Fig. 17.1
(a) Mesiodistal section of premolar monkey tooth (macaque iris) after in vivo treatment using resorcinol formaldehyde resin (Robinson et al. 1976). The resin is seen as a red colouration extending from the lesion surface to the visible limit of the lesion. In this instance, this is the dark zone. (b) Electron microradiograph of human white spot carious enamel, ~dark zone region after infiltration with 14C-labelled resorcinol formaldehyde resin in vitro (Robinson et al. 1976). The section is viewed with the radiographic film in situ. The prism outlines are visible as dense black lines (arrows). This may be due to fogging by the labelled phenol but, in addition, reduction by the resin itself. The image indicates penetration of resin along prism boundaries in the earliest parts of the lesion. Bar = 1 μm
While not being clinically suitable, this material did establish proof of principle in terms of very effective infiltration of caries lesions of enamel with a protective effect against further acid attack. It also highlighted the issues of determining the extent of penetration and the extent to which lesion pores had been occluded.
17.3.4.2 Methacrylate-Based Resins
To date, the ubiquitous methacrylates and their derivatives have received most detailed investigation. The methacrylates present numerous advantages. They are easily available, and many are already in use in dentistry alleviating the need for extensive toxicology trials. Although not completely without risk, a great deal of work has established their biocompatibility (Hume and Gerzina 1996) and their physical properties both before and after polymerisation. They are also relatively easy to polymerise in the oral environment.
Using existing resin preparations, some lesion infiltration by methacrylate resins was reported by Davila et al. (1975). Later studies achieved almost complete penetration in some cases (Rodda and Patanapiradej 1983; Robinson et al. 2001; Gray and Shellis 2002). The more successful preparations with suitable properties are in fact adhesives. Their more effective penetration is most likely a result of lower viscosity and lower surface tension than corresponding unfilled resin preparations. Some of these have already shown potential for use with regard to infiltration of caries lesions, for example, Scotchbond, Gluma 2000, All-Bond 2 and Amalgambond plus (Robinson et al. 2001). Using artificial white spot caries, i.e. demineralised enamel, to allow direct comparisons, some products showed deep penetration throughout the observable demineralised region as well as occlusion of most lesion porosity. Preparations which were less successful tended to be more viscous. Those which showed penetration also conferred a resistance to further acid attack.
In terms of development, an advantage of methacrylate-based preparations is that their physical properties can be selected or altered to suit usage. Etching compounds can be included to open up the surface for adhesion and penetration. In addition, viscosity and surface tension can be altered to improve penetration into the extremely small pores of the lesion (Buonocore 1955; Simonsen 2002; Irinoda et al. 2000; Paris et al. 2007; Meyer-Lueckel and Paris 2010). The latter authors proceeded to develop a modified methacrylate-based resin preparation specifically designed for infiltration. This has shown good penetration of natural lesions with intact surfaces and conferred resistance to further acid attack (Paris et al. 2010, 2013). This product has also shown some success in treating lesions within narrow molar fissures (Paris et al. 2014). Subsequently a wide range of available dental products, mainly methacrylate based, have been investigated for both lesion penetration and the effect on further exposure to acid attack. These comprised both unfilled resins per se and adhesive materials. Adhesive materials seem to show more promise than most resins probably due to their lower viscosity and the fact that many include etching properties derived from incorporated acids which would assist opening up the surface zone of the lesion. Some of these are indicated below. The adhesives Xeno bond V and Single bond variants based on a hydroxyethyl methacrylate adhesive showed good penetration and considerable inhibition of further demineralisation in both cavitated and non-cavitated lesions (El-Kalla et al. 2012). In addition, methacrylate modified with triethylene glycol was also found to be very effective, supporting the view that more hydrophilic properties may facilitate infiltration (Meyer-Lueckel and Paris 2010). A combination of both adhesive (Heliobond) and resin (Icon) was studied by Schmidlin et al. (2012) and proved more effective than resin alone. All showed some protective effect compared with untreated lesions. While this may be due to protection of the crystals within the lesion, judging from the histological data, blocking of surface pores may be as important as infiltration of the entire lesion.
