Abutment Casting
Implant Analogue
Abutment Analogue
TSD4, TSD44, DA4
IA 99, IA DTI
IA4
PA4
TSD5, TSD55, DA5
IA 99, IA DTI
IA5
PA5
TSD99, DA99
IA 99
IA5
PA5
It is also possible, however, to use original abutments and implant analogues in the laboratory. The latter approach is recommended specifically if the abutments are to be selected by the technician (see Sect. 11.2), in which case the longest possible abutment is used for impression-taking. The abutment is then removed, screwed against an analogue and embedded in plaster. After selecting and mounting an appropriate analogue, the dentist can fabricate the restorative work on this model. The technician should invariably use an IA99 implant analogue in this approach, so that the abutment can always be switched to a TSD99 design if considered appropriate.
11.1.2 Collaboration with the Laboratory
Once the framework has been fabricated, it is tried in. Large-span bridges made from CoCrMo can hardly ever be cast from a single workpiece due to the structural deformations associated with casting. The workpieces are either separated after modelling, or they are separately modelled in the first place. If the model is considered trustworthy, then the workpieces can be assembled right in the laboratory. Otherwise, they are separately inserted and bonded together in the patient’s mouth with a fast-curing acrylic resin (e.g. Pattern Resin). Great care must be exercised in assembling the workpieces on the soldered model in order to avoid corrosive layers. Less expensive alternatives to laser soldering would include microplasma soldering or even larger TIC systems, which do not require the use of a solder. While microplasma systems are more expensive than TIC systems, they include the option of subsequent “remodelling” by addition of metal.
The definitive bite registration can usually be performed simultaneously with the framework try-in. If the postoperative mucosal swelling has already resolved by that time, an over-impression with alginate or silicone should be taken with the definitively tried-in framework in place. The relations between the bridge and the mucosa will be displayed better in the resulting model. Early gap formation is avoided, and the bridges thus fabricated will easily remain usable in the medium and long term.
Implants have been selected correctly if the threaded shaft portion comes to be located at least 1 mm above the mucosa, such that the transitional zone between fixture and abutment is accessible with oral hygiene instruments. This requirement has implications for the work in the dental laboratory:
-
The metal shoulder is overcontoured on the vestibular aspect of the aesthetic zone. A punctiform contact of the metal/ceramics with the mucosa is established. At the same time, the space between the threaded pin and the vestibular apron must be accessible for brushing and flossing.
-
The zone where the abutment meets the bridge framework is within the range of brushing and flossing. Therefore, the precise fit of the bridge is much less of a requirement than with screw implants or natural teeth. Also, the gap between the abutment and the bridge can be reliably closed in a permanent manner with the cements available today. The job of the dental technician is greatly facilitated by these advantages, which are particularly relevant in the mandible. After all, perfect congruence between the abutments and the framework is virtually unattainable in complete mandibular bridges, given the flexion of the jaw bone. Any sharp projecting areas can be easily corrected, rounded and polished.
During the ceramic try-in, functional aspects are evaluated as well as the shade and shape of the bridge. Furthermore, abrasive instruments can be liberally used in this session, which takes place before the last firing step is performed. While smaller “segmental” bridges can often be finished in the laboratory with no need for a metal try-in, the demands on the bite registration are greater in this situation. After all, a balanced muscle activity will not be restored any time soon following the implant procedure if partial edentulism was present for an extended period of time, which is particularly true of cantilever situations. Therefore, even though there may be no evident signs of myoarthropathy, the bite cannot be reliably registered in the postoperative phase.
Temporary cements should be avoided on cases with strategic implant positioning if possible. After all, patients who have grown used to mobile dentures over the years cannot be expected to complain about, or even notice, any debonding of individual abutments. If debonding occurs on several abutments, the remaining bonded abutments will be subjected to increasingly excessive loads, which may give rise to (initially non-bacterial and thus reversible) osteolysis or fractures. In patients with good compliance, BOI restorations can also be cemented temporarily over a longer period, especially if the number of abutments is large and the mastication is balanced. This presupposes that it is ensured that patients will appear at the dental office even between scheduled recalls in the event that the temporarily cemented restoration should loosen. In case that the plane of bite is not ideal of balance is missing, even definitively cemented restorations will loosen regularly (or the perimplant bone will show signs of osteolysis or the implant will break). Refer to Chapter 10 for details about establishing the necessary equilibrium of forces.
All known definitive cements can be used. After the cementing step has been completed, the masticatory function needs to be checked. Occlusal considerations are less important, except that antagonists must be kept in their positions. After all, the treatment objective is to offer functional incorporation of the implant-restoration system. The masticatory function is the main aspect of this goal. As far as occlusal parameters are concerned, it is usually sufficient to establish a small number of bilateral and simultaneous contact points, specifically in the area of the palatal cusps.
Extensive structures have to be followed up closely in accordance with the existing muscle situation, especially in the presence of myoarthropathy and abnormal occlusal relationships. The first follow-up visit is scheduled within the first two to four weeks. If extensive masticatory and occlusal corrections are required at this point, a similar interval is selected until the next visit. If the bite situation has appreciably relaxed and moved towards centric relations, the patient should come back after around 3 months. If the positional and functional relationships have stabilized by that time, the follow-up protocol can be switched to 6-month intervals. Radiographs are obtained semiannually in the first two years. After that, radiographic examinations will only be required if and when problems occur. If the restoration also includes residual tooth structures alongside the BOI implants, radiographs will of course have to be obtained periodically on a long-term basis.
In the presence of advanced ridge resorption or relative malpositioning of the jaws, it is commonly observed that the positions of the implants are at variance with the subsequent position of the prosthetic teeth. This phenomenon is due to the centripetal and centrifugal resorption patterns of the maxilla and mandible, respectively. In other words, the threaded pins in the mandible will always be located in a slightly more vestibular position than desired, while those in the maxilla will be characterized by an overly palatal position. Other configurations are naturally also possible if specific situations in terms of relative jaw widths or occlusal relations are present. First of all, an agreement must be reached with the technician whether the prosthetic structure should be characterized by normal or crossbite occlusal relations. Both approaches are viable, provided that the bulk of the restoration will be located over the supporting polygon of the load-transmitting BOI surfaces. Close collaboration with the laboratory is a sine qua non in this situation, since the technician does not know the position of the basal plates. The greater the distance of the chewing surfaces from the supporting polygon, the greater the number and larger the size of the disks to be inserted.
11.1.3 Types of Overload
Due to their heavily focused load-transmitting surfaces, BOI implants are more susceptible to overloading in the early postoperative phase. We distinguish between four types of prosthetic overloading, which will be discussed in the following paragraphs.
11.1.3.1 Primary Overload
A situation in which the prosthetic structure shows early contacts at one or several implant sites may be defined as primary overload. These situations are addressed by carefully reducing the affected jaw segments with abrasive instruments.
11.1.3.2 Secondary Overload
A situation in which the spatial position of the mandible changes as a result of altered muscle function may be defined as secondary overload. These situations usually occur within the first months after inserting a restoration. Secondary overload situations develop naturally while the masticatory function is undergoing adaptive processes. They are addressed in the same way as primary overload situations by reducing the affected segments or by raising other segments. They are not a result of incorrect treatment but of muscular reactions. The clinician should inform the patient of this eventuality in advance so as to avoid misunderstandings.
Secondary overload situations are caused by short-term interactions between chewing muscles and their neuronal control. They can also develop as a result of changes in the jaw morphology, which is a response to altered functional patterns and the situation of nourishment and drainage of the bone. Secondary overload requires frequent adaptations of the occlusal platform, by far more than one would expect from the experience of work on natural abutments.
11.1.3.3 Tertiary Overload
As a result of ongoing long-term functional adaptations while engrams governing the control of the masticatory and postural muscles are being redefined, the bimaxillary positional relations may undergo substantial changes that require correction even years after insertion. As far as implant-supported restorations are concerned, these situations may be described as tertiary overload situations. They are corrected by reducing the affected areas or, if necessary, by replacing the entire restoration. This worst-case scenario may come to pass if regular dental relations and a normal masticatory function cannot be reestablished by simple abrasive adjustments or if the vertical dimension has been excessively reduced by numerous adjustments.
Once again, this type of situation is not due to treatment errors but is caused by long-term normalization of the masticatory function as well as age-related alterations in jaw morphology.
The extent and the consequences of secondary and tertiary overload situations, as well as the timeframes involved, were not fully appreciated and analysed before dental implantology was included in the therapeutic spectrum (Book et al. 1992). Long-time users of BOI implants have learned how to deal with this type of problems. Novices, on the other hand, must pay close attention to the specific circumstances to avoid treatment failure. TMJs are routinely observed to move up to 5 cm (and sometimes as much as 1 cm) as functional abnormalities resolve. Patients with skeletal Class II relations and greatly altered TMJ morphology typically exhibit greater positional variability. Since BOI implants are the only option for patients with advanced jaw resorption to receive a fixed restoration in a single procedure, the experience of conventional restorative procedures cannot be readily transferred to the BOI concept, and it certainly cannot be transferred without qualifications. We continue to be faced with the problem that many non-authorized experts are unaware of or underestimate the consequences of these adaptation processes, so that their formal opinions are often marred by unfortunate misjudgements.
Nevertheless, these trains of thought are being increasingly pursued by crestal implantologists as well. Interestingly, even the University of Bern, Switzerland, seems to have abandoned the absolute concept of “bite registration” in favour of “bite testing” (Mericse-Stern 2002).
Issues concerning the registration of joint position are beyond the scope of this communication. Extreme jaw resorption is virtually always accompanied by painful or asymptomatic myoarthropathy. Facebow registration is therefore a questionable measure (Carlsson and Magnusson 2000) as its result would just reflect a pathological situation. There is a risk that this pathological situation is perpetuated by transferring these facebow data to the new restoration without getting to the bottom of the problem. Since a symmetrical prosthetic outcome is an essential treatment objective, other techniques including a plane record have proved to be a useful alternative to arbitrary registration (Schöttl 1997). The HIP-mount system developed for this purpose has the advantage that the HIP plane determined in the model can be checked by a plane record with the help of the Head Lines measuring device. Since the model is always mounted in the articulator parallel to the occlusal plane, it is easier for the dental technician to fabricate a horizontally correct restoration, which, in turn, will expedite the adaptation of masticatory function. In our view, the HIP technique enables optimal horizontal adjustment of the masticatory plane. Its users will immediately notice any elongations in the maxilla, and they can easily verify the absolute horizontal plane in a reliable manner. Even this technique cannot, however, change the fact that extensive subtractive adjustments or contralateral crowning of teeth will be necessary in the presence of greatly divergent AFMP angles on both sides of the jaw. Furthermore we always have to consider the vertical and horizontal bone level around teeth, around implants and between teeth, implants and even in edentulous sections of the jaw as highly unstable and adapting to function. The joints show a large range of adaptation to many of the changes, and thus compensatory elongations, the buildup of new trajectories, age- and extraction-related bone loss, changes in chewing force and morphological changes, which are followed by changes in the chewing pattern. Even a “correct” centric registration is bound to change considerably over time, which will lead to overload on teeth and implants. In our experience the changes are greater in cases where the bite is not balanced or constructions are unsymmetrical.
11.1.3.4 Iatrogenic Tertiary Overload
These situations include ill-advised occlusal adjustments, usually made by other dentists who are not sufficiently aware of the problems involved, after ossification of the basal plates has been completed. In contrast to the regular secondary and tertiary overload situations, which evolve gradually, iatrogenic tertiary overload situations occur abruptly and involve an even higher risk of implant fracture. After all, there is not enough time left for the well-ossified BIO implant to react to the problem by way of overload osteolysis.
Iatrogenic overload situations, as the name implies, are to be blamed on incorrect dental treatment. It is only fair to add, however, that patients who wear implant-supported restorations in both jaws will not be able to notice and report any premature contacts as readily as patients with natural dentitions.
In patients who received a first BOI restoration in one jaw, followed by a second BOI restoration in the opposite jaw at a later time, the jaw that was treated first may be subjected to iatrogenic tertiary overloading while the jaw that was treated second may be affected by regular types of primary, secondary or tertiary overload. Cases such as these require meticulous follow-up examinations and functional adjustments by additive and subtractive means.
Incidentally, osteolytic phenomena may remain confined to individual disks of an implant or indeed to specific portions of a disk. With the old double-disk implants that still featured a disk-to-disk distance of 3 mm, the crestal disk used to be more susceptible to osteolysis. In this situation, the dentist must consider removing the disk because there is a risk that the osteolytic area may become infected and that this infection may even spread to the basal disk. As long as the infection remains confined to the crestal disk, the implant as such can be preserved.
Figure 11.1 illustrates how BOI implants work. This specific implant was inserted into the crestal part of the alveolus immediately on extracting tooth 46. In other words, the threaded pin was never surrounded by bone. While the remaining space of the alveolus was filled with newly formed bone due to functional stimulation, the area of the threaded pin remained non-ossified. The picture was taken 5 years after the implant had been inserted and immediately loaded.
Figure 11.2 shows a similar case in which the implant was, however, inserted considerably more deeply.
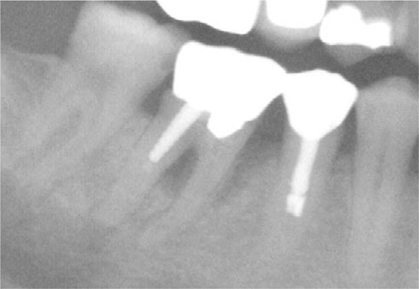
Fig. 11.1.
Situation immediately before tooth 46 was extracted and replaced with an implant in the same session using immediate loading

Fig. 11.2.
Situation at the 6-month follow-up. The extraction area has largely regenerated. A smooth-shafted EDS 10 G10 implant was used
The clinical developments in these examples attest to the fact that a clear-cut line between the initial treatment and the maintenance phase cannot always be drawn. This eventuality must be pointed out to the patient to avoid misunderstandings when he or she is charged for additional dental treatments that may become necessary after the cost ceiling for the initial treatment has been reached. In some patients, notably in those with myoarthropathies, it is downright impossible to draw a line between the initial treatment and the maintenance phase. After all, myoarthropathies are chronic diseases that may require lifelong therapy.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


