(1)
Department of Orthodontics, Universidad Intercontinental, Mexico, D.F., Mexico
Abstract
The issue of orthodontic-induced external apical root resorption (EARR) has attracted the interest of clinicians and investigators because of the alarming clinical and legal implications associated with its occurrence in a severe form. The January/February 2005 issue of the American Association of Orthodontist’s Bulletin reported that medical malpractice is a significant problem in the USA today and that patients are filing claims and lawsuits against medical and dental practitioners, including orthodontists, in record numbers. EARR is a common iatrogenic consequence of orthodontic treatment. Cross-sectional as well as longitudinal studies show that EARR is a small problem for the average orthodontic patient, with radiographic mean resorption of less than 2.5 mm. This magnitude of resorption has no adverse clinical consequences. However, 1–5 % of orthodontic patients experience a severe form of EARR, defined as exceeding 4 mm or one-third of the original root length. Severe root resorption mainly occurs in maxillary incisors. It compromises crown-root ratios and can result in tooth mobility. The main etiologic risk factor for the severe form of EARR is genetic predisposition. Emphasis is thus given on the root-sparing treatment procedures to minimize the risk for development of the severe form of EARR.
3.1 Introduction
Root resorption has been classified by Fuss et al. [1] according to the stimulating factors that induce it. The resorption-stimulating factors include pulpal infection resorption, periodontal infection resorption, ankylotic resorption, impacted tooth or tumor pressure resorption, and orthodontic pressure resorption. Infection root resorption can occur either on the internal or the external root surface and is caused by microbial pathogens. Ankylotic root resorption is caused by macrophages digesting hyalinized tissue following tooth macro-trauma; injury to the root surface is usually so large that healing with cementum is not possible; bone is in direct contact with dentin and is laid down without the presence of a periodontal ligament, leading to replacement resorption. Pressure root resorption is caused by orthodontic forces or by pressure of impacted teeth or tumors against adjacent roots. Fuss’ classification of root resorption allows proper treatment rendering by identifying the stimulating factors.
This chapter will be exclusively dedicated to orthodontic pressure resulting in external apical root resorption (EARR), which is the loss of root structure involving the apical region (Figs. 3.1 and 3.2). The chapter has been divided into seven subchapters which include pathology, epidemiology, risk factors, etiology, prognosis, clinical recommendations to protect patients from developing EARR, and recommendations to minimize or avoid malpractice lawsuits.



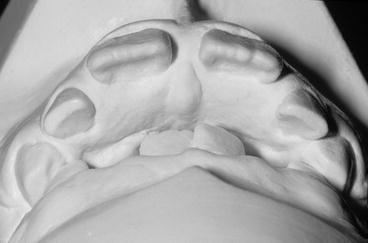
Fig. 3.1
Pretreatment maxillary incisor periapical radiograph of a 36-year-old orthodontic female patient

Fig. 3.2
Posttreatment maxillary incisor periapical radiograph of the same patient at age 39. Four bicuspid extraction case. Note severe EARR which required an intracoronal splint due to incisor mobility
3.2 Pathology
The textbook Contemporary Orthodontics [2] has an excellent description of the EARR process. For the benefit of the reader, the following is a brief summary.
Frontal resorption of the alveolar lamina dura is a desirable process in orthodontic tooth movement because it is not associated with root resorption, while undermining resorption is an undesirable and pathological process since it is associated with root resorption. Undermining resorption occurs when compression of the periodontal ligament (PDL), produced by a sustained orthodontic force against a tooth, is great enough to totally occlude blood vessels and cut off the blood supply to an area within the PDL. Blood flow impediment results in hyalinization, also known as sterile necrosis. During the initial repair phase of the necrosed areas, clast cells resorb not only the underside of the lamina dura but also the cementum and dentin. Removal of hyalinized tissue leads to removal of cementoid and mature collagen, leaving a raw cemental surface that is readily attacked by dentinoclasts. Once orthodontic movement stops, these root craters usually fill back in with cementum, restoring the original contours of the root. However, if the attack on the root surface produced large defects at the apex, they eventually become separated from the root surface. Once an island of cementum or dentin has been cut totally free from the root surface, it will be resorbed and will not be replaced. Thus, shortening of the root occurs when cavities coalesce at the apex, so that peninsulas of root structure are cut off as islands. Then the repair process smoothes over the new root surface and a net loss of root length occurs. Forces are concentrated at the root apex because orthodontic tooth movement is never entirely translatory, which places the narrow periapical region in harm’s way. The coronal third of a root is covered with acellular cementum, whereas the apical third is cellular and the middle third is intermediate. Cellular cementum forms more rapidly and is more active than acellular cementum, but this cellular periapical cementum depends on a patent vasculature. Accordingly, periapical cementum is more friable and easily injured in the face of heavy forces and concomitant vascular stasis. Despite the clinician’s best efforts to keep forces light and well distributed to induce only frontal resorption, some areas of undermining resorption are probably produced in every patient [2].
