This case report describes the significance of orthodontic treatment in reconstruction of a collapsed dental arch and a malocclusion associated with severe periodontitis. A Japanese man (age, 40 years 7 months) had an anterior crossbite, a collapsed occlusion, and severe periodontitis. Orthodontic treatment included the following steps: (1) correction of the anterior crossbite, labial movement of the maxillary incisors, and intrusion and retraction of the mandibular incisors; (2) correction of the posterior crossbite on the left side, buccal movement of the maxillary left canine and first premolars, and intrusion and retraction of the mandibular first premolar into the space of the mandibular left canine; (3) correction of the crowding of the mandibular right buccal segment and alignment of the teeth after extraction of the mandibular right first molar with a periapical lesion; and (4) improvement of the occlusion, with reconstruction of an acceptable occlusion. When combined with restorative and prosthodontic treatment, a fairly good occlusion was obtained. Reevaluation of the treatment after 11 years showed that the occlusion and periodontal condition were maintained well without deepening of the pockets and further bone loss. Orthodontic treatment with a systematic approach helped to recover the occlusion and prevented the recurrence of periodontitis by acquiring a good oral environment and motivating the patient to maintain oral health.
In advanced periodontal disease, collapse of the dental arch often occurs with increased tooth mobility. The situation worsens if there is an anterior crossbite. The traumatic occlusion could cause further breakdown of the periodontium as toothbrushing and maintaining oral hygiene become difficult. Consequently, the situation further exacerbates the periodontal destruction. The loss of teeth would lead to collapse of the occlusion and a reduced quality of life, because oral health is critical for food intake and communication. Reconstruction of the occlusion and alignment of the malposed teeth with orthodontic treatment become necessary not only to prevent disease progression, but also to satisfy patients’ functional, esthetic, and communication demands. This case report describes the favorable and stable outcome of a multidisciplinary approach involving orthodontic and periodontal management for treating a patient with advanced periodontitis, severe tooth mobility, anterior crossbite, and collapse of the occlusion.
Diagnosis and etiology
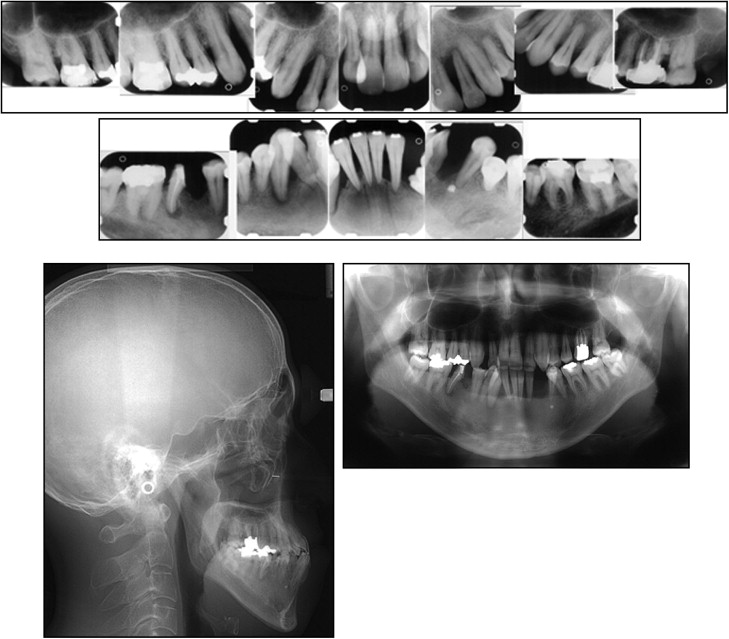
A Japanese man (age, 40 years 7 months) was referred by a periodontist (K.G.) to our clinic at Tsurumi University in Yokohama, Japan, to discuss the possibility of orthodontic treatment. His chief complaints were an anterior crossbite and a collapsed occlusion. The patient reported that he had periodontal inflammation at an early age; it gradually caused collapse of his occlusion. On his first visit to the periodontist, the clinical examination showed that the pocket depth was 15 mm on the maxillary right central and lateral incisors, and most of pocket depths of the other teeth exceeded 5 or 6 mm. The apical area of the mandibular left canine was exposed to the oral cavity, indicating the severity of his periodontitis ( Figs 1 and 2 ). Before the orthodontic examination, the patient received periodontal treatment aiming at complete exclusion of the infection source and reduction of deep periodontal pockets to a depth of less than 3 mm.


