Dentoalveolar surgery in children presents general dentists with unique challenges not encountered in adults. The long-term effects that treatments have on these children must always be taken into consideration. A clear understanding of the growth and development of pediatric patients is necessary to correctly identify dental abnormalities.
Dentoalveolar surgery in children presents general dentists with unique challenges not encountered in adults. The long-term effects that treatments have on these children must always be taken into consideration. A clear understanding of the growth and development of pediatric patients is necessary to correctly identify dental abnormalities.
The tooth bud is a collection of cells derived from the ectoderm of the first brachial arch and the ectomesenchyme of the neural crest cells. The formation of primary teeth is evident between 6 and 8 weeks in utero and the permanent teeth form in the twentieth week. The initial calcification of the primary teeth ranges from 14 weeks for the incisors to 19 weeks for the second molars. The permanent incisors calcify between age 3 and 4 months and the third molars calcify between 7 and 10 years. If the dentition does not develop at these times or there is an event that disrupts the formation, then tooth development ceases. The most common congenitally missing teeth are the third molars followed by the lateral incisors and the mandibular second premolars.
The eruption pattern of the primary and permanent dentition is of critical importance ( Table 1 ). If a tooth or teeth fail to erupt, the cause should be investigated. Possible reasons include but are not limited to tooth malposition, retained primary teeth, arch space/length discrepancies, obstruction by a supernumerary tooth or a cyst (usually seen in teens, such as keratocysts and dentigerous cysts), or tumors (usually seen in childhood, such as compound/complex odontomas and fibro-osseous lesions). An anomaly in dental growth and development may be indicative of a more ominous problem. Clinicians must be aware of possible systemic causes, including endocrine, nutritional, and genetic abnormalities. These can be manifested in a combination of oral and extraoral findings, such as those associated with ectodermal dysplasia.
| Deciduous Dentition | Permanent Dentition | ||||
|---|---|---|---|---|---|
| Tooth | Eruption (Mo) | Root Completion (Y) | Tooth | Eruption (Y) | Root Completion (Y) |
| Maxillary | Maxillary | ||||
| A | 7 | 1.5–2 | 1 | 7–8 | 10 |
| B | 8 | 1.5–2 | 2 | 8–9 | 11 |
| C | 16–20 | 2.5–3 | 3 | 11–12 | 13–15 |
| D | 12–16 | 2–2.5 | 4 | 10–11 | 12–13 |
| E | 21–30 | 3 | 5 | 10–12 | 12–14 |
| 6 | 6–7 | 9–10 | |||
| 7 | 12–13 | 14–16 | |||
| 8 | 17–21 | 18–25 | |||
| Mandibular | Mandibular | ||||
| A | 6.5 | 1.5–2 | 1 | 6–7 | 9 |
| B | 7 | 1.5–2 | 2 | 7–8 | 10 |
| C | 16–20 | 2.5–3 | 3 | 9–10 | 12–14 |
| D | 12–16 | 2–2.5 | 4 | 10–12 | 12–13 |
| E | 21–30 | 3 | 5 | 11–12 | 13–14 |
| 6 | 6–7 | 9–10 | |||
| 7 | 12–13 | 14–15 | |||
| 8 | 17–21 | 18–25 | |||
Finally, in 2003, approximately 12 of 1000 children were found victims of child abuse and neglect. Medical professionals (and conscientious providers) are obligated to document and report cases of suspected child abuse and neglect to the appropriate law enforcement agency. It is estimated that more than half of the cases of child abuse involve the head, face, and neck. It is likely that you will encounter such cases while in practice and you must act in the best interest of the victim who is most often helpless.
Impacted teeth
The management of impacted teeth requires an understanding of the cause, treatment options, and outcomes. Open dialog between general practitioners, pediatric dentists, oral surgeons, and orthodontists is critical for a successful outcome. This section reviews the incidence, causes, diagnosis, and management of impacted teeth other than third molars.
Incidence
The most common impacted permanent teeth after third molars are maxillary canines, mandibular second premolars, and maxillary incisors. Rates of impacted permanent teeth vary among populations and range from 1% to 5%. Although any tooth can become impacted, most studies agree that the maxillary canine has the highest rate of impaction followed by mandibular second premolars, maxillary second premolars, mandibular second molars, and maxillary incisors. Eruption failure of mandibular incisors is rare and is often associated with pathologic conditions.
Rates of maxillary canine impaction approach 2% of the general population. Of these, 8% show bilateral involvement. This is greater than 5 times the rate of mandibular canine impactions (0.35%). Female patients are twice as likely to have an impacted canine as males. Jacoby found the rate of palatally impacted canines to labially impacted canines to be more than 6:1.
Relative to the permanent dentition, primary teeth rarely become impacted. When it occurs, it is most often a mandibular molar. It is important to distinguish between an impacted primary molar and one that appears “submerged” relative to the normal eruption of the adjacent permanent teeth. A congenitally missing succedaneous tooth allows prolonged retention of the primary tooth and often results in ankylosis. As the adjacent permanent teeth erupt, the retained primary tooth takes on a submerged appearance.
Etiology
Before treatment, the cause of an impacted tooth must be ascertained. In general terms, causes of impacted teeth can be categorized into localized mechanical obstruction or systemic abnormalities. Mechanical obstruction can be attributed to arch length deficiency, premature loss of deciduous teeth, prolonged deciduous tooth retention, supernumerary teeth, odontogenic tumors/cysts, abnormal eruption path, and cleft lip and palate ( Fig. 1 ).