Light forces are precisely what orthodontists have been applying since the late 1970s when brackets welded to bands were replaced by direct bonding. Bonding brackets to enamel obligated orthodontists to diminish the magnitude of applied force by using lighter wires to avoid accidental dislodgement of brackets. Currently, narrower brackets are available in order to increase the interbracket distance, resulting in additional force reduction due to increased wire springiness. Many orthodontists are using .018″ instead of .022″ slot brackets, which also diminishes the magnitude of forces that can be applied. Further, some orthodontists are even using glass ionomer cement to bond brackets to minimize the development of white spot lesions. This type of cement limits even more the magnitude of forces that can be applied, particularly during the first 24 h after bonding, because of the diminished bonding adhesion of this cement when compared to composite resin. If orthodontic force magnitude would be the main cause for severe EARR, the incidence should have diminished dramatically since less force magnitude has been used for the past 40 years (due to the use of direct bonded brackets). Unfortunately, this has not occurred.
3.3 Epidemiology
EARR is a common iatrogenic consequence of orthodontic treatment. In an extensive literature review of the evidence for EARR and orthodontic treatment, Weltman [3] made several critical observations. First, post-orthodontic treatment incidence of EARR is 73 % (detected radiographically). Cross-sectional as well as longitudinal studies show that EARR is a small problem for the average orthodontic patient with a radiographic mean resorption of less than 2.5 mm. This magnitude of resorption has no adverse clinical consequences, but unfortunately, 1–5 % of orthodontic patients experience a severe form of EARR (defined as exceeding 4 mm or one-third of the original root length). Severe root resorption mainly occurs in maxillary incisors followed by mandibular incisors and mandibular first molars. Finally, this magnitude of EARR compromises crown-root ratios and can unfortunately result in tooth mobility. Incisor mobility sometimes requires splinting (Fig. 3.2).
More recent studies [4–9] investigating EARR incidence and comparing the severity with lighter forces and studies [10–12] investigating heavier forces, used before the introduction of direct bonding, show similar results. The conclusion is that development of EARR may not necessarily be due to the degree of applied orthodontic force per se but also to a patient’s individual genetic predisposition or susceptibility.
3.4 Risk Factors
Many factors have been proposed as risk factors for the appearance of the severe form of EARR. These can be divided into orthodontic treatment-related risk factors and patient-related risk factors [13]. Examples of treatment-related risk factors are treatment duration [14–25], magnitude of applied force [19, 26–31], direction of tooth movement [11, 24, 25, 27, 32–35], amount of apical displacement [16, 21], method of force application (continuous vs. intermittent) [12, 28, 36–41], type of appliance [42–44], and treatment technique [24, 32, 44–53].
Examples of risk factors related to the patient include previous history of EARR [42, 54–56]; tooth-root morphology, length, and roots with developmental abnormalities [4, 7, 9, 11, 21–23, 57–63]; genetic influences [7, 54, 64–68]; systemic factors [69–72] including drugs (nabumetone) [73]; hormone deficiency, hypothyroidism, and hypopituitarism [74–77]; asthma [41, 58]; root proximity to cortical bone [11, 15, 78]; alveolar bone density [15, 79–81]; chronic alcoholism [82]; previous trauma [9, 12, 41, 47, 54–56, 83–85]; endodontic treatment [4, 10, 35, 41, 55, 56, 86]; severity and type of malocclusion [4, 7–9, 11, 16, 17, 20, 31, 54, 87]; and patient age [12, 14, 17, 21, 22, 36, 88–92], patient gender [7, 17, 21, 31, 56, 57, 65, 78, 93], and patient habits [94].
