Minor oral surgical procedures make up a significant part of the daily practice of dentistry. With the increased sophistication of medical technology and medications there is increased likelihood of performing surgery on patients who are being treated for conditions that require some type of anticoagulant therapy. These patients are at an increased risk for perioperative bleeding or thrombotic complications if anticoagulation is discontinued or the dosage is adjusted. Therefore, a fine balance needs to be obtained and adequate preparation of these patients is the key to establishing this balance. This article reviews suggested approaches to the management of such patients.
Medical advances have led to an increase in life expectancy; however, there has also been a greater prevalence of many chronic illnesses. This has resulted in more patients who present to dental offices on anticoagulant medications. There are a variety of discordant approaches to the treatment of surgical patients on anticoagulant therapy, despite many new studies that purport to provide a guide forward. Some have presented new guidelines that attempt a strict algorithmic approach to patient management. Wahl, in a major review of the literature, suggested that most patients undergoing minor oral surgery did not need to stop or decrease their warfarin or antiplatelet drugs, whereas Todd suggested a more individually tailored approach. This article reviews the different aspects of this ever-present challenge and provides our perspective and guidelines to assist with the management of these patients.
Assessment
A thorough medical and dental history is critical to the identification of patients who may be on some type of hemostasis-altering medication. The dentist must be familiar with the types of diseases and conditions that necessitate the alteration of coagulation mechanisms and the different laboratory tests that are used to assess the coagulation status in these patients. Consultation and coordination of care with the patient’s primary care physician and any other appropriate medical specialist is important to the successful management of the surgical intervention. This, however, does not supplant the primary role of the dentist being the leader of the team taking care of these patients, once the dentist assumes the role of the patient’s surgeon. In addition there should be an awareness of the different laboratory tests and their implications in the management of patients on oral anticoagulation therapy (OAT).
Investigations
The laboratory investigations that are useful in the evaluation and preparation of the patient include a complete blood count (CBC), prothrombin time (PT), activated partial thromboplastin time (aPTT), international normalized ratio (INR), and, in some cases, bleeding time. The CBC involves quantitative evaluation of hemoglobin (g/dL) and platelets ( Table 1 ).
| Test | Normal Ranges | Clinical Significance | Clinical Presentation | |
|---|---|---|---|---|
| Male | Female | |||
| Red blood cells | 4.7–6.1 million cells/μL | 4.2–5.4 million cells/μL | Anemia. If present can represent chronic blood loss, which may mean bleeding diathesis. | Fatigability, pallor, tachycardia |
| Hematocrit | 40.7%–50.3% | 36.1%–44.3% | As above | As above |
| Hemoglobin | 13.8–17.2 g/dL | 12.1–15.1 g/dL | As above | As above |
| Platelets | 150 to 400 × 10 9 /L | Thrombocytopenia. Rule out platelet destruction, eg, HIT | Petechiae, purpura, ecchymosis | |
The quantitative levels of platelets may be normal, but platelet function maybe reduced because of medications, such as aspirin, or clinical conditions, such as uremia. The vascular phase of hemostasis and platelet function is evaluated with the bleeding time. This is a test where a 1-mm slit is made in the skin and blotted with filter paper and timed to determine when bleeding stops. The normal time should be 7 to 9 minutes. However, this test is now less commonly used in standard workup of patients, and some studies have shown that there is little predictive outcome with respect to postoperative bleeding in patients having minor oral surgery. A prolonged bleeding time offers more information with regard to bleeding risk, although a normal test cannot exclude the possibility.
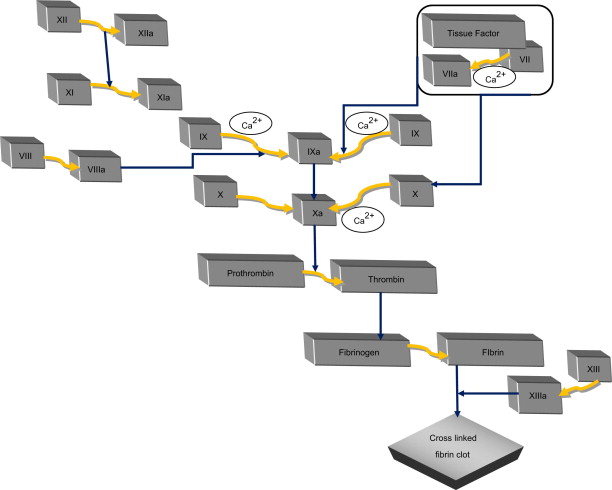
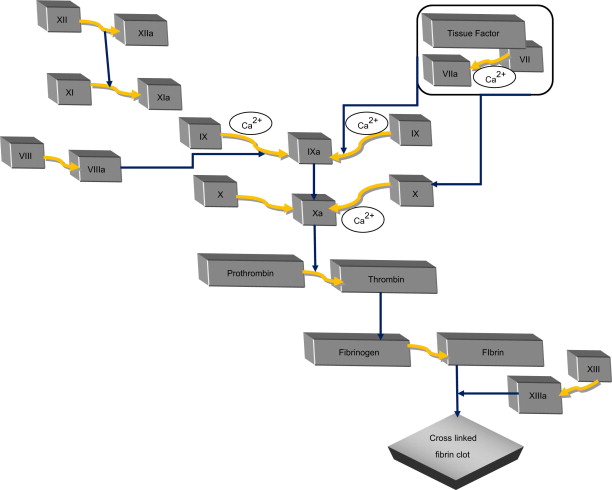
The coagulation tests that are commonly used in practice to monitor bleeding risk and anticoagulant therapy are prothrombin time (PT), activated partial thromboplastin time (aPTT), and thrombin time (TT). aPTT is a measure of the intrinsic pathway of coagulation used in the monitoring of heparin therapy and is usually abnormal in patients with hemophillia. Values are compared with a control and should be within 7 seconds of the control. Values usually range from 25 to 35 seconds. It is usually prolonged if a patient has less than approximately 30% of normal activity. PT measures the integrity of the extrinsic coagulation pathway ( Fig. 1 ). This test is used to monitor warfarin therapy. Values should be compared with a control value, but normal usually range from 12 to 15 seconds. TT is a less frequently used blood test and is used to assess fibrin production. The INR measures the ratio of the patient’s PT to a normal sample that is designed to standardize the differences among laboratories. It is also used to monitor warfarin therapy and the extrinsic coagulation pathway. The normal range is 0.8 to 1.2 and the therapeutic range for anticoagulation is 2.0 to 4.0.
Investigations
The laboratory investigations that are useful in the evaluation and preparation of the patient include a complete blood count (CBC), prothrombin time (PT), activated partial thromboplastin time (aPTT), international normalized ratio (INR), and, in some cases, bleeding time. The CBC involves quantitative evaluation of hemoglobin (g/dL) and platelets ( Table 1 ).
| Test | Normal Ranges | Clinical Significance | Clinical Presentation | |
|---|---|---|---|---|
| Male | Female | |||
| Red blood cells | 4.7–6.1 million cells/μL | 4.2–5.4 million cells/μL | Anemia. If present can represent chronic blood loss, which may mean bleeding diathesis. | Fatigability, pallor, tachycardia |
| Hematocrit | 40.7%–50.3% | 36.1%–44.3% | As above | As above |
| Hemoglobin | 13.8–17.2 g/dL | 12.1–15.1 g/dL | As above | As above |
| Platelets | 150 to 400 × 10 9 /L | Thrombocytopenia. Rule out platelet destruction, eg, HIT | Petechiae, purpura, ecchymosis | |
The quantitative levels of platelets may be normal, but platelet function maybe reduced because of medications, such as aspirin, or clinical conditions, such as uremia. The vascular phase of hemostasis and platelet function is evaluated with the bleeding time. This is a test where a 1-mm slit is made in the skin and blotted with filter paper and timed to determine when bleeding stops. The normal time should be 7 to 9 minutes. However, this test is now less commonly used in standard workup of patients, and some studies have shown that there is little predictive outcome with respect to postoperative bleeding in patients having minor oral surgery. A prolonged bleeding time offers more information with regard to bleeding risk, although a normal test cannot exclude the possibility.
