The radial forearm fasciocutaneous flap was first described by Yang and colleagues in the Chinese literature in 1981 and was coined the “Chinese flap.” It later became popularized as the “workhorse” for head and neck reconstruction by Soutar and co-workers in the 1980s because of its reliability and flexibility in design.
Indications
The thin and pliable skin of the volar aspect of the forearm, as well as its rich vascularity and long pedicle, has made it a nearly ideal donor site for reconstruction of defects in the head and neck and for oral defects. It has been reported in the literature for reconstruction of defects in the floor of the mouth, tongue, buccal mucosa, hard palate, soft palate, skull base, pharynx, larynx, lips, orbit, and skin. It is most ideal for the reconstruction of oral defects requiring thin, mobile tissue, such as in the floor of the mouth, tongue, and soft palate. Based on the radial artery, venae comitantes, and cephalic vein, the flap can be designed to include bone (partial-thickness radius), tendon (palmaris longus), muscle (brachioradialis), and nerve, as well as the skin and fascia. Nearly the entire skin of the forearm (from the flexor crease of the wrist to the antecubital fossa and nearly the entire circumference, except for a small strip on the ulnar aspect of the forearm) can be raised with the flap. The shape and overall dimensions can be tailored to the clinical situation. Bilobed, dual cutaneous paddle, fascia only, and folded and tubed flaps have been designed and successfully used for different reconstructive needs.
Anatomy
The hand and lower part of the arm receive their blood supply from the radial and ulnar branches of the brachial artery. The radial artery terminates in the deep palmar arch and the ulnar artery in the superficial palmar arch. Because harvesting of the radial forearm flap requires complete disruption of the radial artery, the hand and digits will be totally reliant on the ulnar artery for their blood supply. The blood supply to the third, fourth, and fifth digits is normally provided by the ulnar artery, so perfusion to the thumb and index finger is at greatest risk when harvesting this flap. For ischemia of the thumb or index finger to occur, two anatomic variations must be present. First, the superficial palmar arch must lack branches to the thumb and index finger. Second, the superficial and deep palmar arches must completely lack communicating branches. In a cadaver study, Coleman and Anson found that the superficial arch supplied all four fingers and the thumb in 77.3% of cases; however, a combination of the two arterial anomalies that would put the thumb and index finger at risk for ischemia was present in 12% of specimens. An aberrant radial artery and aberrant courses of the radial artery have also been reported and may lead to inaccurate results on Allen test. Anomalies of the ulnar artery have also been reported. The skin of the forearm is supplied by septocutaneous and musculocutaneous perforators arising from the radial, ulnar, anterior, and posterior interosseous arteries. The lateral intermuscular septum separates the brachioradialis and flexor carpi radialis muscles in the forearm. Within the lateral intermuscular septum runs the radial artery and its two venae comitantes, and it gives off most of the fascial branches to the skin of the forearm. The radial artery also sends branches to the muscles of the flexor compartment, the palmaris longus tendon, and the radial nerve. Because the lateral intermuscular septum is attached to the distal end of the radius, it also supplies branches to the periosteum, thus giving the option of harvesting a segment of vascularized bone. The length of the arterial pedicle is limited by the recurrent radial artery, the first major branch of the radial artery after it arises from the brachial artery. Venous drainage for the radial forearm flap is via the deeper paired venae comitantes that run with the radial artery in the intermuscular septum and from larger superficial veins, such as the cephalic vein. The veins that accompany the fascial branches of the radial artery to the skin of the forearm drain via the paired venae comitantes. There are multiple communications between the venae comitantes and the superficial veins of the forearm, thus allowing either of these venous systems to be used for the venous anastomosis. Unlike the arterial pedicle, the cephalic vein may be harvested along its entire course to its junction with the subclavian vein. Cutaneous innervation of the forearm is derived from the medial, lateral, and posterior antebrachial cutaneous nerves. The lateral antebrachial cutaneous nerve is the main sensory nerve to the harvested forearm skin and travels with the cephalic vein in the upper part of the forearm. The radial nerve is a mixed motor and sensory nerve. It provides motor innervation for the majority of the muscles of the extensor compartment, as well as the abductor pollicis longus and brevis. It provides sensory innervation for portions of the upper part of the arm and the dorsum of the forearm via the posterior antebrachial cutaneous nerve. The superficial branch of the radial nerve encountered in the wrist during flap harvest provides sensation to the dorsum of the hand, the thumb, and the index and middle fingers.