Most researchers agree that all of the identified risk factors only explain a small percentage of the variation in EARR. In 1998, Vlaskalic [95] stated: “The long list of suspected causative factors for EARR highlights the state of ignorance that exists with respect to EARR and orthodontic treatment.” Fortunately, more light has been shed since then on the etiology of EARR. Årtun et al. [96], in 2005, reported the results of a multicenter clinical study on EARR in which maxillary incisor periapical radiographs were obtained in 302 consecutively treated orthodontic patients who had fixed appliances. The radiographs were taken at three time periods: pretreatment and 6 and 12 months after appliance placement. The result was that orthodontic patients with detectable EARR during the first 6 months of active treatment are more likely to experience resorption in the following 6-month period than those without such exhibited early EARR. These authors concluded that the low explained variance of identified risk factors, combined with the strong association between the amount of EARR during the first and second 6-month treatment period, suggested a genetic predisposition as the major etiologic factor.
It can be concluded from this study that it is critical for clinicians to obtain periapical radiographs of maxillary incisors 6 months after fixed appliance placement of every patient to identify patients at risk of further EARR.
3.5 Etiology
EARR is apparently related to a genetic predisposition. Harris et al. [65], in a study using the sib-pair model, reported that the strongest single association with EARR seems to be a person’s genotype since familial studies showed that a person’s genotype accounts for about two-thirds of the variation in the extent of EARR. These authors concluded that an individual’s genetic background is the single strongest predictor of EARR, as shown by familial analysis. The first report, in which a genetic marker was described identifying people who are susceptible to EARR before beginning orthodontic treatment, was published by Al-Qawasmi et al. [64]. This paper, titled “Genetic predisposition to EARR,” investigated whether there is linkage and association between polymorphisms of the interleukin IL-1 genes and EARR. The sample consisted of 35 white American families. Each family included two or more siblings treated with orthodontics. Genomic DNA was obtained for isolation and analysis from buccal swab cells of the siblings and their parents. Highly significant evidence of linkage disequilibrium of IL-1B polymorphism with EARR in the maxillary central incisors was obtained. Persons carrying two alleles # 1 (one from the father, the other from the mother) of the IL-1B have, on average, 1.3 mm more EARR than those with either the alleles 1 and 2 or the alleles 2 and 2. Persons homozygous for the IL-1B allele # 1 have a 5.6-fold increased risk of EARR greater than 2 mm as compared with those who are not homozygous for the IL-1B allele 1. When the EARR value of 2 mm was used to divide subjects into affected and unaffected, 72 % of EARR occurred in those carrying both alleles # 1, followed by 39 % of EARR in those carrying the two different alleles, 1 and 2, and 0 % incidence in individuals carrying the two protective alleles # 2. Thus, data indicate that allele 1 and the IL-1B gene, known to decrease the production of IL-1 cytokine in vivo, significantly increase the risk of EARR. The authors propose a model for the pathway through which IL-1B genotype modulates the extent of EARR experienced during orthodontic tooth movement. Their hypothesis is that low IL-1B production in the case of allele 1 results in less catabolic bone modeling in the cortical bone interface of PDL because of decreased number of osteoclasts associated with lower levels of this cytokine. Inhibition of bone resorption in the direction of tooth movement results in maintaining prolonged dynamic loading of tooth root adjacent to compressed PDL, resulting in more EARR because of fatigue failure of the root. In the case of high IL-1B production associated with allele 2, compressed PDL space is restored by resorption of bone interface of PDL, resulting in only mild EARR that is controlled by the cementum-healing mechanism. In spite of the authors’ encouraging findings that EARR does indeed have a genetic basis, they concluded that the genetic predictors of EARR are not yet reliable because IL-1B polymorphism accounts for only 15 % of the total variation of maxillary incisor EARR. These authors report that many genes besides IL-1B are probably involved, that a search for the remaining genetic factors that influence EARR is ongoing with the ultimate goal of providing orthodontic treatment that circumvents EARR, and that in the future DNA analysis might provide a more accurate risk assessment for EARR.
