Fig. 1.1
Schematic representations of the approximate anatomical coverage provided by different fields of view of a CBCT unit. (a) Small FOV, (b) medium FOV, and (c) large FOV
In almost all units, a smaller FOV scan is acquired using a smaller voxel size, thus yielding images with higher spatial resolution. Furthermore, a smaller FOV also reduces scattered radiation, decreasing image noise and contributing to improved image quality. This is particularly important given that many of the endodontic diagnostic applications require higher resolution, for example, evaluation of the periodontal ligament space and lamina dura. Selection of the appropriate FOV should be made considering not only the anatomic coverage but also the image resolution required for the diagnostic task. For example, in a patient with atypical odontogenic pain, all the teeth in a selected quadrant may need to be imaged to rule out an odontogenic cause for the pain. Such patients may possibly benefit from two adjacent limited FOV scans, rather than a single medium or large FOV scan. In this scenario, the lower image resolution with the medium/large FOV scan is likely to compromise critical evaluation of the apical periodontal structures.
1.2.3.5 Voxel Size
The smallest three-dimensional data unit on a CBCT image volume is the voxel. The voxel size depends on the size of the detector pixels, which in current CBCT systems ranges from 0.07 to 0.4 mm. In general, a CBCT scan acquired with a smaller pixel size produces an image with higher spatial resolution. Nevertheless, the detector pixel size is not the only determinant of image resolution. Several other machine-specific parameters such as CT reconstruction algorithms and image processing “filters” modulate the signal-to-noise ratio and image resolution.
In many CBCT units, the voxel size is predetermined for a specific FOV. Typically, smaller FOVs are imaged using a smaller pixel size. In some CBCT units, the operator can manipulate the pixel size for a given FOV. For these protocols, imaging at a smaller pixel size is accomplished by either increasing the number of basis projections or increasing the radiation exposure factors. Clinicians must be aware that these protocols will deliver a higher patient radiation exposure, compared with the standard protocol.
1.3 CBCT Artifacts
The CBCT imaging process starts by making sequential two-dimensional projections along hundreds of angles around the area of interest. Each projection represents a map of x-ray attenuation by objects along the path of the x-ray beam. Mathematical algorithms are applied to this attenuation data to spatially reconstruct the locations of the structures within the imaged volume. There are several factors that influence the accuracy of the reconstructed data. These include discretization of the imaged object, geometrical projection issues, detector noise, and the assumptions in mathematical modeling. Discrepancies between the reconstructed data and the physical state of the actual object may be evident in the image and are termed artifacts. There are several different artifacts described in CT imaging. These include beam hardening artifacts, photon starvation artifacts, cupping artifacts, and partial volume averaging. Schulze et al. [7] provide an excellent description of the physical basis for and the appearances of these various artifacts.
Beam hardening artifacts are noted around dense bony structures and around radiopaque restorations and endodontic filling materials. Clinicians who use CBCT must be aware of the appearances of such artifacts and not confuse them with pathological changes. For example, metallic restorations will result in dark bands and streaks (Figs. 1.2, 1.3, and 1.4). The dark bands which extend to the region around the restoration and to the crowns of the adjacent teeth may be interpreted as caries. When these bands appear on the crowns or roots of adjacent teeth, they may be misinterpreted as caries or root fractures. Likewise, the region around metallic posts and gutta-percha yields dark bands, which may compromise the ability to detect fractures or resorption of the adjacent root structure.
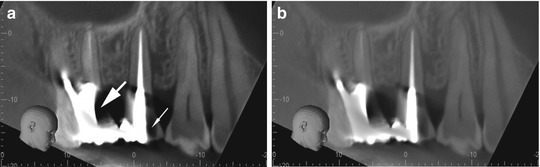
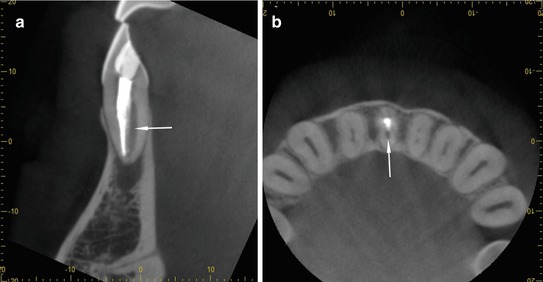
Fig. 1.2
(a) Axial slice demonstrating metallic restorations in the second premolar and first molar teeth. Note the radiating pattern of dark bands and streaks. Note how linear artifacts are evident on the root of the adjacent first premolar. (b) Sagittal CBCT section through the maxillary central incisor. Note the dark zone around the metallic post
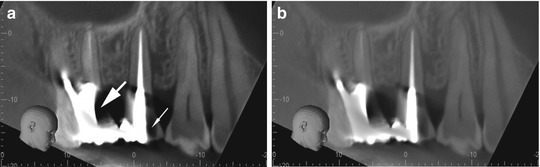
Fig. 1.3
(a) Sagittal slice demonstrating metallic restorations in the second premolar and first molar teeth. Note the dark bands on the molar crown (big arrow) and the crown of the second premolar (small arrow). (b) Same section as in panel A. Note how adjusting the density and contrast allows for better visualization of the crown and root surfaces in the regions of the dark bands, further confirming their artifactual nature