Anatomy
The hand and lower part of the arm receive their blood supply from the radial and ulnar branches of the brachial artery. The radial artery terminates in the deep palmar arch and the ulnar artery in the superficial palmar arch. Because harvesting of the radial forearm flap requires complete disruption of the radial artery, the hand and digits will be totally reliant on the ulnar artery for their blood supply. The blood supply to the third, fourth, and fifth digits is normally provided by the ulnar artery, so perfusion to the thumb and index finger is at greatest risk when harvesting this flap. For ischemia of the thumb or index finger to occur, two anatomic variations must be present. First, the superficial palmar arch must lack branches to the thumb and index finger. Second, the superficial and deep palmar arches must completely lack communicating branches. In a cadaver study, Coleman and Anson found that the superficial arch supplied all four fingers and the thumb in 77.3% of cases; however, a combination of the two arterial anomalies that would put the thumb and index finger at risk for ischemia was present in 12% of specimens. An aberrant radial artery and aberrant courses of the radial artery have also been reported and may lead to inaccurate results on Allen test. Anomalies of the ulnar artery have also been reported. The skin of the forearm is supplied by septocutaneous and musculocutaneous perforators arising from the radial, ulnar, anterior, and posterior interosseous arteries. The lateral intermuscular septum separates the brachioradialis and flexor carpi radialis muscles in the forearm. Within the lateral intermuscular septum runs the radial artery and its two venae comitantes, and it gives off most of the fascial branches to the skin of the forearm. The radial artery also sends branches to the muscles of the flexor compartment, the palmaris longus tendon, and the radial nerve. Because the lateral intermuscular septum is attached to the distal end of the radius, it also supplies branches to the periosteum, thus giving the option of harvesting a segment of vascularized bone. The length of the arterial pedicle is limited by the recurrent radial artery, the first major branch of the radial artery after it arises from the brachial artery. Venous drainage for the radial forearm flap is via the deeper paired venae comitantes that run with the radial artery in the intermuscular septum and from larger superficial veins, such as the cephalic vein. The veins that accompany the fascial branches of the radial artery to the skin of the forearm drain via the paired venae comitantes. There are multiple communications between the venae comitantes and the superficial veins of the forearm, thus allowing either of these venous systems to be used for the venous anastomosis. Unlike the arterial pedicle, the cephalic vein may be harvested along its entire course to its junction with the subclavian vein. Cutaneous innervation of the forearm is derived from the medial, lateral, and posterior antebrachial cutaneous nerves. The lateral antebrachial cutaneous nerve is the main sensory nerve to the harvested forearm skin and travels with the cephalic vein in the upper part of the forearm. The radial nerve is a mixed motor and sensory nerve. It provides motor innervation for the majority of the muscles of the extensor compartment, as well as the abductor pollicis longus and brevis. It provides sensory innervation for portions of the upper part of the arm and the dorsum of the forearm via the posterior antebrachial cutaneous nerve. The superficial branch of the radial nerve encountered in the wrist during flap harvest provides sensation to the dorsum of the hand, the thumb, and the index and middle fingers.
