Introduction
Permanent first molars (PFM) with a poor prognosis are routinely extracted in children throughout the United Kingdom. National guidelines suggest that to achieve spontaneous closure for the mandibular arch, the PFM should be extracted at 8 to 10 years of age, during bifurcation formation of the second molar. The literature is of limited quality and has suggested alternative variables that may be associated with successful space closure. Our aim was to investigate the radiographic prognostic factors associated with space closure after extraction of PFM. Two objectives of the research are reported in this article: to determine factors that might predict space closure of the second molar after extraction of the PFM, and to develop a tool kit to aid clinical decision making.
Methods
We assessed 148 maxillary and 153 mandibular PFM extracted from 81 participants retrospectively. Dental age, second molar developmental stage, second premolar and second molar angulations, and presence or absence of the third molar were assessed on the preextraction orthopantomograms. Outcome was assessed via visual examination, study models, or radiographs.
Results
Closure occurred in 89.9% of the maxillary and 49.0% of the mandibular quadrants. Dental age was statistically, but not clinically, significant in the maxillary arch ( P <0.05). For the mandibular arch, presence or absence of the third molar and second molar angulation were statistically and clinically significant ( P <0.01 and P <0.05, respectively). A tool kit was developed in relation to the mandibular arch variables.
Conclusions
These findings are contradictory to the Royal College of Surgeons guidelines and suggest that the presence of the third molar and a mesially angulated second molar are favorable for space closure. The developed tool kit requires further validity testing.
Highlights
- •
Spontaneous space closure after first molar extraction is sometimes desirable.
- •
Guidelines suggest bifurcation development of the second molar as a predictive factor.
- •
Bifurcation may not be predictive.
- •
Second molar angulation and third molar presence may be predictive.
- •
A developed tool kit shows internal validity, but external validity is still required.
The permanent first molar is one of the first adult teeth to erupt into the mouth about 6 to 7 years of age. This early eruption, along with its position toward the back of the mouth, can make this tooth more susceptible to diseases such as dental caries. Recent dental health surveys in the United Kingdom have also shown increases in the incidence of decay associated with the first molars. This, along with developmental disorders of enamel such as molar incisal hypomineralization, results in a significant level of poor prognoses of first molars and these teeth may be incorporated into orthodontic extraction patterns. In certain occlusions where space is not required to reduce an overjet or relieve crowding, it may be beneficial to extract the first molar in circumstances that favor the mesial eruption of the second molar into this extraction space. This would eliminate or, at the very least, reduce the need for fixed appliance treatment with its associated risks, particularly in patients who may already be susceptible to dental caries. Attempting to close this extraction space can also lead to undesirable orthodontic effects such as excessive retraction of the labial segment. Empirical evidence suggests that spontaneous space closure occurs more readily in the maxillary arch. Space closure in the mandibular arch is less successful; therefore, more research has been previously undertaken to assess potential predictive factors for a successful result.
The majority of research assessing factors that could affect spontaneous space closure of the first molar space was undertaken in the 1960s and 1970s. Positive associations were found between space closure and chronologic age, angulations of the developing second molar and second premolar. presence of the third molar, crowding, and skeletal relationships including retrognathic maxillae and prognathic mandibles. However, these studies relied on subjective measures of outcome, lacked statistical analyses, and had incomplete reporting of results.
Current guidelines in the United Kingdom, developed by the Royal College of Surgeons of England, state that space closure occurs relatively easily in the maxillary arch due to the root morphology of the second molar and mesial tipping of the second molar during eruption. In the mandibular arch, the guidelines suggest that interceptive extractions should be undertaken between 8 and 10 years of age. Previous guidelines suggested that extraction of the first molar when the bifurcation of the second molar is forming could be considered a predictor of successful space closure ; however, the more recent guidelines have recognized that the response of the second molar can be variable, and “acceptable positions are also possible in association with extraction at earlier and later stages of development.” However, the quality of the literature on which this is based is not robust.
The aims of this study were to investigate the following.
- 1.
Whether these radiographic prognostic factors are associated with space closure after extraction of permanent first molars: dental age at extraction, bifurcation development stage of the second molar at extraction, angulation of the second premolar at extraction, angulation of the second molar at extraction, and presence or absence of the third molar at extraction.
- 2.
If statistically and clinically significant factors are found, to develop an easy-to-use tool kit to aid clinicians in space closure prediction.
The primary null hypothesis for the study was that the factors in number 1 have no influence on successful spontaneous space closure after extraction of permanent first molars.
Material and methods
This was a retrospective cohort study. Due to the quality of the previous research, the only potential variable that could be used for sample size calculation was the developmental stage of the permanent second molar. The study with the largest sample size was used. For a power of 0.80 with a significance level of P <0.05 showing a clinically significant difference of 30% between the groups, a sample size of 49 molars was required per group (early, ideal, and late) for a total of 147 molars. It has been recognized that maxillary and mandibular second molars behave differently; therefore, these were analyzed as separate samples requiring 147 maxillary molars and 147 mandibular molars, for a total of 294.
