(1)
Department of Orthodontics, Universidad Intercontinental, Mexico, D.F., Mexico
Abstract
This chapter emphasizes the reasons why lower incisors should generally not be proclined more than 2 mm since this orthodontic movement is associated with problems of health, function, stability, and esthetics. Facial movement of the teeth decreases the buccolingual thickness of the gingival tissue, which results in reduced height (recession) of the free gingival portion. In patients in whom the gingiva covering the labial of the lower incisors is thin and scalloped, orthodontic proclination of the lower incisors may cause not only gingival recession but also dehiscence. Both are examples of health problems associated with proclination of the incisors. An increase in the magnitude of the anterior open bite may occur in open-bite tendency malocclusions if lower incisors are moved labially and sometimes may even result in lip incompetence. These two are examples of functional problems associated with proclination of the incisors. There is evidence that post-retention stability of lower incisor alignment is compromised if the lower incisors were proclined during orthodontic treatment. Additionally, when the lower incisors are moved labially, facial esthetics could be compromised in pleasing facial profiles because as the teeth procline, the lips also move forward, while the chin stays back. An increase in lip protrusion could thus be associated with an undesirable appearance of a decreased chin projection and a diminished definition of the labiomental sulcus. Patient records are shown which illustrate the undesirable effects of lower incisor proclination. The contraindications for incisor proclination are discussed, and the orthodontic procedures recommended by the author to avoid incisor proclination in dentally crowded patients are shown.
2.1 Introduction
Several studies have compared the periodontal health between patients who had orthodontic treatment with individuals who did not have orthodontic treatment.
Slutzkey and Levin [1] evaluated a cohort of 303 healthy patients who had routine dental examinations at a military dental center. They found increased gingival recession in young adults who had undergone orthodontic treatment (on average 4.8 years prior) compared to those who did not have orthodontic treatment. Also the severity and the extent of the recession were significantly correlated with past orthodontic treatment. This study supports the findings of systematic reviews that orthodontic treatment does not improve periodontal health and that it may actually make it worse.
Bollen et al. [2] carried out a systematic review of the relationship between orthodontic treatment and periodontal health. The conclusions were that patients with prior orthodontic treatment had 0.13-mm greater alveolar bone loss than patients without prior orthodontic treatment and that there were 0.23-mm greater pocket depth and 0.03-mm greater recession in subjects with prior orthodontic treatment. The reported small worsening of the periodontal conditions after orthodontic treatment was a generalized mean for the entire dentition. These small, yet significant, differences may be of clinical importance if it is a localized effect (a large worsening around a few teeth) rather than a generalized effect (small worsening around all teeth). This systematic review failed to find a beneficial effect of orthodontic treatment on periodontal health. On the contrary, patients with prior orthodontic care had greater alveolar bone loss, periodontal pocket depth, and gingival recession than individuals who had not received orthodontic treatment. These two studies [1, 2] suggest that orthodontists must be more careful in their treatment planning so as not to damage the gingival tissues.
In our practice of orthodontics, we have to decide, among many things, whether a patient requires extraction or non-extraction therapy. Non-extraction orthodontic therapy in patients who have reduced arch length requires arch expansion, frequently by moving incisors labially and posterior teeth laterally. Wennström [3] showed that facial movement of the teeth decreased the buccolingual thickness of the tissue, which resulted in gingival recession and an increased clinical crown height. In contrast, lingual movement increased the buccolingual thickness of the tissue, which resulted in coronal migration of the soft tissue margin and decreased clinical crown height. Thus, orthodontists might very well be putting patient’s periodontal health at risk by expanding the arches.
Non-extraction therapy tends to move the incisors forward when dental crowding is present because arch perimeter has to be increased to be able to align the crowded teeth. In today’s competitive world, orthodontists are frequently proclining the incisors to alleviate crowding, to treat patients with non-extraction therapy, even though extraction therapy may be indicated. In some instances, this may be the preference of the orthodontist, but often patients demand that treatment be done without extractions. The Internet has also made it easier for prospective patients to find out that orthodontists can treat patients with or without extractions. Patients naturally opt for non-extraction therapy, not understanding the negative consequences of incisor proclination. Orthodontists and orthodontic companies continue to introduce new ways of squeezing all teeth into dental arches, encroaching upon the enveloping muscular and periodontal equilibrium and filling the face and smiles with teeth to overflowing [4], regardless of the gingival health consequences. Proffit et al. [5] state that “……non-extraction treatment and expansion of the dental arches once again are being carried to an extreme.”
