maxillary first molars were in contact with the corresponding buccal cusp tips of the mandibular first molars, expansion was completed. Then the screw was fixed with a ligature wire, and the expansion device was left in place for 3 months of the retention period. At the end of 3 months, the expansion device was removed and a transpalatal arch was placed.
| Hyrax | Hybrid hyrax | P | |
|---|---|---|---|
| Age (y) | 14.3 ± 2.3 | 13.8 ± 2.2 | 0.6 ∗ |
| Activation time (d) | 19.2 ± 4.5 | 20.2 ± 3.0 | 0.5 ∗ |
| Sex | 0.6 † | ||
| Male | 5 (38.5) | 6 (50) | |
| Female | 8 (61.5) | 6 (50) | |
CBCT records were collected before treatment (T1) and at the end of the 3 months of retention (T2), after removal of the expansion appliance. CBCT scans were taken with an Iluma device (IMTEC [3M], Ardmore, Okla) at these settings: 3.8 mA, 120 kV, exposure time of 40 seconds, voxel size of 0.2 mm, axial slice thickness of 0.3 mm, and scanning area of 20 × 25 cm. The DICOM images obtained from the patients were processed with the Mimics software program (Materialise, Leuven, Belgium) for the measurements. All measurements were made by the same researcher (M.G.T.). Blinding was used at the analysis level.
The Frankfort horizontal (FH) plane was constructed using the right and left orbitale, the right meatus acusticus externus, and the midsagittal plane with anterior nasal spine, nasion, and basion. CBCT images taken at T1 and T2 were oriented with the FH plane parallel to the floor and the midsagittal plane perpendicular to the FH plane to standardize the head position. All 2D images were resliced according to the FH plane.
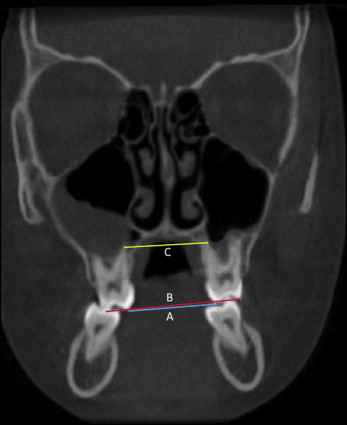
Measurements of bone plate thicknesses of the maxillary posterior teeth at the buccal and palatal aspects were made on the axial sections at the levels of the maxillary right first molar furcation for the right posterior teeth and the maxillary left first molar furcation for the left posterior teeth ( Table II , Fig 3 ). Palatal maxillary width was also measured on the axial section ( Table II , Fig 3 ).
| Parameter | Description |
|---|---|
| Molar mesiobuccal bone thickness (M1 MBBT) | Distance between the external border of the buccal cortical plate to the center of buccal aspect of first molar mesiobuccal root |
| Molar distobuccal bone thickness (M1 DBBT) | Distance between the external border of the buccal cortical plate to the center of buccal aspect of first molar distobuccal root |
| Molar palatal bone thickness (M1 PBT) | Distance between the external border of the palatal cortical plate to the center of palatal aspect of first molar palatal root |
| Second premolar buccal bone thickness (P2 BBT) | Distance between the external border of the buccal cortical plate to the center of buccal aspect of second premolar root |
| Second premolar palatal bone thickness (P2 PBT) | Distance between the external border of the palatal cortical plate to the center of palatal aspect of second premolar root |
| First premolar buccal bone thickness (P1 BBT) | Distance between the external border of the buccal cortical plate to the center of buccal aspect of first premolar root |
| First premolar palatal bone thickness (P1 PBT) | Distance between the external border of the palatal cortical plate to the center of palatal aspect of first premolar root |
| Canine buccal bone thickness (C BBT) | Distance between the external border of the buccal cortical plate to the center of buccal aspect of canine root |