For individual resins, penetration was often variable particularly in the case of natural lesions. Reasons for this variation most probably lie with the state of the lesion. Differences in the extent of demineralisation of the lesion associated with variations in pore size, pore distribution and pore volume (Arnold and Gaengler 2012). For example, inactive lesions were less readily penetrated or protected by resin probably due to smaller pores especially in the outer regions of the lesion where more remineralisation would be expected (Neuhaus et al. 2013). Other components may also affect resin behaviour. Saliva contamination before resin treatment reduced the protective effect of resin against acid demineralisation. This may be due to compromised penetration of resin by salivary proteins (Gelani et al. 2014).
In addition, however, the use of acid in opening up or removing the surface zone and the way it is applied need to be considered. Acid containing gels and painting the lesion surface with acid have been used, and in this respect it was found that hydrochloric acid was more effective than phosphoric acid (Robinson et al. 1976; Paris et al. 2007). This is likely due to the fact that the use of acid gels or painting the enamel surface do not agitate the applied acid. From early work, etching enamel with poor agitation leads to local concentration of acid anions and dissolved calcium phosphate. In the case of phosphoric acid, this will not only limit dissolution but can also result in some redeposition of phosphate-containing mineral, perhaps obscuring the small pores of the enamel lesion. In support of this view, more success was achieved when gels were rubbed on to lesion surfaces when it was also reported that addition of abrasion also facilitated penetration (Lausch et al. 2015). For this reason an extremely fine localised hydrochloric acid spray was used in early experimentation (Robinson et al. 1976, 2000).
There are some disadvantages with current methacrylate preparations. The methacrylates are not self-polymerising and require light activation and/or catalytic activation. Catalytic activators may be cytotoxic, and their possible interface with live tissue, i.e. dentin or pulp, must be taken into account. In this context, light activation would be preferable. However, the stagnation sites where lesions occur, i.e. in deep molar fissures and interproximal areas between teeth, are not necessarily easily penetrated by light. This could lead to the possibility of incomplete polymerisation and a resulting weak polymer and/or of residual monomer leaching from the lesion into adjacent tissue. Long-term effects of this possibility are not yet known.
Most importantly all of the work to date concerning infiltration of caries lesions has indicated that with current materials, opening up of the surface zone and/or removing some surface enamel is an almost necessary prerequisite for successful infiltration. The removal of the lesion surface does, however, raise issues with regard to the surface integrity of the infiltrated lesion over the long term and effects on the adhesion of pellicle and plaque proteins.
17.3.5 Detection of Resin Within the Lesion and Measurement of Occluded Volume
In developing materials specifically for infiltration, the depth of penetration and the ultrastructural location of infiltrant are important parameters in assessing effectiveness. Determination of volume of lesion pores occluded, i.e. filled by resin, is also extremely important in this respect. Data on volume of pores occluded not only provides information concerning penetration effectiveness but also on resin shrinkage during treatment. If the method is nondestructive, it can be used to assess the effects of further acid attack on the treated lesions directly by measuring any increase in pore volume due to further demineralisation.
17.3.5.1 Detection of Infiltrated Resin
As far as penetration is concerned, incorporation of dye into the resin is useful for simple visualisation of penetration (Robinson et al. 2001). For greater resolution, confocal laser scanning microscopy (CLSM) is a valuable tool and has provided useful data on the extent of resin infiltration as well as some data on histological location. In those parts of the lesion infiltrated, this has demonstrated that resin appears to occupy the body of enamel prisms (Fig. 17.2) (Paris et al. 2007). It is of interest to note here that while resin (the methacrylate-based adhesive Excite) was present in the bodies of prisms, the prism boundaries, a region considered to be at least as porous as prism bodies, seemed to contain less resin. The porosity of both prism bodies and prism boundaries is clearly seen by green fluorescein staining of non-infiltrated regions of the lesion. This may be due to local variations in pore structure, but whatever the reason for this is, it raises the important question that while resin may be visibly present, it does not indicate the extent to which porosities are actually occluded. Fully occluded pores would offer maximum protection against further entry of acid and egress of dissolved mineral ions as well as conferring maximum mechanical support. See also Gelani et al. (2014). CLSM has limited penetration into enamel such that estimating penetration depth from the outer surface is limited. Currently such assessments are carried out on tooth sections after in vitro or if possible after in vivo administration. The resin must be labelled with a fluorescent probe to render it visible.