Work-Up/Diagnostic Tests and Imaging
As with any presurgical evaluation, a thorough history and physical examination should be performed, including elicitation of the presence of any co-morbid disease states. If applicable, a head and neck cancer work-up should include a complete blood count; comprehensive metabolic panel, including liver function tests; prothrombin time, partial thromboplastin time, and international normalized ratio; and chest radiograph, applicable computed tomography scans, stereolithographic models, and a Panorex radiograph. Along with preoperative imaging, the physical examination should evaluate for the estimated size of the defect, the location of the lesion, and the tissues to be resected (skin, mucosa, muscle, bone, etc.) to aid in flap selection. Hypercoagulable states are the only true contraindications to microvascular free tissue transfer. This includes diseases such as polycythemia, thrombocytosis, and possibly sickle cell anemia ( Box 69-1 ). Patients taking antiestrogen medications and hormone therapy such as tamoxifen for breast cancer should have the use of these drugs discontinued before surgery because of their known thrombogenic activity. For similar reasons, as well as decreased flap perfusion and impaired wound healing, smokers should be encouraged to stop smoking at least 1 week before surgery. The history and physical examination should also evaluate the patient for prior trauma to the forearm and previous indwelling radial artery catheters. The Allen test is the most important preoperative evaluation to determine the adequacy of circulation to the hand via the ulnar artery. The Allen test is performed by simultaneously occluding the radial and ulnar arteries while the hand is alternately opened and closed, thus causing the hand to become pale from mechanical exsanguination. The hand is then opened to a relaxed position before ceasing compression of the ulnar artery. The fingers should not be held in a hyperextended position because this can cause them to remain pale and yield a false-positive result. Release of the ulnar artery should result in a blush or reperfusion of the hand within 15 to 20 seconds. Special attention should be paid to the thumb and index finger. With a result beyond 15 to 20 seconds, a radial forearm flap should not be performed. In dark-skinned individuals in whom it is difficult to visualize the blush or reperfusion, it is often helpful to evaluate the nail bed instead by compressing and releasing the fingernail. Sometimes it is also helpful to apply a pulse oximeter to the thumb to assess waveform changes and alterations in oxygen saturation when the radial and ulnar arteries are occluded and when the ulnar artery is released. An accurate Allen test result is necessary for avoiding potential ischemic complications after flap harvest. If the result of the Allen test is equivocal or difficult to interpret, radial artery mapping can objectively determine the pattern of flow and reversal of flow following occlusion of the radial artery.
Inherited
- •
Antithrombin III deficiency
- •
Protein C deficiency
- •
Protein S deficiency
- •
Activated protein C resistance
- •
Factor V Leiden
- •
Dysfibrinogenemia
- •
Plasminogen activator deficiency
- •
Plasminogen deficiency
- •
Factor XII deficiency
- •
Polycythemia
- •
Thrombocytosis
- •
Sickle cell anemia
- •
Heparin cofactor II deficiency
Acquired
- •
Prolonged immobilization
- •
Pregnancy
- •
Surgery/trauma
- •
Oral contraceptives/antiestrogens
- •
Homocystinuria
- •
Vitamin K deficiency
- •
Disseminated intravascular coagulation
- •
Smoking
- •
Nephrotic syndrome
- •
l -Asparaginase
- •
Diabetes mellitus
- •
Hyperlipidemia
- •
Malignancy
- •
Lupus anticoagulant
- •
Anticardiolipin antibody
Treatment and Reconstructive Goals
The treatment and reconstructive goals of the radial forearm flap include provision of soft tissue closure and replacement of resected oral cavity soft tissue, along with restoration of adequate function (e.g., speech, mastication, oral continence) and cosmesis to enable the patient to enjoy a reasonable quality of life. Foremost of the advantages of microvascular free tissue transfer is the ability to tailor the donor flap to the specific needs of the ablative site. As mentioned previously, the thin pliable skin of the radial forearm fasciocutaneous flap makes it ideal for the reconstruction of partial defects of the tongue, floor of the mouth, and soft palate. Flap design and orientation should be thoroughly thought out and performed with care because the three-dimensional nature of oral cavity reconstruction can be complex. For example, soft palate reconstruction with the radial forearm flap may require that the skin paddle be folded for adequate reconstruction, thus making positioning and orientation of the vascular pedicle of paramount importance.