| Canine palatal bone thickness (C PBT) | Distance between the external border of the palatal cortical plate to the center of palatal aspect of canine root |
| Palatal maxillary width (PMW) | Distance between the right and left lingual cortical plates measured along a line passing through the centers of the furcation of both maxillary first molars |
| Nasal width (NW) | Distance between the convexity of the right and left borders of the piriform |
| Interpterygoid distance (IPD) | Distance between the most lateral inferior points of the right and left lateral pterygoid plates |
| Intermolar buccal cuspal width (M1 BW) | Distance between the mesiobuccal cusp tips of the right and left first molars |
| Intermolar palatal cuspal width (M1 PW) | Distance between the mesiopalatal cusp tips of the right and left first molars |
| Intermolar apical width (M1 AW) | Distance between the palatal apices of the right and left first molars |
| Intersecond premolar buccal cuspal width (P2 BW) | Distance between the buccal cusp tips of the right and left second premolars |
| Intersecond premolar palatal cuspal width (P2 PW) | Distance between the palatal cusp tips of the right and left second premolars |
| Intersecond premolar apical width (P2 AW) | Distance between the apices of the right and left second premolars |
| Interfirst premolar buccal cuspal width (P1 BW) | Distance between the buccal cusp tips of the right and left first premolars |
| Interfirst premolar palatal cuspal width (P1 PW) | Distance between the palatal cusp tips of the right and left first premolars |
| Interfirst premolar apical width (P1 AW) | Distance between the apices of the right and left first premolars |
| Intercanine cuspal width (C CW) | Distance between the cusp tips of the right and left canines |
| Intercanine apical width (C AW) | Distance between the apices of the right and left canines |
| Molar dental inclination (M1 DI) | Angle between the line passing through the molar palatal root apex and palatal cusp and the vertical line parallel to the midsagittal plane |
| Second premolar dental inclination (P2 DI) | Angle between the line passing through the second premolar palatal root apex and palatal cusp and the vertical line parallel to the midsagittal plane |
| First premolar dental inclination (P1 DI) | Angle between the line passing through the first premolar palatal root apex and palatal cusp and the vertical line parallel to the midsagittal plane |
| Canine dental inclination (C DI) | Angle between the line passing through the canine root apex and cusp tip and the vertical line parallel to the midsagittal plane |
| Molar alveolar inclination (M1 AI) | Angle between the tangent to the alveolar bone and the vertical line parallel to the midsagittal plane at the level of first molar |
| First premolar alveolar inclination (P1 AI) | Angle between the tangent to the alveolar bone and the vertical line parallel to the midsagittal plane at the level of first premolar |
| Maxillary width (MW) | Distance between the left and right maxillary bone convexities on the coronal section at the level of right first molar trifurcation |
| Molar absolute dental tipping (M1 ADT) | Difference between the changes in the first molar alveolar inclination and dental inclination |
| First premolar absolute dental tipping (P1 ADT) | Difference between the changes in first premolar alveolar inclination and dental inclination |
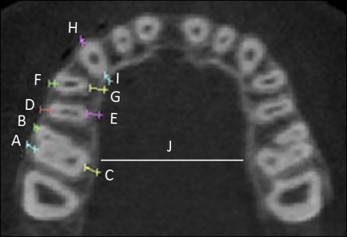
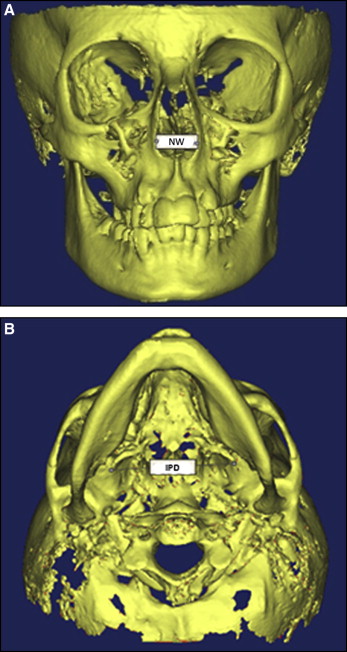
On the 3D images, nasal width and the distance between the lateral pterygoid plates were measured ( Table II , Fig 4 ).