Subjects were recruited from 4 sources according to the criteria in Table I . A previous audit in the paediatric department at the Eastman Dental Hospital identified children who had had interceptive extractions of first molars in the hospital’s general anesthetic theater (source 1). Outcome data in relation to space closure were used from this audit from patients who had attended a review (source 1A). This audit had a significant failure to attend rate; therefore, patients who did not attend the review and were no longer under the care of the hospital were recalled for this study (source 1B). Some patients in this source were still under the care of the pedatric dentistry or orthodontic department, and these patients were invited to participate in the study at their next appropriate review (source 1C). Patients were also recruited from the pediatric dentistry and orthodontic clinics on an ad hoc basis (source 2). Since this study involved patient recall and use of patient information from those who had not been discharged, ethical approval was required and granted (Research Ethics Committee number 13/WM/0398; Integrated Research Application System Project identification number 125278).
| Inclusion criteria | Exclusion criteria |
|---|---|
| Previous removal of at least 1 permanent first molar with the intention of achieving spontaneous space closure | Craniofacial syndromes and anomalies of eruption |
| Preextraction orthopantomogram of adequate quality in the medical records taken at the Eastman Dental Hospital | Extraction or hypodontia of other permanent teeth |
| Able to sign own assent (<16 years of age) or consent form (≥16 years of age or above) | Orthodontic treatment with no pretreatment record available at the Eastman Dental Hospital |
| Parent/guardian gave consent (for participants <16 years of age) | No preoperative orthopantomogram |
All radiographs were taken at the Eastman Dental Hospital (PM 2002 EC Proline; Planmeca, Helsinki, Finland). If more than 1 orthopantomogram was available, the radiograph made closest to the extraction date was used.
Calculation of dental age followed the weighted average method derived from the classification of Demirjian et al and a previously established reference data set. The reference data set determined the mean age of attainment of each stage of development for each tooth. For each participant, all maxillary and mandibular teeth on the left side of the orthopantomogram and all 4 third molars were assessed for development according to the 8-stage system ( Fig 1 ) described by Demirjian et al. Each development stage for each tooth was associated with a mean age of attainment and a standard error derived from the reference data set. The data were then copied into STATA software (version 12; StataCorp, College Station, Tex), and the weighted average was calculated using meta-analysis commands. This method factors not only the mean and standard error but also the size of each subset of data (each tooth at each developmental stage). The meta-analysis then produced a mean age for each patient.
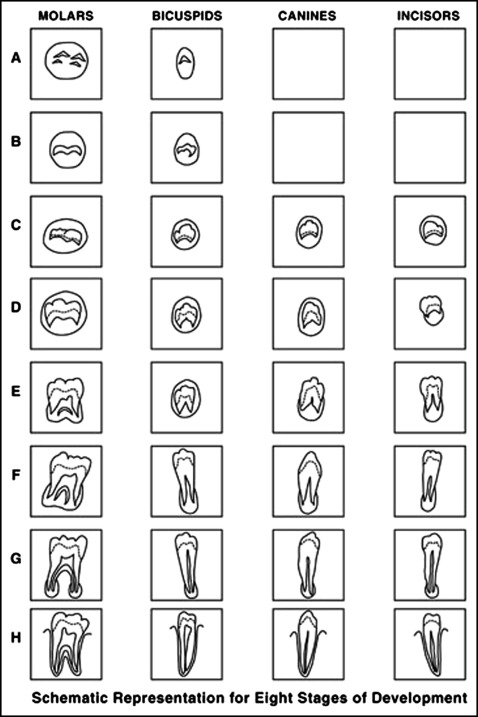
Bifurcation development stage of the second molar was assessed with the orthopantomogram placed on a light box in a darkened room. This was assessed against the 8-stage model of Demirjian et al. Stage E corresponds to bifurcation development, and this was recorded as “ideal” timing. Extraction of permanent first molars at second molar development stages A to D was termed “early” and at stages F to H, “late.”
Angulations of the second premolar and second molar were assessed using a modification of the method of Shiller. This was developed to assess the angulation of the third molars. For the permanent first molar in question, a line was traced along the occlusal plane ( white line ). As shown in Figure 2 , a line was also traced through the body of the second premolar or the second molar ( dotted line ), and the distal angle formed by the intersection of this line with the occlusal plane was recorded as the angulation of the tooth. This means that the smaller the angle, the more mesial the angulation.

Because there were no previously published data regarding the distribution of the angulations of the second premolar and the second molar, the data from the study were used to determine the distribution of the angles.
For each data set, the data were divided into 3 groups: mesially angulated, upright, and distally angulated. If required, data were transformed to achieve a normal distribution. The limits of the upright group were the mean ± 1 SD. This meant that the upright group consisted of the central 68%; the distally angulated group, 16%; and the mesially angulated group, 16%.
The presence of a crypt or an initial calcification of the third molar was taken as development. If none of these signs was present, it was determined that there was no third molar development at this stage.