There are, however, additional reasons why lower incisor proclination should generally be avoided. These are that lower incisor proclination:
-
Increases the magnitude of the anterior open bite in open-bite tendency malocclusions
-
Increases the probability of lip incompetence
-
Compromises post-retention lower incisor alignment stability
-
Diminishes chin prominence appearance as the lips are pushed forward
Clinical examples which illustrate the undesirable effects of lower incisor proclination are shown in the following subchapters as well as examples of the procedures the author recommends to avoid lower incisor proclination.
2.2 Apical Migration (Recession) of the Gingival Margin Associated with Lower Incisor Proclination
During the orthodontic treatment planning process, it is important for clinicians to appreciate that differences in gingival tissue architecture can affect treatment outcomes.
Two biotypes of gingival architecture have been described in the literature. These are thick-flat and thin-scalloped gingiva [6, 7]. Thick gingival tissue is probably the image most associated with periodontal health. The tissue is dense in appearance with a fairly large zone of attachment. The gingival topography is relatively flat with the suggestion of a thick underlying bony architecture. Surgical evaluation of these areas often reveals relatively thick underlying osseous forms. Thin gingival tissue tends to be delicate and almost translucent in appearance. The tissue appears friable with a minimal zone of attached gingiva. The soft tissue is highly accentuated and often suggestive of thin or minimal bone over the labial roots. Surgical evaluation often reveals thin labial bone with the possible presence of fenestration and dehiscence [8]. These two tissue biotypes have different gingival and osseous architectures exhibiting different responses when subjected to orthodontic tooth movements. These different responses dictate different treatment modalities. Evaluation of gingival tissue biotypes is thus important in orthodontic treatment planning. Since thick and thin gingival biotypes are associated with thick and thin osseous patterns, the two tissue types will respond differently.
Cook et al. [9] evaluated the correlation between labial plate thickness and thin or thick gingival biotypes—using information obtained from cone beam computed tomography, diagnostic impressions, and clinical examinations of maxillary anterior teeth—and concluded that a significant association existed between gingival biotype and labial plate thickness.
It has been shown that subjects with thin and vulnerable marginal tissue may be prone to the development of gingival recession due to orthodontic movement of the teeth away from the alveolar process [3, 10, 11]. Therefore, gingival biotype should be evaluated and taken into account during the treatment planning stage. A gingival thickness of 2 mm or more is defined as thick biotype, while a gingival thickness of 1.5 mm or less as thin biotype [12]. Various methods have been proposed to measure tissue thickness. De Rouck et al. [13] introduced a simple method to determine the gingival thickness based on the transparency of a periodontal probe through the gingival margin while probing the sulcus at the midfacial aspect of incisors. If the outline of the underlying periodontal probe could be seen through the gingival margin, it was categorized as thin; if not, it was categorized as thick. This method is minimally invasive and was found to be highly reproducible, with 85 % intra-examiner repeatability in a clinical trial of 100 periodontally healthy subjects [13]. In a population study, thick periodontal biotypes were found to be more prevalent (85 %) than thin-scalloped forms (15 %) [14].
Wennström et al. found no relationship between the initial width of the keratinized gingiva and the tendency for the development of gingival recession during orthodontic tooth movements in monkeys. However, they did find that it is the buccolingual thickness that determines gingival recession and attachment loss at sites with gingivitis during orthodontic treatment. In cases with thin gingiva caused by the prominent position of the teeth, there is no need for pre-orthodontic gingival augmentation procedures; the recession and bone dehiscence will decrease when the teeth are moved to a more proper position within the alveolar bone [15]. Wennström also found that the gingival tissue with little thickness in the presence of dental plaque is more susceptible to apical migration of connective tissue attachment with marginal gingiva, especially near the teeth under the influence of orthodontic force [16].
Thus, knowledge of the periodontal biotype is of fundamental importance because the anatomical characteristics of the periodontium, such as gingival thickness, gingival width, and alveolar bone morphology, will determine periodontal behavior when submitted to orthodontic treatment. It should be emphasized that tooth position can significantly alter the gingival parameters. Patients with thin-scalloped biotypes are considered at risk as they have been associated with a compromised soft tissue response following expansion orthodontic therapy [3].
It can be concluded that when the labial gingival tissue covering the lower incisors is of the thin-scalloped biotype, orthodontic proclination of these teeth could result in a reduction of gingival height and perhaps also gingival dehiscence. Patient A illustrates the latter problem. This patient had thin-scalloped labial gingiva covering her lower incisors (Figs. 2.1, 2.2, 2.3, and 2.6). She developed a gingival dehiscence on the labial of her mandibular left central incisor root during her orthodontic treatment (Fig. 2.17). This gingival defect probably arose due to the orthodontic proclination of the lower incisors, which was required for a successful mandibular surgical setback.