At the time of the orthodontic evaluation, the periodontal condition had improved considerably, and there were no signs of gingival inflammation. The periodontal examination showed that most of the pocket depths were within 3 mm ( Fig 2 ), which indicated that the periodontal condition was favorable for orthodontic treatment. The periodontal condition was routinely monitored by a periodontist.
The patient had a concave profile ( Fig 3 ). The dental examination showed an anterior crossbite with an overjet of −2.0 mm and an overbite of 1.5 mm ( Fig 4 ). The anterior teeth had severe mobility because of the loss of supporting tissues, which made mastication difficult in the anterior segment. The posterior segment showed an Angle Class III molar relationship and a crossbite between the maxillary left canine and premolar, and the mandibular first premolar. There was spacing in the maxillary arch. In the mandibular arch, the left canine had been extracted because of periodontitis, and there was moderate crowding in the mandibular right buccal segment. Severe gingival recession was observed, especially in the anterior teeth with severe tooth mobility.

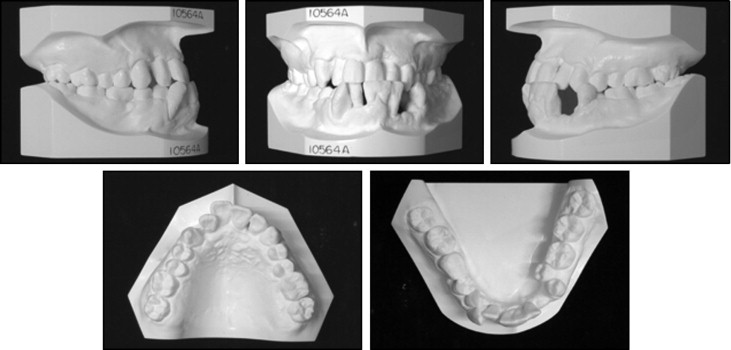
The radiographic examination showed severe alveolar bone loss in the maxillary and mandibular anterior regions. The mandibular anterior teeth and the maxillary lateral incisors on both sides showed alveolar bone losses of 80% to 90% ( Fig 5 ). There were periapical lesions in relation to the mandibular right first molar (hemi-sectioned) and the right canine, and periodontal space widening at the maxillary right and left lateral incisors. Lateral cephalometric analysis showed the following values: ANB angle, 0.9°; FMA, 39.9°; U1-SN, 111.0°; and L1-Mp, 72.2°. Based on the above findings, the patient was diagnosed as having a skeletal Class III malocclusion associated with severe periodontitis.
Treatment objectives
The treatment plan involved an approach to manage both the periodontitis and the malocclusion. The following objectives were established: (1) correct the crossbites in the anterior segment and the left buccal segment, (2) correct the crowding of the teeth, (3) close the spaces, and (4) improve the collapsed occlusion.
Treatment objectives
The treatment plan involved an approach to manage both the periodontitis and the malocclusion. The following objectives were established: (1) correct the crossbites in the anterior segment and the left buccal segment, (2) correct the crowding of the teeth, (3) close the spaces, and (4) improve the collapsed occlusion.
Treatment alternatives
Both the orthodontic and the prosthodontic treatment options were presented to the patient. The orthodontic treatment plan was to correct the crossbites and align the teeth after extraction of the mandibular right first molar to reconstruct an acceptable occlusion. Managing the spaces in both arches in patients with severe periodontitis is difficult, because excessive tooth movement must be avoided to prevent further loss of supporting tissue. In these cases, restorative or prosthodontic treatment might be necessary to fill the spaces and establish continuity of the arches. The prosthodontic option for treatment in our patient would have been extraction of the teeth with severe bone loss, such as the maxillary and mandibular anterior teeth, and restoration of the occlusion with partial dentures.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