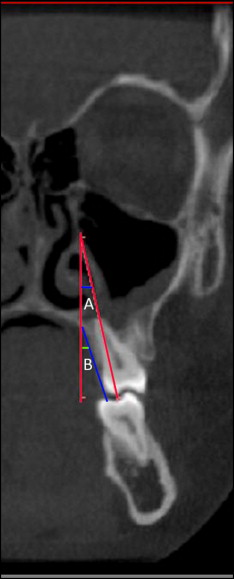
The dental transverse measurements were made on the coronal sections for the canines, first premolars, second premolars, and maxillary first molars. The coronal slices were identified according to the method described by Podesser et al on CT and used by Christie et al on CBCT. For example, the molar slice was defined as the first anterior slice showing the entire palatal root and the crown of the first molar. Premolar and canine slices were chosen as the most anterior slices where the root and the crown of the relevant tooth could be seen in the entire length. Then the distances between the right and left buccal cusp tips, palatal cusp tips, and apices were measured ( Table II , Fig 5 ). Similarly, dental and alveolar inclinations were measured on the coronal sections for right and left canines, first and second premolars, and first molars. Dental inclination was defined as the angle formed by the line passing through the relevant tooth’s palatal root apex and palatal cusp and the vertical line parallel to the midsagittal plane. Alveolar inclination was defined as the angle between the tangent to the alveolar bone and the vertical line parallel to the midsagittal plane on the same coronal section used for dental inclination measurements ( Table II , Fig 6 ). Maxillary width was measured as the distance between the maxillary left and right bone convexities at the level of the nasal base, on the coronal section at the level of right first molar’s trifurcation ( Table II , Fig 7 ).

Statistical analysis
The statistical analyses were performed with the Statistical Package for the Social Sciences (version 21.0; IBM, Armonk, NY). Descriptive statistics, including the means and standard deviations, were obtained for the data. The descriptive statistics are presented as means and standard deviations for the continuous variables or as percentages for the categorical variables. Normal distribution of data was tested using the Kolmogorov-Smirnov test. For normally distributed variables, the 2 independent-samples t test was used to compare the mean differences between the groups. For variables that were not normally distributed, the Mann-Whitney U test was used to compare the mean differences between the 2 independent groups. The Fisher exact test was used to compare the frequency distributions between the groups. For normally distributed variables, the difference between the variables’ before and after levels was analyzed using a paired-samples t test. For variables that were not normally distributed, the difference between the variables’ before and after levels was analyzed with the Wilcoxon test. Significance of the results was evaluated at the level of P <0.05.
Based on the observed effect sizes, experimental statistical power analyses were conducted to determine the power of the study. The sample size was calculated based on the ability to detect 0.6 mm of buccal bone loss of the first premolars after expansion. The expected standard deviation of buccal bone loss was taken from the study of Garib et al, who studied the periodontal effects of RME with tooth-tissue-borne and tooth-borne expanders. The calculation indicated that for a study with a power of 0.90 and an alpha of 0.05, we required a total of 26 patients (13 patients in each group).
One week after the first measurements, they were repeated by the same author (M.G.T.). Intraexaminer reliability values were determined with intraclass correlation coefficients.
Results
Intraclass correlation coefficients were greater than 0.90 for most of the variables and greater than 0.85 for the left second premolar inclinations, the right molar mesiobuccal and distobuccal bone thicknesses, and the left molar distobuccal bone thickness.
No significant differences were observed between the hyrax and hybrid hyrax groups before treatment in terms of age, sex, or periodontal, dentoalveolar, and skeletal measurements except for the right molar, and the right and left canine dental inclinations ( Table III ).