Figs. 2.1, 2.2, and 2.3
Pretreatment intraoral views. Note Class III molar and canine relationship, mandibular midline shift to the left, maxillary left canine and premolars in lingual cross-bite, and anterior cross-bite (visible on the extreme lower right side of Fig. 2.3). Note narrow maxillary lateral incisors and thin-scalloped gingival biotype with almost transparent gingiva covering the incisor roots
Patient A was a 19.8-year-old healthy female with a bilateral Class III malocclusion (Figs. 2.1, 2.2, and 2.3). A family history of prognathism was reported. Her facial profile was prognathic (Fig. 2.4) with both her lower lip and chin appearing more prominent in relation to the rest of her soft tissue profile. Her cephalometric lateral headfilm (Fig. 2.5) demonstrated an ANB angle of 0.5° (SNA 85°, SNB 84.5°); her Wits appraisal of jaw disharmony was a negative 9 mm, and her mandibular plane angle relative to the SN line was 34°; her lower incisors were retroclined relative to her mandibular plane (81°); they were 6-mm forward of the NB line, and her maxillary incisors were 4-mm forward of the NA line and at 106° relative to the SN line; she had a negative 3-mm overjet (Fig. 2.6), with all maxillary incisors in anterior crossbite and with minimal overbite. There was 3 mm of mandibular dental crowding (Fig. 2.7) and 4 mm of dental spacing in the maxillary arch mainly due to narrow lateral incisors (Fig. 2.8), which resulted in a tooth size discrepancy. In the transverse relationship, the mandible had a 2-mm shift to the left (Fig. 2.9) due to the fact that the maxillary left canine and left premolars were in lingual crossbite (Figs. 2.2 and 2.3). In centric occlusion, the mandibular dental midline was 2 mm to the left of both the maxillary dental and the facial midlines due to a mandibular forced shift from centric relation to centric occlusion (Fig. 2.2). The frontal face view shows her mandible shifted to the left side while in centric occlusion (Fig. 2.9), but symmetric while smiling and out of occlusion (Fig. 2.10).
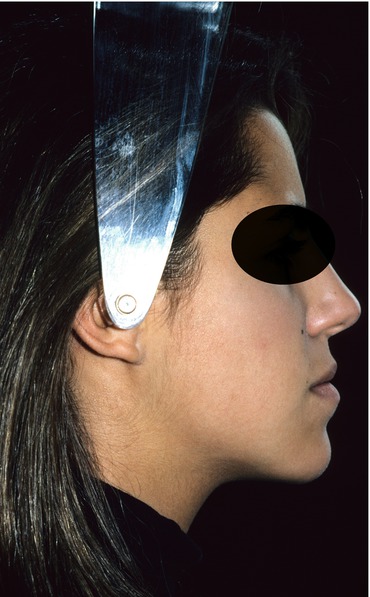