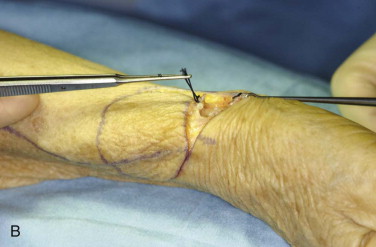
Technique ( Fig. 69-1 )
Once the design of the skin paddle is confirmed and marked out, the arm is exsanguinated with an Esmarch bandage and a tourniquet inflated to 250 mm Hg. Flap elevation is begun at the distal-most aspect of the skin paddle. An incision through skin, subcutaneous fat, and fascia allows identification of the distal radial artery and cephalic vein, which are ligated and transected. The superficial branches of the radial nerve will also be encountered at this time and may be preserved or sacrificed depending on the surgeon’s preference. The longitudinal borders of the skin paddle can now be incised through skin and subcutaneous tissue down through the fascia of the brachioradialis muscle radially and the flexor muscles on the ulnar side. This dissection continues in the subfascial plane to the lateral intermuscular septum between the brachioradialis and flexor carpi radialis. Care must be taken to leave a thin film of paratenon on the tendons of the wrist flexors or wound complications as a result of skin graft failure will be a problem. At this point the proximal portion of the skin paddle can be incised. Care must be taken to avoid injury to the cephalic vein as it emerges from the flap in the subcutaneous fat. A linear incision is then made from the proximal portion of the skin paddle to the antecubital fossa to facilitate dissection of the vascular pedicle from between the brachioradialis and flexor carpi radialis. This incision is then undermined in the subcutaneous plane laterally and medially. Completion of dissection of the cephalic vein can be performed at this stage to the appropriate length and in a circumferential fashion. Finally, the flap can be elevated in a distal to proximal direction to carefully dissect the radial artery and its venae comitantes. Vascular clips will be necessary to control the numerous branches to the surrounding musculature and radial bone. The fascia of the brachioradialis will need to be incised along its length to facilitate proximal dissection of the radial artery. The proximal extent of this dissection is limited by the radial recurrent artery near the antecubital fossa. Once the dissection is complete, the tourniquet is deflated and the flap reperfused for a period of at least 20 minutes. During this time, hemostasis can be achieved with cautery and hemoclips, and final preparation of the recipient site can be performed. After the flap has been allowed to reperfuse, the flap can be harvested by using hemoclips at the desired pedicle length. A suction drain is placed, and the wound is closed in layers with absorbable suture in the deep tissue to reapproximate the divided fascia, as well as in the subdermal layer. Primary closure of the proximal linear incision is easily achieved and may also be possible for the area of the skin paddle. However, the skin paddle area usually requires coverage with a skin graft to avoid excessive tension. Either a split- or full-thickness skin graft may be used and inset with resorbable suture. The graft should be perforated to allow seepage of fluid during healing. This graft should be compressed to the recipient bed with petrolatum gauze, gauze, and cast padding and supported by a plaster splint fabricated to the volar aspect of the lower part of the arm and hand while keeping the wrist, hand, and fingers moderately extended. The splint should be left in place for 7 days to prevent sheer forces on the skin graft. Before placing the final dressing with an elastic wrap, perfusion to the index finger and thumb should be verified by checking capillary refill. The flap should be inset and the microvascular anastomosis carried out promptly to minimize ischemia time. The radial artery is usually a good size match to many recipient arteries in the head and neck, including the facial, superior thyroid, and transverse cervical arteries. The cephalic vein also has excellent caliber and can be matched to the external jugular or facial veins. Thus, this flap has been described as a “macro-microvascular flap.” The decision to use both the cephalic vein and the venae comitantes should be made on a case-by-case basis. Although the flap is well known to survive with drainage from either the superficial or deep venous systems, many surgeons perform more than one venous anastomosis when adequate recipient veins are present. The superficial veins are usually chosen over the venae comitantes when only one venous anastomosis is to be performed because of their larger caliber and thicker vessel walls.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses