A thorough preoperative evaluation to identify correctable medical abnormalities and understand the residual risk is mandatory for all patients undergoing any surgical procedure, including oral surgery. Routine preoperative evaluation will vary among patients, depending on age and general health. This article addresses the preoperative evaluation of surgical patients in general, and the evaluation for general anesthesia in the operating room.
A thorough preoperative evaluation to identify correctable medical abnormalities and understand the residual risk is mandatory for all patients undergoing any surgical procedure, including oral surgery. Routine preoperative evaluation will vary among patients, depending on age and general health. This article addresses the preoperative evaluation of surgical patients in general, and the evaluation for general anesthesia in the operating room.
Part 1
In evaluating a patient for any surgical procedure, surgeons must consider two aspects: (1) the necessary workup that must be performed for the surgical procedure itself, and (2) whether the patient can safely undergo the planed surgical procedure.
In the preoperative evaluation of a patient for oral surgery, regardless of the clinical setting, a good medical history is undoubtedly the most important aspect. A detailed medical history will identify potential management problems (physiologic and pharmaceutical) and allow the dental surgeon to formulate an oral surgical treatment plan in light of the medical status. Patients will present with one or multiple established medical diagnoses, which may alter how dental care is delivered. The role of the dentist is to determine how these medical problems will influence care, or how dental care may affect medical treatment. Medical illness may predispose to acute physiologic decompensation under stress or failure to do well posttreatment, or lead to drug interactions. Dentists must be aware of what potentially can occur and what precautions must be taken to minimize risks. They must identify issues that should addressed pretreatment (eg, insulin, warfarin, aspirin use), such as illnesses that may cause physiologic decompensation during surgery (eg, angina, seizure disorders, asthma) and conditions that may affect the posttreatment phase (eg, diabetes [infection and delayed wound healing], aspirin use [impaired hemostasis]) ( Tables 1 and 2 ).
| Disease | Suggested Preoperative Evaluation |
|---|---|
| Allergies | Allergies to drugs or latex should be determined |
| Asthma | Emotional factors may trigger an attack Evaluate wheezing and do not treat if patient is wheezing Have rescue inhaler available Do not prescribe nonsteroidal anti-inflammatory drugs or aspirin for pain if the patient has aspirin-induced asthma |
| Cerebral vascular disease | Evaluate blood pressure No elective oral surgery within 6 months of the cerebrovascular accident Patients who have had a stroke are usually on anticoagulation therapy; if so, review method and obtain satisfactory recent International Normalized Ratio (INR) from physician |
| Chronic obstructive pulmonary disease | Only the most severe respiratory compromise is a contraindication to routine outpatient dental/oral and maxillofacial surgical care with local anesthesia Determine the patient’s functional capacity (eg, able to walk a block or two on level ground at 2 to 3 miles per hour [mph]; climb a flight of stairs [five metabolic equivalent tasks]) Plan on not performing long or extensive surgical procedures and do not administer 100% oxygen if the patient is suspected to be on carbon dioxide drive |
| Coagulopathy | Consult hematologist for individuals with definitively diagnosed coagulopathies In the absence of a history of bleeding diathesis, abnormal bleeding following exodontia is rare Prothrombin time or partial thromboplastin time is not indicated |
| Coronary artery disease | Stratify patients based on symptoms and exercise capacity according to history Determine the patient’s functional capacity (eg, able to walk a block or two on level ground at 2 to 3 mph, climb a flight of stairs, do light house work) Patients who can perform these functions are at low risk for cardiac decompensation during oral surgery (see Table 2 ) |
| Diabetes mellitus | Diabetes is only associated with higher perioperative risks in vascular surgery and coronary artery bypass grafting Patients with well-controlled diabetes pose no problem Review symptoms such as excessive thirst, nocturia, malaise, and hunger to assess control |
| Epilepsy | Patients with well-controlled epilepsy are no different from average patients Review compliance with therapy |
| Hypertension |
|
| Liver disease | Screen for hepatitis B and C Patients being treated with Interferon for hepatitis C virus will be anemic and easily fatigued, and platelets may also be low Chronic severe liver disease may increase INR Check history of ethanol use |
| Medication | Medication history will provide information on what conditions the patient is being treated and how severe the condition may be Avoid drug interactions |
| Outpatient treatment with warfarin | Check current INR with treating physician Values of the INR at the therapeutic dose <3.5 does not significantly influence the incidence of postoperative bleeding Dental extractions can be performed without modification of oral anticoagulant treatment INR of up to 3.4 is acceptable for extraction of up to three teeth Local hemostasis with gelatin sponge and sutures seems to be sufficient to prevent postoperative bleeding |
| Renal insufficiency | Consult with nephrologist if patient history is inadequate Compensated renal disease is not a contraindication to office oral surgery and simple extraction of teeth in the office under local anesthesia is not generally a problem For patients undergoing dialysis: perform oral surgery on nondialysis day to avoid problems with anticoagulation In emergency: treat patient more than 4 hours after dialysis; do not use penicillin with potassium (Pen VK) because K + is difficult to eliminate through dialysis and may cause electrocardiogram changes |
| Major Heart Diseases to be Treated in Hospital Setting | Heart Diseases That May be Treated in Office Setting |
|---|---|
| Myocardial infarction within 6 month; delay surgery if possible; consult with cardiologist Unstable or severe angina (class III or IV) Decompensated heart failure (class III or IV; ejection fraction <30%) Significant arrhythmias |
Previous myocardial infarction (more than 6 months prior); determine the patient’s functional capacity. Mild angina pectoris (class I or II) Compensated or prior heart failure (class I or II) Low functional capacity (eg, inability to walk three city blocks) |
Review of the dental history should reveal the patient’s reason for seeking oral surgery, because the procedure will be irreversible. The patient’s previous experience with oral surgery should also be determined because this will aid in the decision to use sedation and in determining how to manage postoperative pain. Surgeons should get to know the patient; the old adage “never treat a stranger” should be applied to the normal preoperative evaluation.
The preoperative evaluation for oral surgery will almost always require imaging studies for proper diagnosis and treatment planning. A panographic radiograph is the gold standard, because it will show the entire dentition of both jaws and adjacent structures, and will permit early and accurate identification of dental aberrations and disease. Other radiographs that could be needed are periapical films for endodontic surgery or to provide greater clarity of detail; localizing films for issues such as impacted canines; and cone beam CT three-dimensional radiographic imaging for implantology or pathology cases.
The initial evaluation should help the general dentist decide on the complexity of the procedure and whether the case should be referred to an oral and maxillofacial surgeon. Both the clinical and radiographic examinations should inform the operator if a tooth extraction will be possible through simple forceps delivery, whether the tooth should be sectioned for ease of removal, or whether a surgical flap is necessary.
Part 2
Preoperative Anesthesia Evaluation
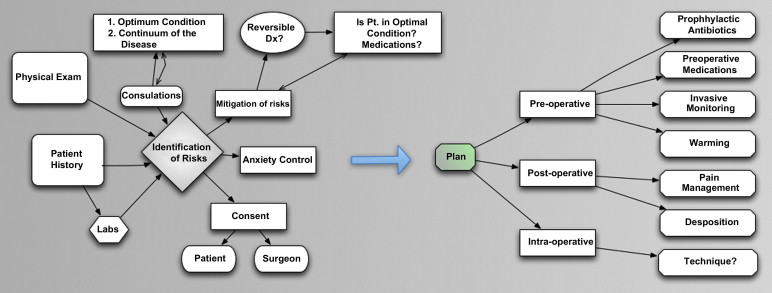
Preoperative evaluation is the foundation for maximizing the chances of the desired outcome, from both the surgical and anesthesia perspectives, because during this process risks are identified and mitigated, and a plan is developed that best balances the risks, benefits, and alternatives available. The products of preoperative evaluation process are diminished patient anxiety and accomplishment of the first steps of risk mitigation and the essential first phase of the informed consent process. Ultimately, the sum of the work product leads to a plan that encompasses the pre-, intra-, and postoperative periods, and establishes the pain management plan and where the patient will go after surgery.
As seen in Fig. 1 , the preoperative evaluation is a truly iterative process. As information is gathered and decisions made in one aspect of the evaluation, upstream and downstream elements may change, and may require starting over from the beginning, until the full picture is elucidated. The preoperative evaluation is a highly dynamic process, requiring frequent thoughtful pauses and reconsiderations as information is gathered and the needs of the patient and surgeon and the abilities of the organization are considered in the development of a perfect plan.
The Perfect Plan
The perfect plan is one that melds the patient’s needs, the care team’s capabilities (knowledge, experience), and the ability of the organization to support (bits, pieces) the contemplated procedure. For completeness sake, the perfect procedure is the one that maximizes the patient’s desired outcome. Occasionally the perfect procedure is so far from what is being offered that no procedure at all should be performed, and other times a procedure should be performed elsewhere. The patient and care team must collaboratively decide how close to perfection is acceptable, when perfection itself is elusive. During the preoperative evaluation process is when this “go/no go” decision must be made.