| Hyrax | Hybrid hyrax | P | |
|---|---|---|---|
| Right | |||
| M1 MBBT (mm) | 1.28 ± 0.72 | 1.73 ± 0.66 | 0.12 |
| M1 DBBT (mm) | 1.85 ± 0.84 | 2.20 ± 0.91 | 0.33 |
| M1 PBT (mm) | 1.06 ± 0.88 | 1.62 ± 0.58 | 0.79 |
| P2 BBT (mm) | 1.92 ± 0.75 | 1.83 ± 0.89 | 0.81 |
| P2 PBT (mm) | 2.08 ± 1.39 | 1.74 ± 0.72 | 0.54 |
| P1 BBT (mm) | 1.17 ± 0.64 | 1.01 ± 0.70 | 0.56 |
| P1 PBT (mm) | 1.73 ± 1.05 | 2.51 ± 1.66 | 0.17 |
| C BBT (mm) | 0.21 ± 0.48 | 0.40 ± 0.85 | 0.52 |
| C PBT (mm) | 2.01 ± 1.08 | 2.40 ± 1.46 | 0.47 |
| Left | |||
| M1 MBBT (mm) | 1.23 ± 0.98 | 1.57 ± 1.03 | 0.41 |
| M1 DBBT (mm) | 1.93 ± 1.00 | 2.67 ± 0.80 | 0.55 |
| M1 PBT (mm) | 1.08 ± 0.74 | 1.22 ± 0.74 | 0.63 |
| P2 BBT (mm) | 2.16 ± 0.64 | 1.98 ± 0.56 | 0.49 |
| P2 PBT (mm) | 1.97 ± 0.97 | 1.87 ± 0.86 | 0.8 |
| P1 BBT (mm) | 1.27 ± 0.72 | 0.78 ± 0.43 | 0.6 |
| P1 PBT (mm) | 1.44 ± 0.78 | 1.90 ± 1.29 | 0.3 |
| C BBT (mm) | 0.14 ± 0.28 | 0.57 ± 0.95 | 0.13 |
| C PBT (mm) | 2.09 ± 1.06 | 1.74 ± 1.37 | 0.48 |
| Right | |||
| M1 DI (°) | 6.85 ± 5.39 | 11.76 ± 5.08 | 0.029 ∗ |
| P2 DI (°) | 7.62 ± 4.46 | 7.35 ± 4.51 | 0.89 |
| P1 DI (°) | 4.92 ± 3.89 | 8.00 ± 5.90 | 0.14 |
| C DI (°) | 20.80 ± 7.65 | 10.98 ± 4.68 | 0.002 † |
| M1 AI (°) | 15.29 ± 4.36 | 19.23 ± 6.73 | 0.094 § |
| P1 AI (°) | 21.34 ± 11.97 | 20.54 ± 8.64 | 0.85 § |
| Left | |||
| M1 DI (°) | 10.38 ± 5.12 | 9.91 ± 5.31 | 0.82 |
| P2 DI (°) | 8.52 ± 5.83 | 8.65 ± 4.72 | 0.95 |
| P1 DI (°) | 4.3 ± 3.47 | 7.00 ± 4.39 | 0.1 § |
| C DI (°) | 15.96 ± 7.25 | 7.37 ± 5.27 | 0.00 ‡ § |
| M1 AI (°) | 14.68 ± 6.02 | 20.84 ± 9.01 | 0.055 § |
| P1 AI (°) | 24.42 ± 10.76 | 20.83 ± 7.97 | 0.37 |
| M1 BW (mm) | 47.88 ± 3.88 | 49.43 ± 4.10 | 0.34 |
| M1 PW (mm) | 34.73 ± 3.68 | 36.28 ± 4.22 | 0.33 |
| M1 AW (mm) | 28.49 ± 3.02 | 30.95 ± 4.26 | 0.1 |
| P2 BW (mm) | 41.50 ± 2.84 | 42.64 ± 3.98 | 0.46 |
| P2 PW (mm) | 29.81 ± 2.27 | 31.83 ± 4.28 | 0.18 |
| P2 AW (mm) | 33.98 ± 4.22 | 36.36 ± 4.39 | 0.24 |
| P1 BW (mm) | 36.22 ± 2.71 | 38.02 ± 3.40 | 0.17 |
| P1 PW (mm) | 24.87 ± 2.60 | 26.85 ± 3.63 | 0.14 |
| P1 AW (mm) | 28.31 ± 2.68 | 28.92 ± 3.42 | 0.63 |
| C CW (mm) | 33.06 ± 3.68 | 32.26 ± 4.80 | 0.68 |
| C AW (mm) | 24.91 ± 2.87 | 25.74 ± 3.33 | 0.56 |
| PMW (mm) | 26.38 ± 2.37 | 26.66 ± 4.28 | 0.83 |
| NW (mm) | 19.84 ± 2.11 | 20.08 ± 2.45 | 0.78 |
| IPD (mm) | 58.38 ± 4.44 | 58.16 ± 4.84 | 0.9 |
| MW (mm) | 62.70 ± 4.75 | 63.39 ± 6.21 | 0.75 |
In the hyrax and hybrid hyrax groups, the mean amounts of screw expansion were 9.75 and 10 mm, respectively.