The coagulation tests that are commonly used in practice to monitor bleeding risk and anticoagulant therapy are prothrombin time (PT), activated partial thromboplastin time (aPTT), and thrombin time (TT). aPTT is a measure of the intrinsic pathway of coagulation used in the monitoring of heparin therapy and is usually abnormal in patients with hemophillia. Values are compared with a control and should be within 7 seconds of the control. Values usually range from 25 to 35 seconds. It is usually prolonged if a patient has less than approximately 30% of normal activity. PT measures the integrity of the extrinsic coagulation pathway ( Fig. 1 ). This test is used to monitor warfarin therapy. Values should be compared with a control value, but normal usually range from 12 to 15 seconds. TT is a less frequently used blood test and is used to assess fibrin production. The INR measures the ratio of the patient’s PT to a normal sample that is designed to standardize the differences among laboratories. It is also used to monitor warfarin therapy and the extrinsic coagulation pathway. The normal range is 0.8 to 1.2 and the therapeutic range for anticoagulation is 2.0 to 4.0.
Anticoagulants
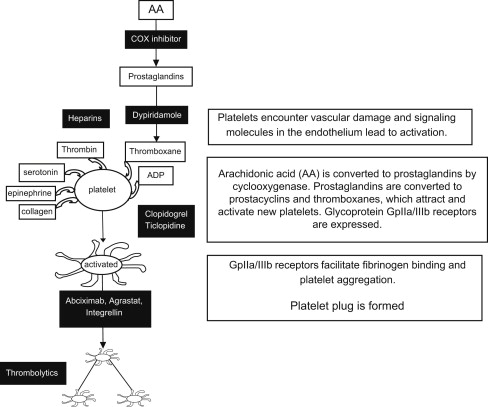
Hemostasis is the arrest of bleeding either by physiologic processes involving vasoconstriction and activation of the coagulation cascade or by surgical processes. Medications that interrupt this process can be grouped into 2 primary categories: anticoagulants that interrupt the coagulation cascade and antiplatelet factors ( Fig. 2 ). There is an increased risk of bleeding with the use of all anticoagulants, but some more so than others. The type of medical condition and the attendant use of anticoagulants can be used to assess bleeding risk and hence it is important for the practicing dentist to be familiar with this area of medicine.
Warfarin is an oral anticoagulant that was discovered in Wisconsin more than 80 years ago. It was initially used as a rat poison but was discovered to have human applications as a result of a failed suicide attempt by an American sailor in 1955. It works by inhibiting vitamin K–dependant coagulation factors and its effect is dose dependant. The half-life is 36 hours and its full effect takes 72 to 96 hours. The anticoagulation efficacy is measured by the PT and INR. A target INR range of 2.0 to 4.0 is used for most patients. It is metabolized in the liver and excreted via the kidneys. Various medications can potentiate or decrease the effect of the drug, and a thorough knowledge of these medications is important. Table 2 lists some of these medications. Warfarin is metabolized in the liver via a similar mechanism as many other drugs; therefore, when it is administered simultaneously with some medications, it may result in either an increase or decrease in the blood concentration of warfarin, thus affecting the efficacy of its action (see Table 2 ). Warfarin has also been shown to interact with many herbal medications. Drugs that are highly protein bound will displace warfarin and increase its blood concentration, leading to an increase in the INR.
| Enhancers | Inhibitors |
|---|---|
| Metronidazole – antibiotic | Barbituates |
| Macrolide antibiotics – eg, erythromycin, clarithromycin, least affected by azythromycin | Carbamazepine |
| Phenytoin | Cholestyramine |
| Sulfamethoxazole – component of the antibiotic Bactrim | Rifampin |
| Ciprofloxacin | Thiazide diuretics |
| Ginkgo biloba, Ginseng | Vitamin K |
Heparin was discovered in 1916 and is usually derived from porcine mucosa. It is a parenteral drug that inhibits thrombin and factor Xa. Administration is intravenous (IV) or subcutaneous (SC) and it primarily affects the intrinsic coagulation pathway. It has a short half-life of approximately 1 hour and is mainly administered via IV infusion or intermittent SC injection. The anticoagulation effects of this drug are monitored via measuring the aPTT, which should be 1.5 to 2.0 times the normal. Platelets should also be reviewed because of the risk of the rare side effects of heparin-induced thrombocytopenia (HIT) and heparin-induced thrombocytopenia and thrombosis (HITT). These usually occur within the first 10 days of starting heparin therapy but can occur up to many weeks after it has been discontinued. Heparin is more commonly used in the hospital setting rather than for outpatient management.
Depolymerization of heparin produces low molecular-weight heparin (LMWH). LMWH requires less monitoring than heparin and hence is often used in outpatient management for patients who require relatively short-term anticoagulation ( Table 3 ). LMWH is also used for in-hospital patient care for therapeutic or prophylactic treatment of conditions such as deep vein thrombosis (DVT). LMWH is available for SC or IV use only. Warfarin is known to have its clinical and practical limitations so ultra-low molecular-weight heparins are currently being developed; for example, semuloparin and bemiparin.
| Anticoagulants | Mechanism of Action | Use/Indication |
|---|---|---|
| Unfractionated Heparin |
Inhibits antithrombin III and factors IXa, Xa, XIa, XIIa, and thrombin Inhibits heparin cofactor |
Prophylaxis and treatment of thromboembolic diseases (DVT, pulmonary embolus, atrial fibrillation with emboli and dialysis. Monitored via aPTT. |
| Low molecular-weight heparin (enoxaparin, dalteparin, tinzaperin) |
Inhibit factor Xa and thrombin | As above. Acute MI and adjuncts to coronary percutaneous intervention. Monitoring is not required but can be done by assay for anti- factor Xa activity. |
| Selective factor Xa inhibitors (indirect) (Fondaparinux) |
Inhibits factor Xa by binding to antithrombin III | Main indication for use is DVT prophylaxis but is also used for the treatment of DVT and thromboembolism. No need to monitor anticoagulant effects. |
| Direct thrombin inhibitors (lepirudin, argatroban, dabigatran-oral administration) |
Inactivate thrombin | Acute coronary syndrome with or without percutaneous intervention, atrial fibrillation, acute ischemic stroke, treatment and prophylaxis of DVT. Monitor with aPTT. |
| Warfarin | Inhibits hepatic synthesis of the vitamin K–dependent coagulation factors II, VII, IX, and X and the anticoagulant proteins C and S. | Mechanical valves, chronic atrial fibrillation, deep venous thrombosis, pulmonary embolism, and dilated cardiomyopathy. Monitored with PT and INR. |
| Antiplatelet drugs Aspirin Clopidogrel (Plavix), Prasugrel (Effient), Ticlopidine (Ticlid) Cilostazol (Pletal) Abciximab (ReoPro), Eptifibatide (Integrilin), Tirofiban (Aggrastat) Dipyridamole (Persantine) |
Cyclo-oxygenase inhibitors. ADP receptor inhibitors. Phosphodiesterase inhibitor. Glycoprotein IIB/IIIA inhibitors (intravenous use only). Adenosine reuptake inhibitors. |
Treatment and prevention of arterial thrombi. see Fig. 3 |
Fondaparinux is a selective Factor Xa inhibitor that is administered SC. This class of drug is chemically similar to LMWH and does not require monitoring of the drug action during use.