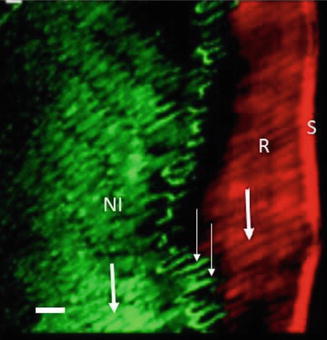
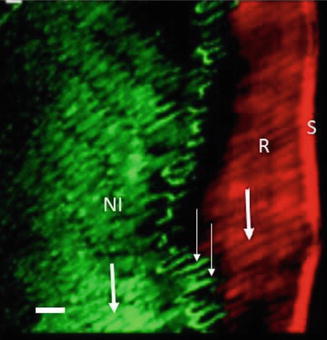
Fig. 17.2
CLSM image of an HCl-etched lesion treated with the adhesive Excite (Adapted from Paris et al. 2007 with permission). S surface of lesion, R the outermost 50–100 μm of prism cores are filled with resin (red fluorescence heavy arrow), NI non-infiltrated parts of the lesion body, the highly porous prism cores (heavy arrow) and prism boundaries (light arrows) show green fluorescence. Bar = ~10 μm
Radiographic procedures are appropriate if resins are rendered radio-opaque. This is not feasible, however, with current methacrylate-based resins since they are radiolucent. Incorporation of radio-opaque components or a radio-opaque filler would be necessary. The technology is, however, of value in assessing the protective effect of resin against further demineralisation. Autoradiography is also a useful approach for investigations in vitro and has the possibility for detailed ultrastructural location (see Fig. 17.1b).
17.3.5.2 Determination of Occluded Pore Volume
Measurement of volume occluded by resin is also an important parameter as indicated above. Partially occluded pores will offer less protection to further acid attack as well as poorer mechanical support.
Determination of occluded pore volume is not easily achieved but has been attempted in studies with resorcinol formaldehyde and some dental resin adhesives (Robinson et al. 1976, 2001). Lesion pores were infiltrated with 2-chloronaphthalene, known to penetrate even the pores of the earliest stages of lesion formation. Quantitative extraction of the 2-chloronaphthalene permitted a determination of accessible lesion pore volume. Subsequent measurement after resin infiltration provided a measurement of volume occluded by resin. This also permitted a measurement of resin shrinkage. This was up to 30 % for the resorcinol preparation but was reduced to almost zero by a second treatment indicating almost 100 % pore occlusion. The method was highly reproducible in artificial lesions (6 % standard deviation) but was less so for natural lesions. This is most likely due to more complex pore structure of natural lesions and the presence of organic material such as proteins in the lesion (Robinson et al. 1998; Shore et al. 2000).
17.3.6 Effects of Infiltration on Carious Tissue
Infiltration as a clinical treatment is still at an early stage so that there is little data on the long-term effects of infiltration on caries lesions. A systematic review has concluded that the treatment is useful for preventing caries progression in lesions with intact surfaces, but studies are required to establish durability of the treatment in terms of tooth integrity as well as caries progress (Doméjean et al. 2015). Some shorter-term investigations have been carried out mainly with regard to cosmetic acceptability of the treatment especially on lesions resulting from stagnation around orthodontic brackets.
These reported an initial improvement in lesion appearance which was sustained over a 6-month or 1-year period. This suggests that resin treatment did not result in a lesion surface which was prone to staining rendering it suitable for visible sites in the mouth (Feng and Chu 2013; Borges et al. 2014; Knösel et al. 2013). It may also suggest that the surface was not rendered more prone to plaque deposition.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