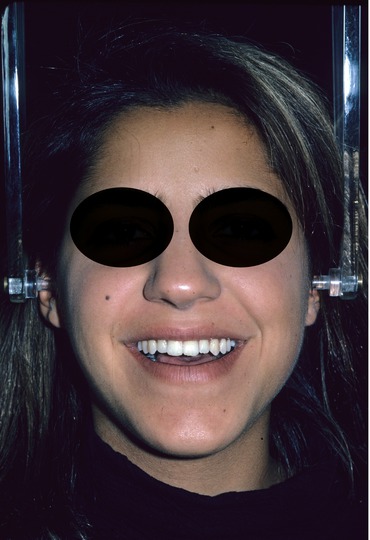
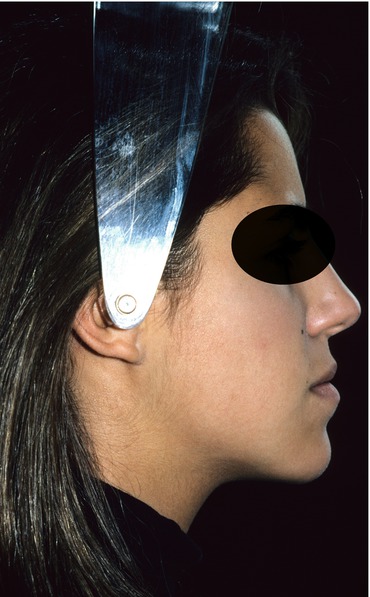
Fig. 2.4
Pretreatment profile facial photograph. Note Class III facial profile