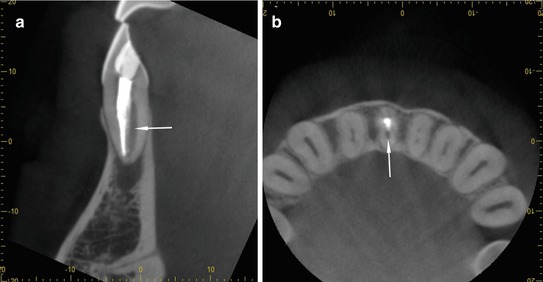
Fig. 1.4
(a) Sagittal and (b) axial slices through the mandibular anterior region. Note the presence of an unfilled canal in the central incisor (arrows). This additional canal should not be confused with artifacts from the radiopaque gutta-percha
1.4 Radiation Dose Considerations
The basic premise of diagnostic radiographic imaging is that the benefits from the examination far outweigh the risks associated with ionizing radiation exposure. The principles of radiation risk and safety that apply to conventional periapical and panoramic radiography also apply to CBCT imaging. CBCT users should be familiar with the doses delivered by various CBCT imaging protocols, the risks associated with radiation exposure in this range, and the methods to minimize patient radiation exposure.
1.4.1 Risks from Diagnostic Radiation
X-rays are ionizing radiations. Interaction of x-ray photons with biological molecules, predominantly water, produce reactive radicals that cause ionization and potential biological damage which may manifest as radiation-induced effects. The effects depend on the specific tissues exposed and the dose and dose rate of radiation. There are two types of radiation-induced effects—deterministic and stochastic.
1.4.1.1 Deterministic Effects
Deterministic effects occur when the radiation absorption in a tissue or organ exceeds a threshold level. This threshold is dependent on the specific tissue or organ that is exposed. When the radiation dose is higher than the threshold level, the effect is induced. Further increasing the radiation dose increases the severity of this effect. Examples of deterministic effects include radiation-induced cataracts, decrease in salivary gland function, osteoradionecrosis, and radiation-induced fibrosis. Radiation doses from dento-maxillofacial radiographic imaging are orders of magnitude lower than the threshold levels for deterministic effects in the various tissues exposed. Thus, the risk of inducing such deterministic effects by maxillofacial imaging is essentially zero.
1.4.1.2 Stochastic Effects
In contrast to deterministic effects, there is no minimum threshold dose for causing stochastic effects. This implies that even low levels of radiation exposure could trigger stochastic effects. The probability of causing stochastic effects decreases with decreasing radiation dose, and this is the basis of dose minimization in diagnostic radiology. Examples of stochastic effects include radiation-induced neoplasia and heritable effects of radiation.
The principal risk from diagnostic maxillofacial CBCT imaging is the risk of radiation-induced neoplasia. The association between radiation exposure and cancer has been firmly established both by animal studies and by studies of human populations that were exposed to ionizing radiation, either intentionally or by accident. These studies have demonstrated some basic concepts that have important implications in radiation safety and protection:
-
There is a latent period between the exposure and the occurrence of cancer, which may vary from a few years to several decades.
-
Certain tissues are more sensitive to the carcinogenic effects of x-radiation. In the craniofacial region these include the thyroid gland, the red bone marrow, the brain, the salivary glands, and the parathyroid glands.
-
Age at the time of exposure is a strong modifier of radiation-induced cancer risk. It is estimated that radiation-induced cancer risks are at least three- to fivefold higher in children [8]. This is attributed to increased organ sensitivity to radiation-induced carcinogenesis and longer life expectancy, which allows time for neoplastic development.
It is currently accepted that ionizing radiation-caused DNA damage is the initial trigger for radiation-induced cancer. Even a single photon can produce radicals to cause DNA damage, and this explains the stochastic nature of radiation-induced neoplasia. The number of radicals produced increases with dose, and thus, the likelihood and extent of radiation-induced DNA damage increases with radiation dose. The current model for estimating radiation-induced cancer risks is based on the linear no-threshold hypothesis (LNT), which assumes that the risk of radiation-induced cancer increases linearly with increasing radiation dose. This hypothesis is based on scientific data that demonstrate such a linear dose response, although at doses typically above 100 milliGray (mGy). The nature of the risk at doses in the order of a few tens of mGy has not been experimentally established. Nevertheless, the assumptions of the LNT model have not been disproven, and thus, regulatory agencies continue to use this model to conservatively estimate risk and develop policy guidelines on radiation exposure to occupationally exposed individuals and members of the public.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


