MaxilloMandibular Defects
The primary objective of prosthetic rehabilitation is to restore and improve speech and swallowing function. Esthetic considerations are equally important after tumor ablation when structures that lend support to facial projection and symmetry are extirpated in the surgery. The goals of reconstruction may vary in different patients as a result of the need to achieve a balance between the components of the defect, co-morbid conditions affecting surgical reconstruction, and patient motivation. Contemporary management of patients with head and neck cancer integrates surgical reconstructive techniques with prosthetic rehabilitation to optimize function and esthetics. Microvascular free tissue transfer for surgical reconstruction has been revolutionary in addressing the functional deficits present after ablative surgery of large tumors. The biology of the disease and the wound-healing properties of the recipient site after previous therapy are taken into account to determine a plan for reconstruction. If bone is to be part of the reconstructive effort, a method of fixation to ensure flap stability is needed until bony union takes place. Major advancements in surgical reconstructive techniques and new approaches to maxillomandibular defects have effectively provided a more conventional setting for prosthetic reconstruction of the dentoalveolar arch and surrounding structures. Composite free flaps from the fibula, iliac crest, and scapula regions are designed and harvested to address loss of tissue volume for restoration of mandibular continuity and to separate the oral from the sinonasal cavity.
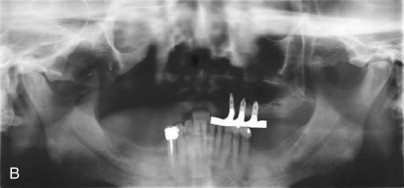
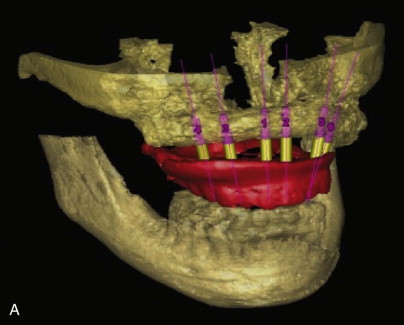
Preservation of tongue motion and restoration of tongue volume are critical in achieving a favorable functional outcome if the tumor extends to the tongue or floor of the mouth. Soft tissue defects involving the overlying skin or mucosal defects involving the lip or cheek, as well as any sensory and motor nerve deficits, will define which reconstructive option is best for functional recovery. Vascularized bone free flaps (VBFFs) from the fibula or iliac crest provide good to excellent bone volume and the quality required by the underlying bone for osseointegration and the application of prosthetics. VBFFs will either restore discontinuity of the mandible or re-establish a stable base for the maxilla. Bone harvested from a distant donor site with its own blood supply presents additional strategies for osseointegration and prosthetic rehabilitation when reconstructing defects caused by the ablative treatment of benign and malignant tumors. Among such strategies is use of the vascular bed for osseointegration before radiation therapy. Placement of implants in the immediate surgical setting will shorten the overall treatment time until definitive prosthetic restoration can be accomplished. Once the bone is secured to the reconstruction plate and anastomosis of the recipient vessels is completed, implant placement is performed. After primary implant placement, the restorative team must allow 12 to 16 weeks for osseointegration and undisturbed healing. When a patient has completed radiation therapy after reconstruction and primary implant placement, the fixtures are uncovered once the soft tissue reaction has subsided. Soft tissue modifications can also be performed at this time, such as flap debulking or vestibuloplasty procedures. A surgical stent can be used and screwed into the implants for healing purposes before definitive prosthetic rehabilitation. Primary implant placement is helpful in developing a comprehensive approach to ablative surgery, subsequent reconstruction, and prosthodontic rehabilitation with adjunctive radiation therapy. This also holds true for placement of implants into native bone at the time of tumor resection to optimize function without surgical reconstructive procedures. This strategy circumvents the need for treatment with hyperbaric oxygen in patients requiring radiation therapy. In addition, primary implant placement will minimize time with an unstable prosthesis and compromised function in an edentulous patient, especially edentulous maxillectomy patients ( Fig. 73-1 ). As the defect enlarges, side effects such as hypernasal speech and nasal regurgitation of food are frequently encountered with an unstable prosthesis.


Prosthetic Design Considerations
The decision for fixed versus removable prosthetic restorations is dependent on clinical factors such as the availability of bone, the number and position of implants to assist or support restorations, maintenance of hygiene, and manual dexterity. Palatal obturators for maxillectomy patients or palatal augmentation prostheses to restore lingual-palatal contact for glossectomy patients are removable. If tumor surveillance is also a consideration, a removable prosthesis is indicated.
In addition to these clinical factors, other considerations such as comfort and psychosocial implications affect prosthetic design. When addressing reconstruction of the dental arch with osseointegrated prostheses, our preference is to provide patients with a fixed implant-supported restoration. In patients in whom the remaining arch is edentulous and lateral mandibular reconstruction is being performed, the implants should be placed in the anterior native mandible. This is an ideal location for placement of fixtures in patients undergoing lateral jaw resection for posterior alveolar, floor of the mouth/lateral tongue, or tonsillar primary tumors because this area is usually spared during radiation therapy. Placement of a minimum of four or five implants with the greatest anterior-posterior spread possible to minimize cantilever forces on the distal extension of the prosthesis and posterior placement of the distal implant on the contralateral side are potentially limited by the mental nerve and foramina. This landmark must be identified and care taken to avoid injury to the mental nerve.
These restorations are retained by screws when the prosthesis is retrievable as opposed to a cemented restoration. This design consideration is an important factor in cases in which direct visualization of tissue is necessary. There are also issues of maintenance. Composite free flaps can use muscle for lining the oral cavity, and on occasion, peri-implant mucosa requires surgical débridement of hyperplastic inflammatory tissue. In addition, because of a lack of innervation of the free flap, muscle will atrophy over time and require secondary impressions and relining procedures to prevent food debris from collecting under the prosthesis.
Managing the Height of the Fibula
The advantages of the fibula free flap have made it a “workhorse” flap for reconstruction of mandibular discontinuity defects. The length of bone that can be harvested is excellent for reconstruction of the inferior border of the mandible and restoration of symmetry to the lower third of the face. The low donor site morbidity and the ability of a second surgical team to harvest the fibula free flap simultaneously also contribute to its favorable characteristics. Additionally, there is good to excellent bone stock for osseointegration. Because of the bicortical nature of the fibula, it possesses approximately 12 mm of bone height for endosteal implants. Use of the fibula versus the iliac crest can present a geometric challenge for prosthetic reconstruction. As mentioned, the fibula is best positioned so that it reproduces the contours of the outline of the lower third of the face. This may lead to an intraoral discrepancy in height with the native mandible. Additionally, the dental arch lies lingually above the reconstruction so that implants can be positioned facial to the dental arch and the occlusal plane. There are surgical techniques to overcome this discrepancy in height. One is to position the fibula more superiorly and use the reconstruction plating system to reproduce the contours of the inferior border. Another is the “double-barrel” technique in which the fibula is folded to increase the height of the fibula free flap. We have found that the height discrepancy can also be addressed through prosthetic design. The use of a bar framework designed to sit lingual to the implants can overcome the discrepancy in height and facial position. An implant-assisted removable overdenture can be constructed in a manner that promotes lip and cheek competence. The overdenture will have small fenestrations at the base of the facial flange to overcome the facial position of the implants. Resistance to cantilever forces is possible as a result of the bicortical nature of the fibula ( Fig. 73-2 ).




These concepts can also be applied to a screw-retained fixed restoration in a dentate patient by using a cast mesostructure-superstructure design. The mesostructure is milled so that the support for the implant is centralized over the mandibular neo-ridge and the corresponding superstructure acts as a fixed partial denture that is set with screws into the mesostructure ( Fig. 73-3 ).






The contours of the mandibular prosthesis can provide support to the lower lip for restoration of projection and symmetry of the mouth. The loss of motor function from the marginal mandibular branch of the facial nerve as a result of ablative procedures can be ameliorated with this means of lip support.
Palatomaxillary Reconstruction
Surgical reconstruction of palatomaxillary defects has evolved over the past decade and emerged as a viable option for patients undergoing resection of large tumors. Although surgical closure of large palatomaxillary defects can also provide closure of the oral cavity, problems are encountered when large soft tissue flaps occupy the functional space over the tongue and are not amenable to dental reconstruction. The use of VBFFs to reconstruct large palatomaxillary defects provides surgical closure and restores the stable base of the hard palate above the alveolar process. As with mandibular reconstruction, it allows the placement of dental implants for prosthetic rehabilitation. This approach optimizes function and addresses the shortcomings of an obturator. Even though an obturator can be used for successful restoration and remains a standard for prosthetic rehabilitation, as defects get larger, nasal escape can compromise speech and swallowing. Because these side effects also have implications for comfort and psychosocial interaction, surgical reconstruction of palatomaxillary defects is an excellent alternative approach to optimal functional rehabilitation.