Fig. 2.5
Pretreatment cephalogram. Note anterior crossbite associated with a Class III skeletal relationship

Fig. 2.6
Pretreatment lateral intraoral view of incisors in anterior crossbite. Note narrow maxillary lateral incisor and thin-scalloped gingival biotype
Fig. 2.7
Pretreatment occlusal view of the lower arch. Note 3 mm of dental crowding
Fig. 2.8
Pretreatment occlusal view of the upper arch. Note dental spacing mesial and distal to the lateral incisors and distal to the left canine, totaling 4 mm

Fig. 2.9
Pretreatment frontal facial view with the teeth in occlusion. Note the chin deviated toward the left side
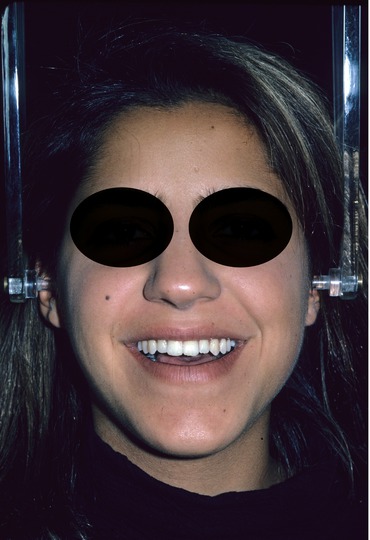
Fig. 2.10
Pretreatment frontal facial view with the teeth out of occlusion. Note that the chin is less deviated toward the left
The patient and her parents were informed that extraction of the two mandibular first premolars, combined with orthodontic treatment, might correct both the anterior and the posterior crossbites but that with this extraction therapy, the chin prominence would appear increased because the lower lip would be retracted and the retroclined lower incisors would appear even more so (observe extreme right side of Fig. 2.3). Non-extraction orthodontic therapy combined with a mandibular surgical setback was thus recommended.
The treatment objectives were to align the lower teeth, to close the maxillary spaces by bonding composite buildups on the narrow maxillary lateral incisors, and to surgically setback her mandible to reduce the excessive chin projection while simultaneously correcting both the anterior and the posterior crossbites. The left posterior crossbite would be automatically corrected during the mandibular surgical setback because as the mandible is surgically moved backward, its transverse width diminishes. Both the patient and her parents accepted this treatment plan, except for the maxillary lateral incisor composite buildups. Thus, the treatment plan was modified. It included closing all maxillary spaces, by incisor retroclination, and aligning the lower teeth, by lower incisor proclination. These orthodontic movements would result in an increased negative overjet thereby creating greater surgical space to achieve facial harmony. This increased negative overjet would allow the surgeon to maximize the mandibular surgical setback and thereby diminish the excessive chin prominence.
Full brackets were bonded to both dental arches, and a progression of arch wires were tied to all the brackets. Six months later, an increased negative overjet of 10 mm had been created (Fig. 2.11) by proclining the lower incisors from 6 to 8.5 mm relative to the NB line and by retroclining the maxillary incisors from 4 to 0 mm relative to the NA line. The thin-scalloped labial gingiva covering the lower incisors is noticeable (Figs. 2.6 and 2.11) and also the worsening of her facial profile, due to proclination of her lower incisors and retroclination of her upper incisors (Fig. 2.12). Full orthodontic records were taken at this time, including a lateral headfilm (Fig. 2.13). Surgical orthodontic arch wires were tied to the brackets (Fig. 2.11), and a chin cup appliance (Fig. 2.14) was given to her to be used nighttime during the 6 months following surgery. The purpose of this appliance was to minimize the relapse tendency of the mandible to move forward again, as reported by Proffit et al. [17]. These authors suggested that the anterior relapse tendency of the mandible could be due to muscular pull as function resumes and that the altered orientation of the elevator muscles, which occurs when the mandible is moved posteriorly, could lead to some forward adjustment of the mandible particularly if the ramus was pushed to a more vertical inclination during surgery. Thus, the chin cup appliance may help stabilize the mandible while postsurgical muscle adaptation takes place.

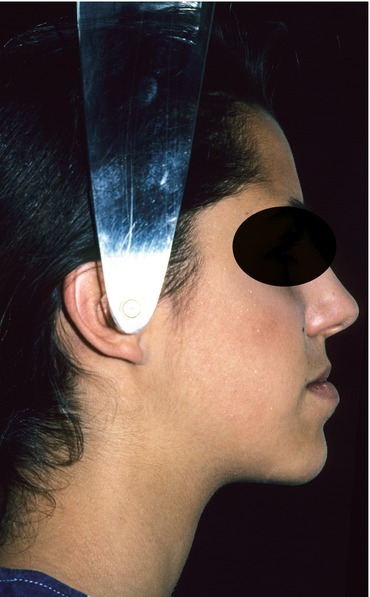



Fig. 2.11
Progress presurgical lateral intraoral view of incisors in anterior crossbite. Note that the negative overjet has been increased, that all maxillary spaces have been closed, and that surgical orthodontic arch wires are in place
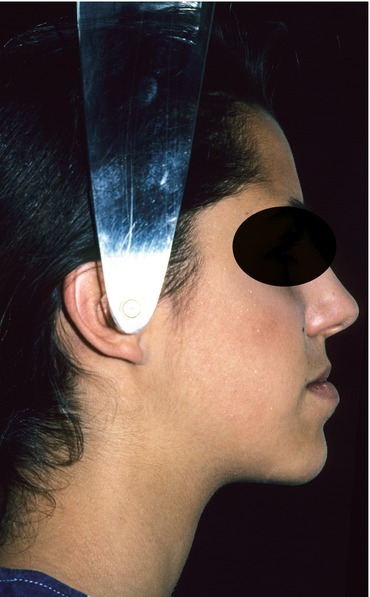
Fig. 2.12
Presurgical facial profile view. Note worsening of the Class III profile due to the orthodontic proclination of the lower incisors and the retroclination of the upper incisors