There were treatment changes in the hyrax group. Statistically significant decreases were found in the right and left first molar and the first premolar buccal bone thicknesses ( P <0.01), whereas significant increases were noted in the first molar and the first premolar palatal bone thicknesses ( P <0.001). The right and left first molar and the first premolar dental inclinations increased significantly ( P <0.05). Similar significant changes were also found for alveolar inclinations of the first molars and first premolars, except for the left first premolar inclination. All transverse interdental measurements showed significant increases. Palatal maxillary width, maxillary width, nasal width, and distance between the lateral pterygoid plates (skeletal measurements) increased by mean values of 4.59 ± 2.15 mm ( P <0.001), 1.98 ± 2.85 mm ( P <0.05), 2.46 ± 1.69 mm ( P <0.001), and 1.06 ± 1.37 mm ( P <0.05), respectively ( Table IV ).
| T1 | T2 | T1 − T2 | P | |
|---|---|---|---|---|
| Right | ||||
| M1 MBBT (mm) | 1.28 ± 0.72 | 0.53 ± 0.56 | 0.74 ± 0.63 | 0.001 † |
| M1 DBBT (mm) | 1.85 ± 0.84 | 1.12 ± 0.65 | 0.73 ± 0.74 | 0.004 † |
| M1 PBT (mm) | 1.06 ± 0.88 | 2.79 ± 1.12 | −1.72 ± 0.73 | 0.0001 ‡ |
| P2 BBT (mm) | 1.92 ± 0.75 | 2.05 ± 0.69 | −0.11 ± 0.41 | 0.33 |
| P2 PBT (mm) | 2.08 ± 1.39 | 2.18 ± 1.34 | −0.93 ± 0.99 | 0.74 |
| P1 BBT (mm) | 1.17 ± 0.64 | 0.56 ± 0.62 | 0.60 ± 0.42 | 0.00 ‡ |
| P1 PBT (mm) | 1.73 ± 1.05 | 2.75 ± 1.13 | −1.01 ± 1.10 | 0.00 ‡ |
| C BBT (mm) | 0.21 ± 0.48 | 0.20 ± 0.37 | 0.013 ± 0.20 | 0.81 |
| C PBT (mm) | 2.01 ± 1.08 | 2.00 ± 0.79 | 0.06 ± 0.71 | 0.97 |
| Left | ||||
| M1 MBBT (mm) | 1.23 ± 0.98 | 0.36 ± 0.57 | 0.87 ± 0.75 | 0.001 † |
| M1 DBBT (mm) | 1.93 ± 1.00 | 0.98 ± 0.82 | 0.95 ± 0.71 | 0.00 ‡ |
| M1 PBT (mm) | 1.08 ± 0.74 | 2.84 ± 0.69 | −1.75 ± 0.64 | 0.00 ‡ |
| P2 BBT (mm) | 2.16 ± 0.64 | 1.82 ± 0.67 | 0.34 ± 0.55 | 0.043 ∗ |
| P2 PBT (mm) | 1.97 ± 0.97 | 2.18 ± 0.88 | −0.21 ± 0.75 | 0.32 |