3.6 Prognosis
This subtopic is subdivided into pretreatment, active treatment, and posttreatment prognosis.
3.6.1 Pretreatment Prognosis
Harris et al. [65] (previously mentioned) suggested that an individual’s genetic background could assist in doing an EARR pretreatment risk assessment. These authors recommended that post-orthodontic radiographs of siblings and/or parents be evaluated to predict risk for EARR. In other words, a prior sibling’s orthodontic outcome could be a useful gauge of another sibling’s risk of EARR. Unfortunately, sibling and parent’s posttreatment radiographs are not frequently available.
3.6.2 Active Treatment Prognosis
When EARR is detected during orthodontic treatment, it will progress for as long as the treatment continues, as demonstrated by (Årtun et al. [96]). Patients should be made aware of the problem. If the decision is to continue orthodontic treatment, further radiographic monitoring of the patient is recommended. Also, even lighter forces should be applied and alternate upper and lower arch wire activations, for example, activating once every 2–3 months each individual arch instead of monthly. Rest periods are thus built into treatment. The teeth are orthodontically moved, followed by a period during which forces are minimized with passive arch wires for 2–3 months to allow root repair. Movement could then be resumed. Therefore, the rate of tooth movement is slowed, and the reparative process of the cementum can keep abreast of the erosive processes of over-compression of the PDL, as the root is forced against the alveolus. A force-free rest period allows the cementum to recover the exposed dentin, thus improving root length at the end of treatment. A pause also permits repair of the necrotic hyalinization zone, including central tissue zones in the PDL that appear to be protective of the root. Levander et al. [97], in 1994, reported a clinical study evaluating the effect of a treatment pause on teeth in which EARR was discovered after an initial treatment period of 6 months with fixed appliances. They found that the amount of EARR was significantly less in patients treated with a pause of 2–3 months than it was in patients treated without interruption.
3.6.3 Posttreatment Prognosis
Once the patient is in the retention phase, EARR ceases [10] and root healing processes occur, such as remodeling of irregular apical areas, apical rounding, smoothing of edges, and return to a normal PDL width. Statistical modeling has shown that 3 mm of apical root loss equates to 20 % loss of attachment area and that 1 mm of crestal bone loss also creates 20 % loss of attachment [98]. Thus, conservation of crestal bone level is paramount when EARR occurs. To improve post-orthodontic treatment prognosis, occlusal equilibration to eliminate interferences is recommended. If tooth mobility is present, an intracoronal stabilizer should be bonded (similar to a canine to canine fixed retainer). In addition, maintenance of excellent oral hygiene and frequent dental appointments for professional prophylaxis are recommended.
3.7 Clinical Recommendations to Protect Patients from Developing EARR
Since orthodontists cannot yet identify which pre-orthodontic patients are susceptible to severe EARR, a signed informed consent is important both for adequate patient education and for proper risk management. Dental histories reporting macro-trauma should alert the clinician because there is an increased risk of EARR associated with macro-trauma [83]. The clinician should also be aware that teeth with short roots have an increased risk of loss in patients who also have crestal alveolar bone height loss [98], particularly if the roots have been shortened even more by EARR. In susceptible patients, the probability of EARR development in its severe form is increased by the following: moving teeth considerable distances [16, 21], using heavy continuous orthodontic forces [19, 26–31], moving teeth that have had previous macro-trauma [83], moving teeth against cortical plates [11, 15, 78] (as is frequently done in patients with severe skeletal discrepancies treated with orthodontics exclusively instead of a combination of orthodontics and orthognathic surgery), and an increased treatment time [14–25]. Specifically, patients who need orthognathic surgery to achieve a successful result, but are treated nonsurgically, usually take longer to treat. Long and narrow roots are also at increased risk for EARR since in tipping movements, the longer the root, the more pressure at the root apex due to longer moment arms. EARR can be minimized in orthodontic patients by moving teeth with light forces, through trabecular bone, with periodic radiographic monitoring and, most importantly, by moving them the least distance possible. This may be accomplished by using the following root-sparing orthodontic treatment regimes:
1.