Fig. 2.13
Presurgical cephalogram. Note orthodontic incisor decompensation created in preparation for mandibular surgical setback

Fig. 2.14
Chin cup appliance given to the patient to minimize the postsurgical relapse tendency of the mandible to move forward again due to muscle pull
The patient underwent surgical setback of her mandible, with simultaneous extraction of her maxillary third molars (Fig. 2.15). One month postsurgery, the facial profile appears greatly improved (Fig. 2.16). Unfortunately, a labial gingival dehiscence developed following the surgical procedure. The dehiscence partially denuded the mandibular left central incisor root. The author attributes the development of this dehiscence to two reasons. The first is that the patient did not brush her teeth well following the surgical procedure, as is usually the case in orthognathic surgery patients; the second is that the patient’s gingival biotype was thin scalloped, which is more susceptible to suffer dehiscence when combined with incisor proclination [3, 16]. The patient was asked to maintain the cleanliness of this area. Three months postsurgery, the brackets were removed, removable orthodontic retainers were given, and posttreatment records were obtained. The patient was then referred to a periodontist to cover the dehiscence (Fig. 2.17) with a free gingival graft (Fig. 2.18), which was harvested from her palatal mucosa.





Fig. 2.15
Immediate postsurgery lateral cephalogram. Note normal skeletal and dental relationships

Fig. 2.16
One month postsurgery facial profile view. Note pleasing facial features

Fig. 2.17
Posttreatment intraoral frontal view. Observe gingival dehiscence in the lower left central incisor root area with partial root denudation

Fig. 2.18
Posttreatment intraoral photograph taken after a free gingival graft was placed to cover the dehiscence. Graft was harvested from the patient’s palatal mucosa
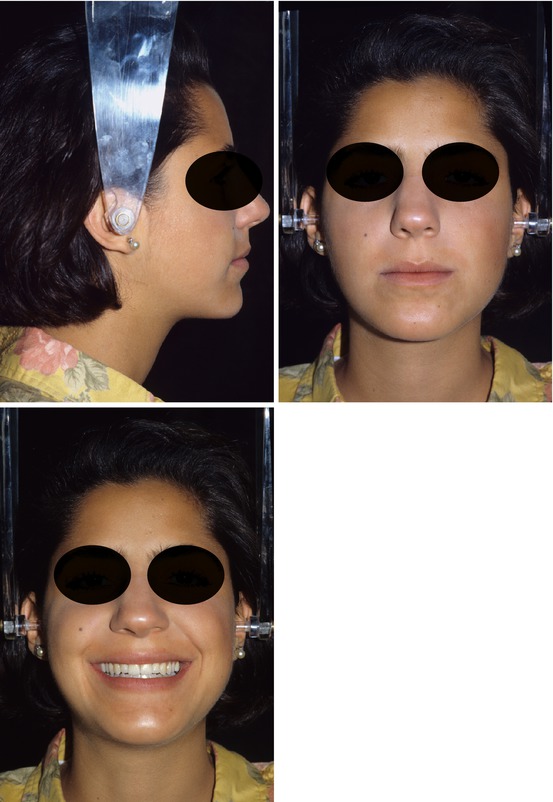
The patient and her parents were very pleased with both the orthodontic (Figs. 2.19, 2.20, 2.21, 2.22, and 2.23) and the facial results (Figs. 2.24, 2.25, and 2.26); facial profile improvement was indeed dramatic when one compares the pre- and the posttreatment facial profile photographs (Figs. 2.4 and 2.24) because the chin and the lower lip projection decreased. The posttreatment cephalometric lateral headfilm (Fig. 2.27) demonstrates an excellent maxillo-mandibular relationship, as well as adequate cephalometric incisor positions. Her ANB angle is now 4° (SNA 84° and SNB 80°), and her Wits appraisal is a positive 2 mm. Incisor positions are also within the cephalometric norms, allowing the lips and chin to have a normal position. Her lower incisors, which were originally retroclined relative to her mandibular plane at 81°, are now at 88°. These incisors were 6 mm in front of the NB line and are now again at 6 mm; her maxillary incisors changed from being 4 mm to 2 mm in front of the NA line and from 107° to 90° with respect to the SN line. These slightly retropositioned maxillary incisors were the result of having closed the maxillary spaces orthodontically. A better occlusal result could have been achieved had the maxillary spaces been closed with lateral incisor composite buildups. With buildups, the maxillary incisors would be more proclined, allowing the mandible to be more advanced, with cusps coinciding with embrasures.



