Introduction
The objective of this study was to compare the head posture of patients with obstructive sleep apnea (OSA) having different levels of severity with that of control subjects.
Methods
One hundred subjects participated in this study. Seventy-five subjects underwent overnight polysomnography in a sleep laboratory and were allocated into “mild,” “moderate,” or “severe” OSA groups, and 25 subjects with no complaints regarding OSA were allocated into 1 group and served as the controls. Cephalometric radiographs were obtained from all participants in natural head position. Craniocervical, craniovertical, and cervicovertical angles were measured in the groups. Data were analyzed using the least significant difference.
Results
The results showed significant differences between the OSA groups and the control group, and among the test groups, in all craniocervical, craniovertical, and cervicovertical angles ( P <0.05), except for 1 craniovertical measurement ( P >0.05). There were no significant differences in this measurement among the test groups and in any measurement between the mild and moderate OSA groups ( P >0.05).
Conclusions
Head posture showed significant differences in patients with OSA. In general, the more severe the OSA, the more extended the natural head position as indicated by increases in the craniocervical angles. The cervical posture parameters may indicate existing OSA.
Highlights
- •
Head posture showed significant differences in patients with sleep apnea.
- •
Cervical posture parameters may indicate existing obstructive sleep apnea.
- •
We studied the degree of extension affected by the severity of apnea on natural head position.
The word “apnea” originates from the Greek word “apnoia” and means “without breathing.” This terminology was initially used by Guilleminault et al in defining sleep apnea syndrome. Obstructive sleep apnea (OSA) causes obstruction of the upper airway during sleep and is also associated with daytime symptoms. Untreated patients with OSA may have an increased risk of comorbid disease, such as systemic hypertension, depression, stroke, angina, and cardiac dysrhythmias, and it is also known that OSA is associated with motor vehicle accidents, poor work performance, and reduced quality of life. It is difficult to determine the etiology of OSA because this syndrome is multifactorial, with neural, hormonal, muscular, and structural anatomic factors. It occurs in 2% to 4% of adults aged between 30 and 60 years.
There is a relationship between craniofacial changes and postural development, which Solow and Kreiborg termed “the soft tissue stretching hypothesis.” Upper airway obstruction causes a change in posture via extension of the craniocervical angle. This leads to an increase of the forces on skeletal structures and decreases forward growth of the maxilla and the mandible. In accordance with this hypothesis, many studies have declared that the people with OSA have an extended natural head posture (NHP), reduced posterior airway space, an abnormally long soft palate, and a low position of the hyoid bone.
Polysomnography (PSG), which is recommended as the gold standard for the diagnosis of OSA, plays a crucial role in OSA research and involves an overnight sleep study conducted in a laboratory. The polysomnogram tests electrocephalography (brain waves), electro-oculography (eye movement), electrocardiography, electromyography (chin and leg movement), sleep positioning, respiratory activity, and oxygen saturation.
Previous studies have shown that people with sleep apnea have a small, retruded mandible, a narrow posterior airway space, enlarged tongue and soft palate, an inferiorly positioned hyoid bone, and retroposition of the maxilla. However, the effects of the severity of OSA on head posture remain controversial. Therefore, the aim of this study was to compare the NHP of patients with different degrees of OSA. For the purposes of this study, the null hypothesis assumed that there are no statistically significant differences among various NHP measurements of the different OSA groups and the controls.
Material and methods
A total of 100 subjects participated in the study; they were referred from both the Department of Orthodontics and the Department of Pulmonary Diseases, University of Gaziantep, in Turkey. Ethical approval was obtained from the university’s ethics committee.
The participants underwent overnight PSG in the sleep laboratory in the Pulmonary Disease Department of Gaziantep University. PSG data were obtained while they were asleep, under the supervision of a sleep laboratory technician.