Antiplatelet Medications
There are various antiplatelet medications that are used to aid anticoagulation. Some are used both therapeutically and for prophylaxis, for example, aspirin. There are others that are used primarily for therapeutic purposes. These may be given together with aspirin or as single-dose therapy. Knowledge of how they work and the implications for their withdrawal from therapy is imperative in the proper surgical management of patients on OAT.
Aspirin is one of the most commonly encountered medications in a patient’s drug history. The active ingredient is acetylsalicylic acid. It is used in the treatment of a myriad of conditions and functions as an analgesic, anti-inflammatory, antipyretic, and antiplatelet medication. It belongs to the group of medications known as nonsteroidal anti-inflammatory drugs. It irreversibly inhibits platelet action, unlike other drugs in the group. The PT, aPTT, and platelet count are usually normal in patients on aspirin therapy but the bleeding time may be prolonged.
Clopidogrel irreversibly inhibits the adenosine diphosphate receptors on platelets and thus inhibits aggregation and clot formation. It is an alternative drug for persons who require anticoagulation who are unable to tolerate aspirin therapy.
The more common antiplatelet medications enjoy widespread use in the population. Both dental and medical clinicians still encourage stoppage of these drugs from 7 to 10 days before surgery. Although there is a paucity of prospective studies on cessation of antiplatelet drugs as compared with cessation of warfarin, the few that are available support continuation for minor oral surgery. One such study, by Partridge and colleagues published in 2008, compares a group of 27 patients on various antiplatelet medications with a control group of 23. They found no difference in postoperative bleeding. This sample size is small and none of the patients were noted to be on dual antiplatelet therapy, which limits how much that can be extrapolated from the study. Other retrospective reports have been in congruence with Partridge and colleagues’ therefore, for minor limited oral surgery procedures, the literature supports maintenance of therapy.
An overview of a patient’s drug history is not only important for the primary anticoagulant medications but also for those with secondary anticoagulation effects. These may increase the risk of bleeding and include drugs such as simvastatin used in the management of hypercholesterolemia.
Conditions That May Require Anticoagulant Therapy
Knowledge of the various disease states that often require patients to be on anticoagulants is the first step in managing these patients. The most common ones are patients with mechanical cardiac valves, atrial fibrillation, DVT, pulmonary embolism, peripheral vascular disease (PVD), myocardial infarction, and ischemic strokes, among others.
Patients who present to the dental office with these or similar conditions should undergo further evaluation to ascertain the degree of anticoagulation. The patient’s primary care physician should be contacted to discuss the relative need for maintaining anticoagulants during minor oral surgery. It is important to keep in mind that many physicians will make recommendations based on general surgical patients, and must be informed of the differences as they relate to oral surgery. There have been a number of studies in the past few decades that have documented the ability to achieve hemostasis in patients who do not have cessation of therapy. Malmquist and colleagues noted that there was no significant difference in hemostasis in a group of patients on oral anticoagulants who used hemocon dental dressing and the control group. Hence, there is a pronounced shift toward doing minor surgical procedures while maintaining some degree of anticoagulation therapy.
Despite this trend, there are those who argue for a more cautious approach, indicating that the problems of postoperative bleeding are not insignificant. Todd, in an article in 2003, further states that the instances of serious complications as a result of withholding oral anticoagulants are not as frequent as was once thought and that some may have been attributable to prolonged withdrawal of warfarin beyond what is normally recommended. He goes on to advocate guided withdrawal for moderate-risk to high-risk patients and those undergoing more extensive oral surgery, with bridging therapy for some patients based on their risk profile.
Of the previously listed conditions that require some alteration of coagulation, the major ones that require full anticoagulation therapy are patients with mechanical cardiac valves, atrial fibrillation, pulmonary embolism, and those with a history of a recent DVT or ischemic stroke. The possible life-threatening complications that may result from cessation of therapy in these patients would dictate consideration of local hemostatic measures for minor surgical procedures while having them remain on anticoagulation treatment or doing the procedures in a hospital setting.
