Introduction
Current studies have compared indirect bonding with direct placement of orthodontic brackets; many of these have shown that indirect bonding is generally a more accurate technique. However, the reproducibility of an indirect bonding setup by an orthodontist has yet to be described in the literature. Using cone-beam computed tomography and computer-assisted modeling software, we evaluated the consistency of orthodontists in placing orthodontic brackets at different times.
Methods
Five orthodontists with experience in indirect bonding were selected to place brackets on 10 different casts at 3 time periods (n = 30 per orthodontist). Each participant completed an initial indirect bonding setup on each cast; subsequent bracket placements were completed twice at monthly intervals for comparison with the initial setup. The casts were scanned using an iCAT cone-beam computed tomography scanner (Imaging Sciences International, Hatfield, Pa) and imported into Geomagic Studio software (Geomagic, Research Triangle Park, NC) for superimposition and analysis. The scans for each time period were superimposed on the initial setup in the imaging software, and differences between bracket positions were calculated. For each superimposition, the measurements recorded were the greatest discrepancies between individual brackets as well as the mean discrepancies and standard deviations between all brackets on each cast.
Results
Single-factor and repeated-measure analysis of variance showed no statistically significant differences between time points of each orthodontist, or among the orthodontists for the parameters measured. The mean discrepancy was 0.1 mm for each 10-bracket indirect bonding setup.
Conclusions
Orthodontists are consistent in selecting bracket positions for an indirect bonding setup at various time periods.
The straight-wire appliance is based on the concept that ideal bracket placement will correct tooth positions in all 3 planes of space during treatment. Accurate bracket placement is essential for effective and efficient orthodontic treatment. However, many practitioners apply brackets indiscriminately, making the finishing stage of comprehensive orthodontic treatment more difficult and time-consuming. Carlson and Johnson have enumerated 4 elements that demand attention when initially positioning brackets: (1) bracket base adaptation to the contour of the tooth surface, (2) evaluation of the rotational position of each bracket from the occlusal direction, (3) determination of the vertical position of each bracket, and (4) determination of the desired slot angulations of each bracket by evaluating the position of the roots. All of these elements are necessary for ideal bracket placement and can be adequately visualized when completing an indirect bonding setup. Hodge et al stated that the main advantage of indirect bonding over direct bonding is a reduction in the envelope of error in bracket position in each of the 3 orientations examined (vertical, horizontal, and angular).
Several studies have shown that indirect bonding is generally a more accurate technique for bracket placement than direct bonding. Improving bracket placement accuracy reduces the need for subsequent repositioning and can even shorten treatment time. Currently, several companies advertise a computer-aided bracket placement system from which, after submission of a pretreatment cast, an impression, or an intraoral scan, an indirect setup can be provided ready for bonding. A computer algorithm defines the shape of each tooth on the 3-dimensional model, establishes the spatial relationships of the teeth, and calculates the ideal bracket placement on the virtual model. An indirect bonding tray is then returned to the provider. Research has shown that the computerized tools used in this process provide accurate bracket placement, possibly supporting the companies’ claims that they provide significant decreases in treatment time. However, although computer algorithms can provide precise reproducibility, the human element is advantageous to incorporate alterations from the technically “ideal” placement to provide overcorrection of rotated teeth or accentuated tip to resist unwanted root movement during space closure mechanics, for example. Therefore, orthodontists might vary somewhat in their perceptions of ideal bracket placement and even alter their individual “ideal” over time.
Would bracket placement by an orthodontist for indirect bonding have similar results as shown in the customized commercial setups? How consistent would a provider be if given the same casts on which to place brackets at different time periods? Taylor and Cook assessed the variability in bracket position as a range on 3 occasions when brackets were placed. In their study, brackets were placed on a typodont model from maxillary canine to maxillary canine on 3 separate occasions a minimum of 4 weeks apart. They concluded that 12 experienced providers positioned brackets differently from each other, and the providers failed to reposition brackets in identical positions on subsequent occasions. However, an evaluation of bracket placement consistency on “real-world” cases would be useful in determining whether orthodontists would consistently select the same bracket placements to manage all the requirements for tooth movement in crowded occlusions with rotated and tipped teeth.
The purposes of this study were to evaluate the previously mentioned scenario and to assess the ability of orthodontic providers to place orthodontic brackets in the same positions on the same casts of crowded dentitions at different times for an indirect bonding setup. Consistency in bracket placement was evaluated using cone-beam computed tomography (CBCT) technology combined with computer-aided modeling software to superimpose and evaluate bracket positions 3 dimensionally.