Figs. 2.19, 2.20, 2.21, 2.22, and 2.23
Posttreatment intraoral views. Note well-aligned teeth but not in an ideal Class I occlusion due to the tooth size discrepancy arising from narrow maxillary lateral incisors
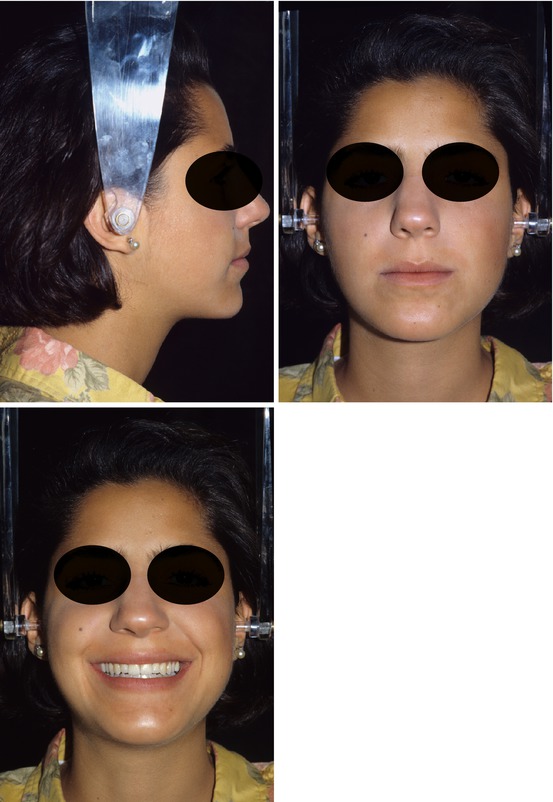
Figs. 2.24, 2.25, and 2.26
Posttreatment facial views. Note facial harmony

Fig. 2.27
Posttreatment cephalogram. Note normal overjet and pleasing facial profile
A maxillary and a mandibular removable retainer were given to the patient one day after bracket debonding with instructions to wear them nighttime for as long as she wished to have straight teeth. The upper retainer that the author recommends is the wraparound type (Fig. 2.28). The reason for using this type of retainer is that the labial/buccal wire does not interfere with the occlusion. The lower retainer design can be seen in Fig. 2.29. It is a retainer that covers both the labial and the lingual of all the teeth in the arch. These retainers impede labiolingual and rotational tooth movements from occurring and also prevent spaces from reopening [18]. Figures 2.30 and 2.31 show the retainers in place. The gingival-labial acrylic of the lower retainer has been cut away in the grafted area. The patient was instructed to return for annual retainer checkups.



Fig. 2.28
Intraoral occlusal view of the removable maxillary wraparound retainer
Fig. 2.29
Intraoral occlusal view of the removable mandibular retainer

Figs. 2.30 and 2.31
Intraoral frontal and right lateral views with retainers in place. Note that in the mandibular retainer, the gingival-labial acrylic has been cut away in the area corresponding to the graft so as not to impinge on it
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