As has been previously stated, the historical standard of care for managing patients on oral anticoagulant therapy was to stop the medication for a number of days before surgery and check the INR. If it was close to the normal range, then surgery was performed. Patients who were considered high risk and who could not be kept on these medications were hospitalized and switched to heparin, which has a shorter duration of action. The surgery was performed after briefly stopping the heparin. Once hemostasis was ensured, heparin was restarted and later switched to the oral anticoagulant. This is logistically more difficult and costly and involves hospitalization. Now, however, there are a greater variety of approaches to treat these patients, further contributing to the controversy that persists on how best to manage them.
There are 5 different approaches that can be used for patients who are fully anticoagulated that require minor oral surgery, which we will classify as categories 1 to 5:
- 1.
Cessation of OAT
- 2.
Cessation of OAT with bridging IV heparin therapy
- 3.
Cessation of OAT with bridging low molecular-weight SC heparin therapy
- 4.
Decrease in dosage of OAT
- 5.
Maintenance of OAT.
The first method is the traditional way in which we have handled these individuals. Warfarin is stopped 3 to 5 days before surgery, a PT and INR are done and, if normal or near normal, the agreed upon surgery is performed. This would be done for patients who are considered low risks for thromboembolic phenomena as determined by their medical history in conjunction with their physician.
The second method is for high-risk patients, for example those with mechanical valves, recent ischemic stroke, or a recent episode of pulmonary embolism. These patients would be hospitalized and slowly switched to IV heparin over 3 to 5 days, and remain fully anticoagulated until a few hours before surgery, whereupon the heparin would be stopped. After the prescribed surgery is completed and hemostasis is achieved, IV heparin would be restarted and later that day OAT would also be restarted. Once the warfarin has achieved full anticoagulation, the IV heparin would stop.
The third method is for patients with medium surgical risk. This method has become more popular with the advent of LMWH drugs that are longer acting. OAT is stopped 3 to 5 days before surgery while LMWH is started. Upon completion of surgery, warfarin is started that same evening and LMWH is stopped when PT and INR indicate adequate anticoagulation.
The fourth method involves decrease of the dosage of warfarin to get the INR in a range of 2.0 to 2.5. Once that has been attained, the surgery is performed and the dosage is increased back to normal that same evening, provided adequate hemostasis is present.
The final method involves no alteration of OAT. The INR is still done on the day of surgery. If it is between 2.0 and 4.0, the surgery is performed using adequate local hemostatic measures, such as placement of cellulose sponges, packs, suturing, and hemostatic liquids. These patients should be followed closely for up to 5 days after the procedure. Patients at high risk for thromboembolism would fall into this category.
With all methods, the patient’s physician should be aware of the plan. It is imperative to have in place a variety of local hemostatic agents for use, a readily available oral surgical specialist back-up and close follow-up measures in place. It is important to remember that patients who are on anticoagulant therapy, who have surgery and are noted to have adequate hemostasis at the conclusion of the procedure, can have bleeding issues up to 10 days after surgery. This is not an infrequent occurrence, so follow-up surveillance must be in place.
Patients Who Are Fully on OAT
Over the past 10 years there has been a trend toward the fifth method, maintaining anticoagulant therapy for patients who are having minor surgical procedures, such as minor oral surgery. This is so because, as has been previously mentioned, cessation of therapy in high-risk patients has been linked to an increased incidence of strokes and cardiac events. An additional consideration is that there has been a shift toward doing more procedures, even on seriously ill patients, outside of a hospital setting. There has also been a plethora of better hemostatic agents that have been developed for local control of bleeding that have enabled this move. To better understand these agents and the mechanism of action, it is important to review the coagulation cascade and how different medications affect the various reactions (see Fig. 1 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