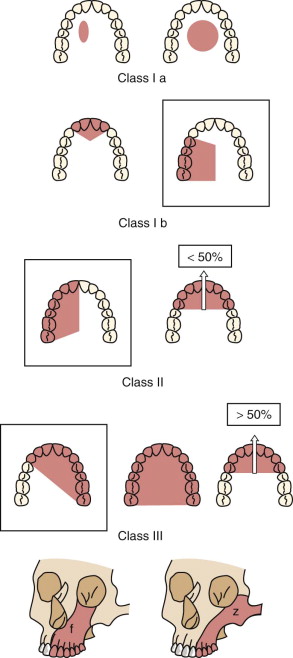
Our classification system essentially addresses the size and location of palatomaxillary defects and considers the biomechanical properties that contribute to prosthetic instability and compromised function. The remaining dental arch and palatal shelf, as well as other components involved in anatomic retention, such as scar band formation with a split-thickness skin graft (STSG), have been useful prognostic factors in treatment algorithms and, in particular, the indications for VBFF reconstruction. As the remaining dental arch shortens and the palatal surface decreases, prosthetic instability is more likely to occur ( Fig. 73-4 ). Three categories of defects describe the horizontal nature of palatal defects. If an orbital defect is accompanied by a maxillectomy defect, surgical reconstruction should address the separation of the combined defects separately. Maxillectomy defects have the subscripts “o” for orbital floor and “z” for zygoma to address these areas in the restorative decision-making process. A class I defect is a subtotal maxillectomy defect in which there is loss of the posterior alveolus to the canine tooth. This type of defect has sufficient remaining retentive and stabilizing components. Class I defects are therefore amenable to either prosthetic obturation or surgical reconstruction with a radial forearm free flap or palatal island flap. The remaining dental arch and palate are used to provide restoration of the dental arch with a tissue-borne prosthesis. Implants in the remaining native maxilla are necessary if the dentition is hopeless or the patient is edentulous. A class II defect is a hemimaxillectomy defect extending to the midline. In class II defects, the increased size of the defect and loss of the ipsilateral canine and molar dentition make the use of a VBFF reconstruction important if the surgeon decides to not use a prosthetic obturator. A class III defect extends beyond the midline. The defect involves both canines and the ipsilateral molar dentition and results in a bilateral defect with a poor prosthodontic prognosis ( Fig. 73-5 ). As the maxillectomy defect increases in size and the remaining dentition and palate decreases in size, a VBFF is preferred over a fasciocutaneous free flap. Osseointegration and prosthodontic rehabilitation can restore dentoalveolar structures and occlusal contact to optimize speech and swallowing functions. Once again, a fixed-implant restoration is the authors’ preference in this situation. Treatment planning involves more implants rather than a minimum number for support of a restoration. In the event of implant failure, prosthetic success can still be achieved with a shorter restoration of the dental arch or an implant-assisted overdenture without added time or surgery.


Prosthetic Design Considerations
The decision for fixed versus removable prosthetic restorations is dependent on clinical factors such as the availability of bone, the number and position of implants to assist or support restorations, maintenance of hygiene, and manual dexterity. Palatal obturators for maxillectomy patients or palatal augmentation prostheses to restore lingual-palatal contact for glossectomy patients are removable. If tumor surveillance is also a consideration, a removable prosthesis is indicated.
In addition to these clinical factors, other considerations such as comfort and psychosocial implications affect prosthetic design. When addressing reconstruction of the dental arch with osseointegrated prostheses, our preference is to provide patients with a fixed implant-supported restoration. In patients in whom the remaining arch is edentulous and lateral mandibular reconstruction is being performed, the implants should be placed in the anterior native mandible. This is an ideal location for placement of fixtures in patients undergoing lateral jaw resection for posterior alveolar, floor of the mouth/lateral tongue, or tonsillar primary tumors because this area is usually spared during radiation therapy. Placement of a minimum of four or five implants with the greatest anterior-posterior spread possible to minimize cantilever forces on the distal extension of the prosthesis and posterior placement of the distal implant on the contralateral side are potentially limited by the mental nerve and foramina. This landmark must be identified and care taken to avoid injury to the mental nerve.
These restorations are retained by screws when the prosthesis is retrievable as opposed to a cemented restoration. This design consideration is an important factor in cases in which direct visualization of tissue is necessary. There are also issues of maintenance. Composite free flaps can use muscle for lining the oral cavity, and on occasion, peri-implant mucosa requires surgical débridement of hyperplastic inflammatory tissue. In addition, because of a lack of innervation of the free flap, muscle will atrophy over time and require secondary impressions and relining procedures to prevent food debris from collecting under the prosthesis.
Managing the Height of the Fibula
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