Assessment of space closure was binary: ie, space closed or space present (unsuccessful space closure) between the mesial aspect of the second molar and the distal aspect of the second premolar. The presence of a visible contact between the second molar and the second premolar with no significant vertical or transverse discrepancy at the contact was considered a success. This was determined clinically through patient callbacks and recruitment from outpatient clinics, or from study models and radiographic records if orthodontic treatment had commenced. If there was any significant chipping or distortion of the study models or radiographic distortion, these data were excluded from the study.
For dental age, bifurcation development stage of the second molar, angulations of the second premolar and the second molar, and presence or absence of the third molar, all 4 quadrants of the same 10 orthopantomograms were assessed 2 weeks apart. For dental age, acceptable reliability for bifurcation development stage of the second molar was taken as a proxy, since the method used for both of these variables was the same. For the dependent variable (space closure), data were only used from subjects who had study models, photographs, or radiographs to prevent the need for repeat visits.
For numeric variables (angulations of the second premolar and the second molar), paired t tests and Lin’s concordance correlation coefficients were used; for categorical variables (bifurcation development stage of the second molar, presence/absence of the third molar, and space closure), kappa and weighted kappa scores were used as appropriate.
Measurements of angles and detecting the presence of a developing third molar were considered within the scope of the day-to-day practice of the primary researcher (S.P.) and therefore calibration to a gold standard was not required. Measurements of second molar stage by the primary researcher were calibrated to a gold standard clinician who had undertaken doctorate-level research regarding dental aging and was therefore competent in assessing the classification of Demirjian et al on orthopantomograms for this age group. Because this was a categorical variable, the Cohen weighted kappa test was used to assess adequate calibration of the primary researcher.
Statistical analysis
SPSS (version 21; IBM, Armonk, NY) and STATA (StataCorp) statistical packages were used for initial data analysis. All patient identifiable data were removed. Each participant was allocated a study number known only to the primary researcher, and this number was used throughout the study.
As data were collected from up to 4 sources, it was important to ensure that there were no significant differences between these groups. The chi-square test was used to ensure that the outcome frequencies were not different to allow the data to be combined.
The distributions of the angulations of the maxillary and mandibular second premolars and second molars were assessed for normality based on skewness and kurtosis. Previous literature has described skewness of near zero and kurtosis less than 1 as acceptable for normality.
As data were collected from up to 4 quadrants in each participant, multilevel analysis was undertaken to account for any clustering effects using MLwiN software (version 2.1; Centre for Multilevel Modelling, University of Bristol, Bristol, United Kingdom). The analysis worked at 2 levels: the level of the patients (dental age) and the level of the quadrants (bifurcation development stage of the second molar, angulations of the second premolar and second molar, and presence or absence of the third molar).
A generalized mixed multilevel model construction was used including all variables and data was entered into the MLwiN software. Any nonsignificant variables ( P >0.05) were removed from the model, and the model was rerun. The resultant model was then tested against the data set to determine the goodness of fit. Given the nature of in-vivo models, a goodness of fit of 80% or greater was considered a good fit. A multilevel model was used to allow for multiple observations (up to 4 quadrants) in the same patient.
Results
A total of 94 patients were included in the initial part of the study; however, 13 patients were excluded (orthodontic treatment, 4; noninterceptive extraction, 4; medical conditions, 2; no preextraction orthopantomogram, 2; and primary failure of eruption, 1). Seven quadrants in the remaining 81 patients were also excluded (ankylosis of primary teeth; impacted second premolars; developmental absence of second premolars, 2 each; delayed eruption of the second molar, 1). This left 148 maxillary and 153 mandibular teeth. Comparisons of the outcome data between the 4 sources of data for maxillary and mandibular molars showed no significant differences ( P = 0.79 and P = 0.28, respectively). We therefore assumed that attendance at a review clinic or commencement of orthodontic treatment was not affected by the presence or absence of a first molar space for this sample of patients.
Reliability testing for the explanatory and dependent variables showed substantial agreement ( Table II ). The results for the numeric data are outlined in Table III . For categorical variables, intraoperator reliability values ranged from 0.8337 to 1.000 (almost perfect to perfect). Calibration for bifurcation development stage of the second molar achieved kappa values of 0.8529 and 1.000 for the mandibular and maxillary arches, respectively.
| Tooth | 95% limits of agreement | P value from paired t test | Lin’s CCC | 95% CI of Lin’s CCC | Agreement |
|---|---|---|---|---|---|
| Angulation of maxillary premolar | −3.457 to 3.457 | 1.000 | 0.984 | 0.933-0.995 | Substantial agreement |
| Angulation of mandibular premolar | −3.106 to 3.506 | 0.7163 | 0.988 | 0.954-0.997 | Substantial agreement |
| Angulation of maxillary molar | −4.175 to 3.975 | 0.8825 | 0.981 | 0.928-0.995 | Substantial agreement |
| Angulation of mandibular molar | −3.698 to 4.098 | 0.7577 | 0.971 | 0.891-0.993 | Substantial agreement |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