The severity of OSA was determined using the apnea-hypopnea index (AHI), which was defined as the sum of mixed obstructive apnea and hypopnea events per hour of sleep when the participant was undergoing PSG. The study sample consisted of 3 groups of 25 subjects each ( Table I ). They were allocated into groups according to the severity of their OSA. The guidelines of American Academy of Sleep Medicine Task Force were used for grouping: mild OSA (AHI, 5-15), moderate OSA (AHI, 16-30), and severe OSA (AHI, >30). The mean ages of the participants were 49.08 ± 12.92, 54.20 ± 11.13, and 50.44 ± 7.49 years for the mild, moderate, and severe groups, respectively. The control group consisted of another 25 adults from the Department of Orthodontics who did not undergo PSG. The control group selection criteria were no report of sleep disorder or snoring, no previous apnea, and no surgery related to the maxillary or mandibular region. The mean age in the control group was 33.40 ± 10.81 years.
| Group | N | Age, mean ± SD (y) | Sex, male/female |
|---|---|---|---|
| 1 (control) | 25 | 33.40 ± 10.81 | 18/7 |
| 2 (mild OSA) | 25 | 49.08 ± 12.92 | 13/12 |
| 3 (moderate OSA) | 25 | 54.20 ± 11.13 | 17/8 |
| 4 (severe OSA) | 25 | 50.44 ± 7.49 | 18/7 |
Cephalometric radiographs were obtained from all participants under standardized conditions with their teeth in centric occlusion, their head in a natural position (mirror position) without a head holder, and their lips in a habitual posture, as described by Solow and Siersbaek-Nielsen. The radiographs were taken with the same digital x-ray unit (XG 3; Sirona, München, Germany), and 9 angles were used to evaluate the postural variables. All cephalometric radiographs were traced by the same experienced investigator (R.O.).
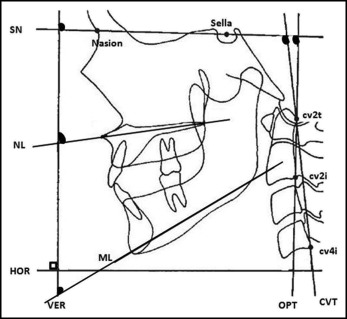
The craniocervical angulations (SN-OPT, SN-CVT) (the inclination of the head in relation to the cervical column) were expressed by angles between the craniofacial reference lines and the cervical column reference lines odontoid process tangent through cv2i-cv2t (OPT) and cervical vertebral tangent through cv4i-cv2t (CVT). The craniovertical angulations (SN-VER, NL-VER, ML-VER) (ie, the inclination of the head in relation to the true vertical) were expressed by the angles between the craniofacial reference lines, sella-nasion line, nasal line (spina nasalis anterior to spina nasalis posterior), mandibular line (gonion to gnathion), and the true vertical. The cervicovertical angulations (OPT-VER, CVT-VER) (ie, the inclination of the cervical column in relation to the true vertical) were expressed by the angle between the cervical column reference lines and the true vertical ( Fig ; Table II ).
| Reference line | Definition |
|---|---|
| SN | Sella-nasion line |
| NL and ML | Nasal line (spina nasalis anterior to spina nasalis posterior) and mandibular line (gonion to gnathion) |
| OPT | Odontoid process tangent through cv2i-cv2t |
| CVT | Cervical vertebra tangent through cv4i-cv2t |
| VER | True vertical line |
| HOR | Horizontal line |
Dahlberg’s formula was used to assess the reliability of the cephalometric measurements. A total of 20 randomly selected radiographs were retraced and remeasured by same investigator (R.0.) 3 weeks after the initial analysis. The method error ranged from 0.30° to 0.71° for the craniocervical, craniovertical, and cervicovertical angles, and the mean difference was not significant.
Statistical analysis
The statistical analysis was carried out with SPSS software for Windows (version 20; IBM, Armonk, NY). The Kolmogorov-Smirnov statistical test was used for normality analysis, which showed that the data were normally distributed: ie, the distance between the empirical distribution function of the sample and the cumulative distribution function of the reference distribution was not statistically significant, and parametric tests were used ( Table III ). The least significant difference test ( Table IV ) was applied to evaluate the intergroup differences in the variables.
| Variable | n | Kolmogorov-Smirnov normality test, P value |
|---|---|---|
| SN-CVT | 100 | 0.200 ∗ |
| SN-OPT | 100 | 0.200 ∗ |
| SN-VER | 100 | 0.114 ∗ |
| NL-VER | 100 | 0.200 ∗ |
| ML-VER | 100 | 0.200 ∗ |
| OPT-VER | 100 | 0.200 ∗ |
| CVT-VER | 100 | 0.200 ∗ |
∗ P > 0.05 showed normal distribution: ie, the distance between the empirical distribution function of the sample and the cumulative distribution function of the reference is not statistically significant, and parametric tests were applied to these variables.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