Elements of an anesthesiologist history and physical
Each member of the clinical care team must perform an evaluation. Unquestionably, each member can use the information obtained by another, and independently verify the information as needed. The team must acknowledge that each specialty has its own perspective, albeit overlapping, to bring to the evaluation table. For example, the surgeon may consider gender from the point of view of disease prevalence and function, the nurse from the vantage point of social issues, and the anesthesiologist may be thinking about the need for a pregnancy test. Each specialty has its own anxiety points that must be addressed during the evaluation period, and therefore each specialty must, in some measure, perform its own assessment. Table 3 lists some of the common historical questions that most practitioners explore, and how an anesthesiologist would consider the information.
| Historical Area | Anesthesia Import |
|---|---|
| Proposed procedure | Patient positioning, possible anesthetic techniques, fluid shifts, blood loss, invasive monitoring, prophylactic antibiotic requirement |
| Past medical history | Possibility of recrudescence, psychological (anxiety) impact, lingering physical impact |
| Concurrent medical history | End-organ damage, where the patient is in the continuum of disease, whether the patient is in optimal condition, whether the disease processes be reversed, need for full stomach prophylaxis, need for prophylactic beta-blockade |
| Medications | Indication of disease severity, drug interactions |
| Surgical history | Psychological impact, increased complexity if returning to the same area, disease severity, difficult airway previously, history of postoperative complications, such as nausea and vomiting or delayed awakening |
| Family history | Malignant hyperthermia and other genetic disorders |
| Gender | Proper approach, pregnancy testing, increased sensitivity to nausea and vomiting postoperatively |
| Age | Pharmacokinetic and dynamic impact, patient interaction/communication, different equipment/skills for pediatric age group, associated ischemia risks |
| Smoking | Carboxyhemoglobin level, reactive airway disease, postoperative intubation increased, pulmonary disease, diminished postoperative nausea and vomiting |
| Sleep apnea | Need for postoperative respiratory monitoring until narcotics are no longer needed, increased intubation risks, associated cardiovascular disease |
| Height and Weight | Obesity is linked to full stomach risks, and the need to base most medication dosing on lean body weight, with airway and pulmonary issues Body positioning and equipment consideration go along with morbid obesity In patients with markedly low body mass index, the pharmacokinetic impact of low protein state must be considered |
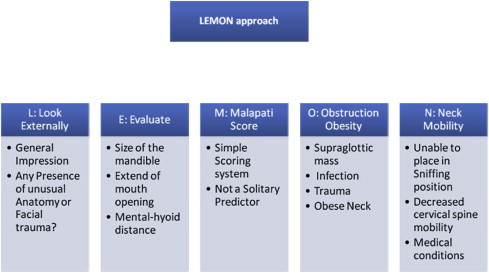
Similarly, the unique point of view each specialty brings to the evaluation of historical data is what is brought to the physical examination. Physicians are taught early on that pertinent positive and negative findings are the drivers of not only the history but also the physical examination. The anesthesiologist’s point of pride is the airway examination, with a focus on trying to discern whether difficulty will be encountered on ventilating or intubating the patient. No one best airway examination component exists; rather, the anesthesiologist must integrate the totality of the examination to reach a conclusion. One commonly adopted algorithm of airway evaluation is the LEMON approach ( Fig. 2 ).
The Mallampati classification ( Fig. 3 ), which relates tongue size to pharyngeal size, is a common component of a thorough airway examination. The examination is performed with the patient in the sitting position, the head held in a neutral position, the mouth wide open, and the tongue protruding to the maximum. The subsequent classification is assigned according to the pharyngeal structures that are visible:
-
Class I: visualization of the soft palate, fauces, uvula, and anterior and posterior pillars
-
Class II: visualization of the soft palate, fauces, and uvula
-
Class III: visualization of the soft palate and the base of the uvula
-
Class IV: soft palate not visible at all.
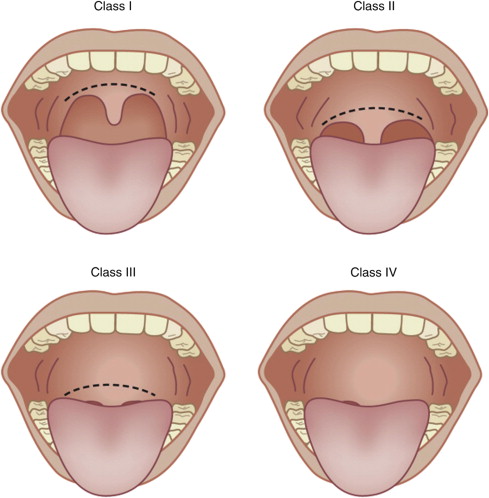
The anatomic considerations in determining whether the patient can be intubated revolve around mouth-opening ability, relative sizes of the oral structures, and the ability of the mobile parts of the airway axes to align in a “sword swallower” sniffing position. Although the Mallampati classification evaluates soft tissue sizes and relationships, along with mouth opening, 13 other examination features should also be considered as part of the airway evaluation, as listed in Box 1 .