Growth modification to correct severe skeletal Class II malocclusions
2.
Early interception of maxillary canines that have mesial eruption paths
3.
Serial extraction to modify eruption paths (guidance of eruption)
4.
Correction of anterior open bite with a palatal tongue spur appliance
5.
Orthognathic surgery to avoid moving teeth large distances and against cortical plates
The ultimate goal of these five recommended treatment strategies is to provide orthodontic treatment that circumvents EARR. The following are clinical examples of some of these regimes.
3.7.1 Growth Modification to Correct Severe Skeletal Class II Malocclusions
There is considerable controversy among orthodontists about the timing of orthodontic treatment. Those who promote early treatment in the mixed dentition claim to have better results, even though a second phase of orthodontic treatment may be required. Some orthodontists however prefer to initiate treatment in the late mixed dentition with the belief that they can achieve equally good clinical results in a single phase. This section presents a case report of a Class II, Division 1 patient that significantly benefited from early mixed dentition treatment. Emphasis on early treatment helps to achieve lip competence, prevent incisor fractures, diminish the need for extraction of permanent teeth, and minimize the possibility of EARR. The recommended appliances are shown, as well as the long-term clinical results and stability.
Advantages of early treatment should include the following:
-
Early/timely Class II treatment helps to minimize incisor trauma and external apical root resorption.
-
Prevention of incisor tooth trauma helps avoid its long-term consequences.
-
Combination headgear is superior to functional appliances.
-
Utilization of all the growth accelerations that occur in growing patients rather than just the adolescent growth acceleration is advantageous.
-
Maxillary sutural growth can be easily modified while mandibular growth cannot.
-
Differential growth is the key to long-term stability.
-
Children’s compliance is better than adolescent’s as documented by timing devices [99].
Children with severe skeletal Class II, Division 1 malocclusions, with large overjets, may be treated using their growth potential by inhibiting maxillary growth while mandibular downward and forward growth takes place. Taking advantage of growth to correct an overjet minimizes the need for extensive tooth movement (avoids dental compensations). Therefore, risk of the development of EARR is diminished. In addition, trauma to the incisors may be prevented when lip incompetence due to Class II malocclusion is treated in the early mixed dentition [100–104].
Class II skeletal correction is likely best achieved through the use of a combination occipito-cervical headgear. Functional appliances accomplish Class II correction mostly through tooth movement (proclination of mandibular incisors and retroclination of maxillary incisors) [105, 106], thereby increasing the risk of EARR in genetically susceptible patients. Also, the probability of bicuspid extractions is increased when Class II malocclusion correction is achieved with functional appliances because these appliances tend to procline lower incisors [106, 107]. This proclination, as reviewed in Chap. 2 of this book, compromises long-term stability, periodontal health, and facial esthetics.
In the practice of orthodontics, we as specialists have to decide, among many things, whether a patient requires extraction or non-extraction therapy taking into account the magnitude of dental crowding in the setting of the patient’s initial facial profile. When functional appliances are used to correct Class II malocclusions, the probability of requiring extraction of bicuspids is higher because both fixed and removable functional appliances tend to procline lower incisors. The evidence that lower incisors procline with the use of functional appliances is given by the randomized clinical trials of early Class II treatment published by O’Brien et al. [106] and by Tulloch et al. [107]. The latter study found that 31 % of a group of patients treated in the mixed dentition with a functional appliance (modified bionator) eventually required bicuspid extractions compared with a group of patients who used a combination headgear in which the extraction rate was only 16 %. Patient E serves as an example of how a skeletal Class II malocclusion was corrected in a growing child with the use of a headgear. The patient did not require extraction therapy in the second phase of treatment because proclination of lower incisors did not occur as would have arisen with the use of a functional appliance.
Patient E, treated by the author, illustrates the advantages of using a combination (occipital and cervical traction) headgear to correct a skeletal Class II, Division 1 malocclusion. Correction of a large incisor overjet by growth modification with a headgear avoided having to move incisors thereby protecting them from experiencing EARR. Headgear use also helped avoid the need for extractions in the second phase of treatment because lower incisors were not proclined, a factor also minimizing risk of EARR.