| P1 BBT (mm) | 1.27 ± 0.72 | 0.47 ± 0.61 | 0.80 ± 0.65 | 0.001 † |
| P1 PBT (mm) | 1.44 ± 0.78 | 2.97 ± 1.06 | −1.53 ± 0.82 | 0.00 ‡ |
| C BBT (mm) | 0.14 ± 0.28 | 0.26 ± 0.45 | −0.12 ± 0.53 | 0.41 |
| C PBT (mm) | 2.09 ± 1.06 | 2.26 ± 0.89 | −0.16 ± 0.62 | 0.36 |
| Right | ||||
| M1 DI (°) | 6.85 ± 5.39 | 13.62 ± 8.71 | −6.77 ± 8.03 | 0.01 ∗ § |
| P2 DI (°) | 7.62 ± 4.46 | 4.99 ± 3.59 | 2.42 ± 5.60 | 0.14 |
| P1 DI (°) | 4.92 ± 3.89 | 7.64 ± 6.60 | −2.71 ± 4.53 | 0.05 |
| C DI (°) | 20.80 ± 7.65 | 19.28 ± 7.21 | 1.28 ± 5.41 | 0.41 § |
| M1 AI (°) | 15.29 ± 4.36 | 18.63 ± 5.00 | −3.33 ± 5.13 | 0.037 ∗ |
| P1 AI (°) | 21.34 ± 11.97 | 26.01 ± 10.48 | −4.67 ± 3.82 | 0.001 † § |
| Left | ||||
| M1 DI (°) | 10.38 ± 5.12 | 13.35 ± 6.37 | −2.96 ± 3.47 | 0.01 ∗ |
| P2 DI (°) | 8.52 ± 5.83 | 7.45 ± 5.27 | 1.06 ± 6.97 | 0.59 § |
| P1 DI (°) | 4.3 ± 3.47 | 6.63 ± 5.51 | −2.33 ± 3.03 | 0.017 ∗ § |
| C DI (°) | 15.96 ± 7.25 | 19.75 ± 7.42 | −2.68 ± 8.88 | 0.076 |
| M1 AI (°) | 14.68 ± 6.02 | 18.17 ± 6.09 | −3.48 ± 4.47 | 0.016 ∗ § |
| P1 AI (°) | 24.42 ± 10.76 | 27.00 ± 8.99 | −2.58 ± 5.60 | 0.122 |
| M1 BW (mm) | 47.88 ± 3.88 | 56.39 ± 4.49 | −8.51 ± 2.35 | 0.00 ‡ |
| M1 PW (mm) | 34.73 ± 3.68 | 43.34 ± 3.78 | −8.60 ± 2.01 | 0.00 ‡ |
| M1 AW (mm) | 28.49 ± 3.02 | 36.21 ± 4.73 | −7.71 ± 3.82 | 0.00 ‡ |
| P2 BW (mm) | 41.50 ± 2.84 | 50.01 ± 3.64 | −7.85 ± 3.33 | 0.00 ‡ |
| P2 PW (mm) | 29.81 ± 2.27 | 38.66 ± 3.56 | −8.17 ± 3.55 | 0.00 ‡ |
| P2 AW (mm) | 33.98 ± 4.22 | 37.36 ± 3.01 | −3.12 ± 3.24 | 0.004 † |
| P1 BW (mm) | 36.22 ± 2.71 | 43.70 ± 4.71 | −7.48 ± 4.21 | 0.00 ‡ |
| P1 PW (mm) | 24.87 ± 2.60 | 33.98 ± 4.40 | −9.11 ± 3.66 | 0.00 ‡ |
| P1 AW (mm) | 28.31 ± 2.68 | 35.14 ± 4.22 | −6.83 ± 3.76 | 0.00 ‡ |
| C CW (mm) | 33.06 ± 3.68 | 36.27 ± 3.21 | −2.47 ± 2.03 | 0.00 ‡ |
| C AW (mm) | 24.91 ± 2.87 | 28.34 ± 3.92 | −2.63 ± 2.82 | 0.003 † |
| PMW (mm) | 26.38 ± 2.37 | 30.98 ± 3.67 | −4.59 ± 2.15 | 0.00 ‡ |
| NW (mm) | 19.84 ± 2.11 | 22.30 ± 2.45 | −2.46 ± 1.69 | 0.00 ‡ |