Material and methods
Five orthodontists experienced in indirect bonding were selected to place brackets on 5 different orthodontic model sets at 3 times. The 5 cast sets (maxillary and mandibular comprised each set) along with the corresponding panoramic radiographs were chosen by 1 investigator (G.G.) from preorthodontic study models of patients with varying degrees of crowding. These patient records were selected from those treated in the Tri-Service Orthodontic Residency Program at Lackland Air Force Base in Texas. Each set of models had a full complement of permanent teeth from second premolar to second premolar, and no abnormally worn dentitions, fractured teeth, or severe crowding that would prevent orthodontic bracket placement in ideal positions. Each panoramic x-ray and the corresponding casts were deidentified to ensure that all protected health information was removed and then numbered for tracking purposes. The original casts were duplicated using alginate (Jeltrate; Dentsply, York, Pa) and poured in Die-Keen green jade stone (Heraeus Modern Materials, South Bend, Ind). For each model, a 1-mm clear vacuform stent (Dentsply Raintree Essix, Bradenton, Fla) was fabricated and replaced each time the brackets were placed. This allowed the orthodontist to place brackets onto the same model unmarred from prior bracket placement and still visualize the teeth underneath. Consistency for the vacuform stent was maintained using the same machine, stent material, laboratory technician, and duplicated casts. The numbered models were then distributed to the orthodontists with the vacuform stent fitted onto the model, upon which the brackets were placed.
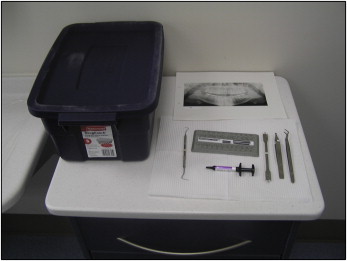
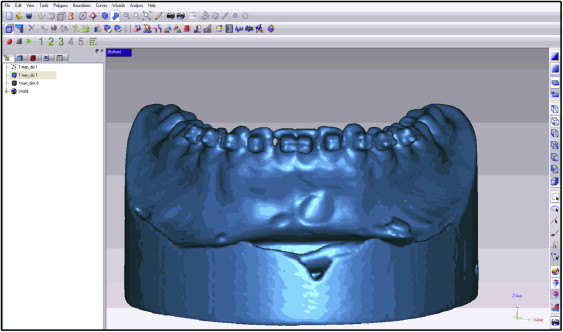
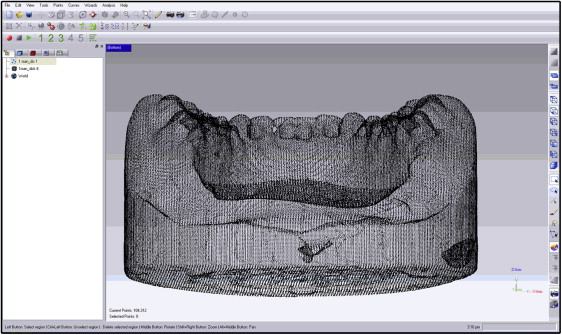
Each provider was given an explorer, bracket placement forceps, bracket height gauges, a panoramic x-ray from the patient, a curing light, orthodontic brackets, and a dispensing syringe of Transbond XT composite resin (3M Unitek, Monrovia, Calif) to bond the brackets ( Fig 1 ). The brackets were 0.022-in Roth prescription brackets (3M Unitek). Each orthodontist was required to place the brackets within 48 hours in his or her perceived “ideal” bonding position for each tooth and reminded to compensate 1 mm for the stent thickness if the bracket height gauge was used. The providers were instructed to place no identifying marks on the brackets, models, or vacuform stents. They placed the brackets the first day and then reviewed their placements on the second day. At the end of the second day, a dental technician collected the materials, ensuring that the casts ( Fig 2 ) were not identified or linked to any provider. The casts were then scanned with a 0.2-mm voxel size iCAT CBCT unit (Imaging Sciences International, Hatfield, Pa) at Wilford Hall Ambulatory Surgical Center, Lackland Air Force Base, with the scan protocol of 6 ×16-cm field of view, 40 seconds, 46.72 mAs, and 120 kVp. After the scan, a new vacuform stent was placed on the models and distributed to another provider with the same instruments and instructions. One month after the initial placement, each provider was given the same casts, brackets, and instruments and asked to replace the brackets. The casts were then rescanned, and the bracket positions were compared with the initial placements. This procedure was repeated after a second 1-month interval. For each time point, CBCT images were then imported into a modeling software program (Studio; Geomagic, Research Triangle Park, NC) ( Fig 3 ) to translate the data into a 3-dimensional polygon mesh of approximately 200,000 triangles per scan with vertices ( Fig 4 ). Subsequent CBCT scans for the same provider and same casts were then imported into the software ( Fig 5 ), and alignment of the casts was completed. The program’s global registration macro was then used to align the polygon meshes ( Fig 6 ). The differences in bracket positions were then measured using the base of the casts as a constant and matching the polygon meshes of the 2 time points. Color-coded superimpositions were used to demonstrate the differences, and measurements were calculated from the vertices of the point polygon mesh triangles of the 3-dimensional object for the 2 time points ( Fig 7 ). For each superimposition, the maximum distance of 1 vertex of the superimposed polygon mesh and the average distances between all vertices were measured, and standard deviations were calculated. To ensure accuracy, calibration was performed before each session using 2 scans of an identical cast in the same position, with a coarse position of the 2 models to a global origin point, performing the global registration of the 2 models, and then executing an overlay reduction of the models for the calibration.


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