-
Previous complications
-
Loose teeth or dentures
-
Buck teeth
-
Long upper incisors
-
Cannot prognath
-
Interincisor distance <3 cm
-
Nonvisualized uvula
-
High or arched palate
-
Thyromental distance <6 cm
-
Noncompliant submandibular space
-
Short neck
-
Thick neck
-
Not capable of sniffing position
-
Mallampati classification
Other particular parts of the physical examination, beyond the basic heart and lung examination, are directed by the contemplated surgery and anesthetic technique, along with the patient’s presentation. For example, a patient undergoing a carotid endarterectomy would require a more concerted neurologic examination. The fine art of history and physical examination must embrace documenting the pertinent positive and negative findings after integrating large quantities of information from the surgeon, patient, and other sources.
The history and physical examination work product
The history and physical examination contribute to several follow-on activities, such as ordering consultations and laboratory investigations, along with the initial steps in risk mitigation, anesthesia plan development, and the informed consent process. As areas of concern become unmasked, more tests or consultations and different approaches to mitigating the risks may become necessary. As the evaluation telephoto lens is brought from near to far, and back again, changes in the anesthesia plan and consent must be kept in mind.
Consultations are necessary when questions remain that are beyond the evaluating physician’s knowledge base. The basic questions that are asked of the consultant are (1) is the patient in optimal condition, (2) does the patient have reversible disease, and (3) where is the patient in the continuum of disease. Simply sending a request to a consultant to clear a patient for surgery is likely to yield an equally noninformative response of “patient cleared,” and must be avoided. The consultant is a key member of the preoperative evaluation team. Referral patterns are frequently in place with consultants who are sensitive to preoperative evaluation needs; this type of network should be encouraged. Basic required tests can be ordered in advance of the consultant appointment, such as an echocardiogram, before the internist or cardiologist sees a patient with known heart disease. The need for quality communication cannot be overstated, especially with consultant interactions. Calling the consultant before sending the patient over for evaluation can speed the preparation process tremendously, with the invested time yielding substantially greater insight when the final report comes back. The request to the consultant should include the three basic questions mentioned earlier, laying the groundwork for answers.
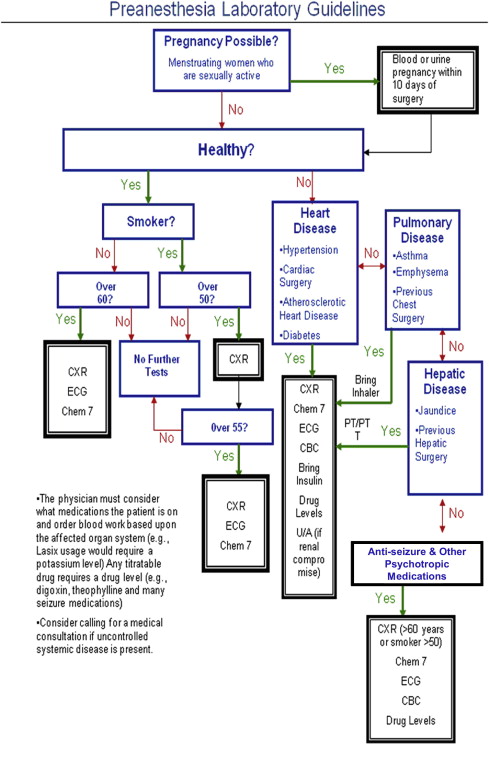
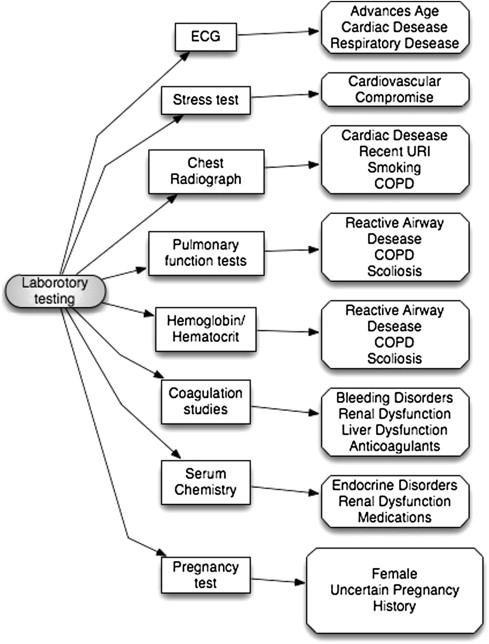
Laboratory guidelines
A few considerations must be addressed before a laboratory investigation is ordered, and which routine tests, other than pregnancy testing, should be avoided must be determined. First, the physician should determine whether the laboratory results will make a difference in treatment. If the results of the laboratory investigation will make no difference, then it should not be performed. Second, whether the disease is prevalent in the patient population should be determined, and then the laboratory investigation may be considered a screening tool, such as an echocardiogram in the elderly to screen for ischemic heart disease. Otherwise, laboratory investigations should answer the same basic questions for which consultations are sought: (1) is the patient in optimal condition, (2) does the patient have reversible disease, and (3) where is the patient in the continuum of disease. An example of this approach is to order a pre- and post-bronchodilator pulmonary function test for a patient with asthma. Fig. 4 highlights a suggested rational thought process in ordering laboratory tests, and Fig. 5 highlights supporting information.