| IPD (mm) | 58.38 ± 4.44 | 59.45 ± 4.52 | −1.06 ± 1.37 | 0.016 ∗ |
| MW (mm) | 62.70 ± 4.75 | 64.69 ± 5.25 | −1.98 ± 2.85 | 0.027 ∗ |
There were also treatment changes in the hybrid hyrax group. Only significant periodontal changes were observed in the molar measurements. Right and left mesiobuccal and distobuccal bone thicknesses for the first molars decreased, with mean values of 0.89 ± 0.46 mm ( P <0.001) and 0.98 ± 0.61 mm ( P <0.001) for the mesiobuccal thicknesses, and 0.86 ± 0.88 mm ( P <0.01) and 1.16 ± 0.38 mm ( P <0.001) for the distobuccal thicknesses, respectively. Significant amounts of bone thickening were found in the palatal bone plate of the molars ( P <0.001). As for the hyrax group, all transverse interdental and skeletal measurements showed significant increases ( Table V ).
| T1 | T2 | T1 − T2 | P | |
|---|---|---|---|---|
| Right | ||||
| M1 MBBT (mm) | 1.73 ± 0.66 | 0.83 ± 0.72 | 0.89 ± 0.46 | 0.00 ‡ |
| M1 DBBT (mm) | 2.20 ± 0.91 | 1.33 ± 0.75 | 0.86 ± 0.88 | 0.006 † |
| M1 PBT (mm) | 1.62 ± 0.58 | 2.91 ± 0.60 | −1.29 ± 0.58 | 0.00 ‡ |
| P2 BBT (mm) | 1.83 ± 0.89 | 1.83 ± 0.74 | −0.00 ± 0.38 | 0.99 |
| P2 PBT (mm) | 1.74 ± 0.72 | 2.16 ± 1.00 | −0.27 ± 0.42 | 0.04 ∗ |
| P1 BBT (mm) | 1.01 ± 0.70 | 0.69 ± 0.67 | 0.14 ± 0.96 | 0.23 |
| P1 PBT (mm) | 2.51 ± 1.66 | 2.70 ± 1.95 | −0.40 ± 1.27 | 0.57 |
| C BBT (mm) | 0.40 ± 0.85 | 0.39 ± 0.76 | 0.01 ± 0.46 | 0.92 |
| C PBT (mm) | 2.40 ± 1.46 | 2.31 ± 1.89 | 0.09 ± 1.02 | 0.77 |
| Left | ||||
| M1 MBBT (mm) | 1.57 ± 1.03 | 0.58 ± 0.74 | 0.98 ± 0.61 | 0.00 ‡ |
| M1 DBBT (mm) | 2.67 ± 0.80 | 1.51 ± 0.82 | 1.16 ± 0.38 | 0.00 ‡ |
| M1 PBT (mm) | 1.22 ± 0.74 | 3.02 ± 0.75 | −1.79 ± 0.96 | 0.00 ‡ |
| P2 BBT (mm) | 1.98 ± 0.56 | 1.72 ± 0.70 | 0.19 ± 0.64 | 0.32 |
| P2 PBT (mm) | 1.87 ± 0.86 | 1.93 ± 0.64 | −0.04 ± 0.52 | 0.78 |
| P1 BBT (mm) | 0.78 ± 0.43 | 0.76 ± 0.61 | 0.009 ± 0.59 | 0.95 |
| P1 PBT (mm) | 1.90 ± 0.29 | 1.78 ± 1.71 | 0.09 ± 0.68 | 0.62 |
| C BBT (mm) | 0.57 ± 0.95 | 0.41 ± 1.01 | 0.13 ± 0.45 | 0.31 |