Patient E was a 6.0-year-old healthy girl (Figs. 3.3, 3.4, and 3.5) with a skeletal Class II, Division 1 subdivision malocclusion (Fig. 3.6) with lip incompetence. She exhibited a protrusive maxillary lip, a lower lip trapped behind her maxillary incisors, and a retrusive mandible. Her maxilla was prognathic, and her mandible was retrognathic with an ANB angle of 10° (SNA 85°, SNB 75°). Her vertical relationships were within normal limits, with a mandibular plane to SN angle of 35° (Fig. 3.7). Her lower incisors were slightly protrusive both relative to her mandibular plane (100°) and to her NB line (+5 mm). Her maxillary incisors were somewhat retrusive being 2 mm in front of the NA line but normal relative to the SN line, being at an angle of 102°. She had an 11.5-mm anterior overjet (Figs. 3.8, 3.9, 3.10, and 3.11) and a normal overbite. Her lower incisors were crowded (Fig. 3.12) with the lower dental midline deviated 2 mm to the right of her maxillary dental midline (Fig. 3.9). The molar relationships were end-to-end Class II on the right side (Fig. 3.8) and Class I on the left side (Fig. 3.10).



Figs. 3.3, 3.4, and 3.5
Pretreatment facial photographs of a 6-year-old female patient. Note Class II profile with a protrusive upper lip and a retrusive lower lip associated with a large ANB angle (10°). Also note incompetent lips

Fig. 3.6
Pretreatment close-up of cephalogram. Note large incisor overjet (11.5 mm) due to a retrognathic mandible (SNB 75°) and a prognathic maxilla (SNA 85°), with the lower lip trapped behind the maxillary incisors

Fig. 3.7
Pretreatment cephalogram. Mandibular plane angle to SN is 35°, giving normal vertical proportions
Figs. 3.8, 3.9, and 3.10
Pretreatment intraoral views with teeth in occlusion. Note end-to-end Class II malocclusion on the right side and Class I on the left side, with mandibular dental midline deviated toward the right side. Also note crowding of lower incisors and a maxillary central incisor diastema
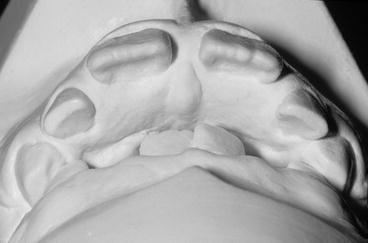
Fig. 3.11
Pretreatment dental casts in occlusion reveal the 11.5-mm incisor overjet

Fig. 3.12
Pretreatment intraoral mandibular occlusal view. Note a 4-mm arch length deficiency without taking into account the leeway space
A combination headgear was recommended to correct the overjet by maxillary forward growth inhibition and naturally occurring mandibular forward growth. Lip incompetence would self-correct with the abovementioned maxillary growth modification. The mixed dentition analysis revealed that all permanent teeth would be able to erupt with sufficient space if leeway space was held. In addition, serial extraction of the primary teeth would be required, starting with extraction of her two primary mandibular canines to allow self-alignment (driftodontics) of her crowded lower incisors. As soon as these incisors self-aligned (by tongue pressure alone), a mandibular lingual holding arch would be cemented on her lower first permanent molars. The patient and her parents were also informed that full fixed appliances might later be required following the eruption of all of her permanent teeth to do the final detailing of the occlusion and to achieve proper dental alignment. Both the patient and her parents accepted the treatment plan.
Treatment objectives were to change the facial profile from maxillary prognathic and mandibular retrognathic to orthognathic, to reduce the anterior overjet, to achieve lip competence, and to align the lower incisors. Maxillo-mandibular growth was expected in this patient since she was a 6-year-old female with her menarche still years away. A combination headgear was recommended to inhibit maxillary horizontal growth while mandibular growth proceeded, hopefully, in a forward and downward direction.