The marriage of patient- and surgery-specific risks
When the history, physical, consultations, and laboratory tests are completed, the patient-specific risks should be clear, and the surgery-specific risks must now be considered, which together will yield total patient risk. Fluid shifts, blood loss, and surgical site are part of the surgical contribution to the total risk palate. Intrathoracic, cardiac, major intra-abdominal, major vascular, and long bone procedures, and those that are likely to result in 20% blood loss (typical adult, 1000 mL), are all considered to present a major surgical risk ( Fig. 6 ).
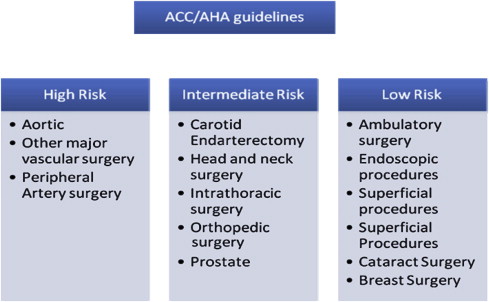
Total patient risk is determined by patient-specific risk combined with surgical risk. Anesthesia-specific risk is negligible, because it is low in modern practice. The first key element of the preoperative evolution is completed once total patient risk is identified and quantified, and then practitioners can proceed to the second element, risk mitigation.
Risk Mitigation
Risk mitigation strategies must be considered and a balance found between the risks and benefits of performing an oral procedure. Alternative approaches and when it is appropriate to perform no intervention should also be considered. The first step in risk mitigation is to ensure that the patient is in as good condition as possible. Disease that can be reversed should be, and the forthcoming surgical and anesthesia procedures that are now being considered must take the patient-specific issues into consideration, always ensuring that the risk/benefit ratio stays in the patient’s favor. For example, in a smoker who is a high-risk patient, risk mitigation involving smoking cessation and allowing time for the body to recalibrate to the new state would reduce the risk to almost the same as the general population. Medical practice is now effective at getting patients in optimum condition for surgery. Three areas of risk mitigation, beyond selection of the anesthetic technique, are frequently missed by the perioperative team: full stomach prophylaxis, beta-blockade with superior pain management, and avoidance of postoperative nausea and vomiting.
Full Stomach
A full stomach before surgery is a concern because of the risk of aspiration and the difficulty with intubation if stomach contents are in the posterior pharynx. Once general anesthesia is induced, patients lose their ability to maintain a patent airway and breath and the protective ability to cough. The elements to consider are gastroesophageal junction tone minus hydrostatic pressure within the stomach, which is equal to barrier pressure. If the barrier pressure is negative, the patient is at high risk for regurgitation or vomiting. Therefore, to ensure a positive barrier pressure, patients are required to fast before surgery in an attempt to lower the hydrostatic pressure. Many articles have been written on what constitutes sufficient time for stomach emptying, with modern practice segregating the issues into type of meal and patient age. Based on the body of literature, Tables 4 and 5 provide somewhat conservative approaches to preoperative fasting. However, these must be regarded as a set of guidelines rather than a firm set of rules.
| Ingested Material | Minimum Fasting Time (h) |
|---|---|
| Clear liquids | 2 |
| Breast milk | 4 |
| Infant formula | 6 |
| Nonhuman milk | 6 |
| Light meal | 6 |
| <6 mo | No milk or solids 4 h before procedure | b No clear liquids 2 h before procedure |
| 6 mo to 3 y | No milk or solids 6 h before procedure | No clear liquids 3 h before procedure |
| >3 y | No milk or solids 8 h before procedure |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