| C PBT (mm) | 1.74 ± 1.37 | 1.55 ± 1.23 | 0.15 ± 0.98 | 0.59 |
| Right | ||||
| M1 DI (°) | 11.76 ± 5.08 | 14.19 ± 4.24 | −2.43 ± 5.53 | 0.15 § |
| P2 DI (°) | 7.35 ± 4.51 | 5.82 ± 4.73 | 1.01 ± 2.86 | 0.25 |
| P1 DI (°) | 8.00 ± 5.90 | 9.30 ± 4.54 | −1.54 ± 2.84 | 0.16 |
| C DI (°) | 10.98 ± 4.68 | 10.10 ± 5.76 | 0.80 ± 5.30 | 0.61 § |
| M1 AI (°) | 19.23 ± 6.73 | 22.22 ± 5.41 | −2.98 ± 5.59 | 0.091 § |
| P1 AI (°) | 20.54 ± 8.64 | 24.17 ± 6.95 | −3.63 ± 9.39 | 0.38 § |
| Left | ||||
| M1 DI (°) | 9.91 ± 5.31 | 12.81 ± 6.90 | −2.89 ± 4.90 | 0.06 |
| P2 DI (°) | 8.65 ± 4.72 | 6.15 ± 4.22 | 2.54 ± 5.51 | 0.19 § |
| P1 DI (°) | 7.00 ± 4.39 | 6.50 ± 4.06 | 0.45 ± 2.51 | 0.54 § |
| C DI (°) | 7.37 ± 5.27 | 6.28 ± 5.03 | 0.90 ± 1.74 | 0.1 |
| M1 AI (°) | 20.84 ± 9.01 | 23.30 ± 9.91 | −2.46 ± 5.93 | 0.17 § |
| P1 AI (°) | 20.83 ± 7.97 | 22.03 ± 7.64 | −1.10 ± 3.13 | 0.24 |
| M1 BW (mm) | 49.43 ± 4.10 | 58.52 ± 4.05 | −9.08 ± 2.60 | 0.00 ‡ |
| M1 PW (mm) | 36.28 ± 4.22 | 45.41 ± 4.24 | −9.12 ± 2.72 | 0.00 ‡ |
| M1 AW (mm) | 30.95 ± 4.26 | 36.97 ± 4.99 | −6.02 ± 3.06 | 0.00 ‡ |
| P2 BW (mm) | 42.64 ± 3.98 | 49.42 ± 5.03 | −4.52 ± 3.83 | 0.00 ‡ |
| P2 PW (mm) | 31.83 ± 4.28 | 38.88 ± 4.60 | −4.69 ± 3.83 | 0.00 ‡ |
| P2 AW (mm) | 36.36 ± 4.39 | 40.49 ± 5.99 | −2.74 ± 3.43 | 0.012 ∗ |
| P1 BW (mm) | 38.02 ± 3.40 | 41.84 ± 4.61 | −3.18 ± 2.58 | 0.001 † |
| P1 PW (mm) | 26.85 ± 3.63 | 31.43 ± 5.04 | −3.82 ± 2.73 | 0.00 ‡ |
| P1 AW (mm) | 28.92 ± 3.42 | 33.45 ± 4.51 | −3.77 ± 3.03 | 0.001 † |
| C CW (mm) | 32.26 ± 4.80 | 34.09 ± 4.65 | −1.52 ± 1.62 | 0.006 † |
| C AW (mm) | 25.74 ± 3.33 | 30.94 ± 4.05 | −4.32 ± 3.27 | 0.00 ‡ |
| PMW (mm) | 26.66 ± 4.28 | 30.79 ± 5.65 | −4.12 ± 2.46 | 0.00 ‡ |
| NW (mm) | 20.08 ± 2.45 | 22.71 ± 2.84 | −2.54 ± 1.94 | 0.034 ∗ |
| IPD (mm) | 58.16 ± 4.84 | 59.36 ± 5.39 | −1.20 ± 1.72 | 0.004 † |
| MW (mm) | 63.39 ± 6.21 | 66.02 ± 6.14 | −2.62 ± 2.38 | 0.003 † |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