The combination headgear (Fig. 3.13) delivers two simultaneous and equal forces to the maxillary first permanent molars, a cervical distal force and an occipital distal force. The resultant vector of these two simultaneous forces is a horizontal distal force (Fig. 3.14). The objective of applying these two forces is to provide a distalizing force through the molars that will not extrude nor intrude them. These forces, if they are of orthopedic magnitude (400 g per side), modify the growth direction of the maxillofacial sutures [108–114]. The line of action of the force should ideally pass horizontally through the center of resistance of the molars in order to avoid tipping them. This can be achieved by raising the outer bow so that the line of action of the two forces passes through the center of resistance of the molars which is considered to be located at the level of their trifurcation. The maxillary first permanent molars are used as anchors to transmit the orthopedic forces to the maxillary sutures to restrict their horizontal growth rather than to distalize the molars themselves. Even though the molars move distally while the headgear is worn (nighttime), they migrate to their original positions when the headgear is not being worn (usually daytime); the net effect is skeletal modification exclusively, not dental movement. The outer bow should be short, with its distal end coinciding with the anteroposterior position of the anchor molars. The inner bow should be expanded by 2 mm symmetrically so that when it is placed in one molar tube, it rests just outside the other tube. This should be done during the monthly appointments because the relative forward growth of the mandible will produce a posterior crossbite tendency, unless the upper arch width is expanded.
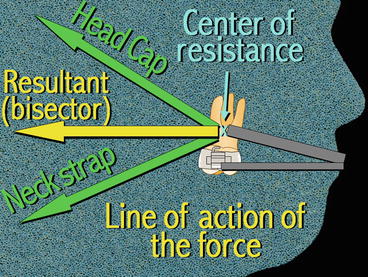
Fig. 3.13
Combination headgear used to restrain maxillary sutural growth in a forward direction while natural mandibular growth proceeds downward and forward
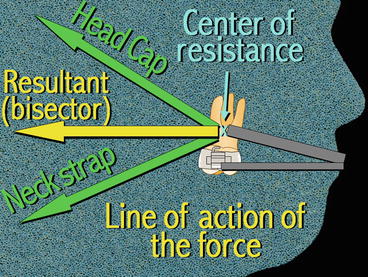
Fig. 3.14
Diagram illustrating the forces and vectors associated with the combination headgear. The objective of the two applied forces (cervical and occipital) on the maxillary first molars is to use them as anchors to transmit these forces to the maxillofacial sutures, inhibiting maxillary forward growth (growth modification)
The patient was given a combination headgear (Fig. 3.13) at age 6.0 with instructions to wear it unfailingly every night and, when possible, afternoons also. Her mixed dentition analysis predicted that all her permanent teeth mesial to the first molars would be able to erupt with sufficient space, without the need to increase arch length. Her mandibular primary canines were extracted to allow the permanent lateral incisors to be aligned by tongue pressure. Three months after the extractions, the lateral incisors were sufficiently aligned (Fig. 3.15) to allow the placement of a fixed lingual holding arch (Fig. 3.16). One year later, the lower first primary molars were extracted (Fig. 3.17) to allow the permanent canines to erupt with sufficient space (Fig. 3.18). Eighteen months later, the lower second primary molars were extracted (Fig. 3.19) to allow the first and second bicuspids to erupt taking advantage of the leeway space. Once all her permanent lower teeth erupted, brackets were bonded to all her lower permanent teeth (Fig. 3.20) to correct minor rotations (Fig. 3.21). Four months later, she was debonded (Fig. 3.22) and the headgear was discontinued. A lower removable retainer (Fig. 3.23) and a maxillary removable wraparound retainer were given to the patient along with instructions to wear them every night for as long as she wished to keep her teeth well aligned. Final records were taken, and the patient was asked to return annually for retainer checkups and to observe whether the third molars would erupt in a correct position.




Fig. 3.15
Three months post-extraction of primary lower canines, progress view at age 6.3. Note that the lateral incisors are in better alignment having been moved forward by tongue pressure. Blue Alastik separators were placed mesial to the lower first permanent molars to create band space for a cemented lingual holding arch

Fig. 3.16
Lower holding arch cemented

Fig. 3.17
Extraction of lower first primary molars to give space for the erupting canines. Progress view
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