Systemic causes include hereditary conditions, such as cleidocranial dysplasia (dysostosis) (CCD) and Down syndrome. Other systemic causes include endocrine dysfunction, febrile diseases, and irradiation. Radiographs of patients with CCD show many retained deciduous teeth with unerupted permanent and supernumerary teeth, frequently with distorted crowns and roots. Extraction of the retained deciduous teeth does not promote eruption of their permanent successors so surgical exposure and orthodontic traction is often necessary.
Evaluation
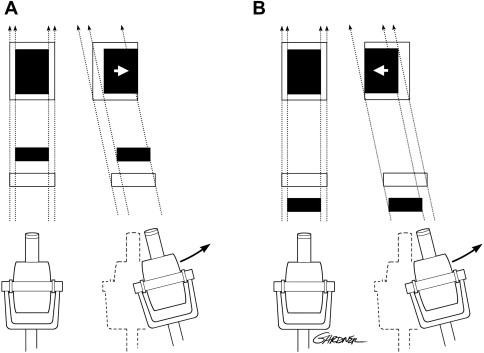
After determining the cause of an impacted tooth, clinicians must devise a treatment plan. Clinical signs of abnormal exfoliation and eruption sequences necessitate that clinicians act early, thus preventing future problems. The initial radiographic examination should include a panoramic radiograph supplemented with a variety of other modalities to determine the position of the impacted tooth in 3-D. Aside from determining horizontal and vertical positions of teeth, panoramic radiographs can aid in determining buccal-lingual positions. A tooth that is positioned outside of the radiographic trough appears out of focus and larger or smaller than the adjacent teeth. If positioned palatal to the adjacent teeth (ie, further from the x-ray film), a larger image can be expected ( Fig. 2 ). Alternatively, a smaller image can be expected if the tooth is positioned labial to the focal trough.

When the location of an impacted tooth is not obvious, a series of periapical radiographs is used to determine tooth position. This technique is commonly referred to as the tube-shift technique or Clark’s rule. To use Clark’s rule, an initial periapical radiograph is taken in the standard fashion. A second periapical radiograph is then taken after moving the beam source mesially or distally. If an impacted tooth appears to move in the same direction as the beam, it is located lingual or palatal to the adjacent teeth. If it moves in the opposite direction, the tooth is buccal or labial to the adjacent teeth. The common acronym for this is SLOB (same-lingual, opposite-buccal) ( Figs. 3–5 ). Often impacted teeth can be located in the middle of the alveolus or angulated so that half of the tooth is on the buccal side and half on the palatal. In these circumstances, an occlusal radiograph is valuable.


Treatment Options
After determining the location and the cause of an impacted tooth, clinicians should consider the treatment options and determine if referral to a specialist is warranted. Decisions on extraction are based on associated pathologic conditions, tooth position, feasibility of orthodontic alignment, and patient cooperation. Studies by Stivaros and Mandall evaluated the radiographic appearance of teeth and the decision to extract or bring the tooth into the arch. As the angulation of a tooth to the midline increased, it was more likely to be extracted. Palatally impacted teeth were more likely to be retained and brought into the arch than labially positioned teeth. Other treatment options include serial extractions and spontaneous eruption, exposure and spontaneous eruption, exposure with orthodontic traction, autotransplantation, extraction with prosthetic replacement, and no treatment.
Examples
Maxillary canines
To understand the cause of maxillary canine impaction it is important to consider the timing of its development and the surrounding anatomy. The maxillary canine bud is positioned high in the maxilla between the nasal cavity and the orbital rim. Posteriorly, this space is limited by the anterior sinus wall. As root formation progresses, the crown of the canine contacts the roots of the lateral incisor mesially, the first premolar distally, and the resorbing roots of the deciduous canine. Theoretically, these teeth guide the developing canine into its proper position in the arch. When anomalies exist in lateral incisor and premolar form and position, the canine wavers from its expected eruption path and can become palatally or labially impacted.
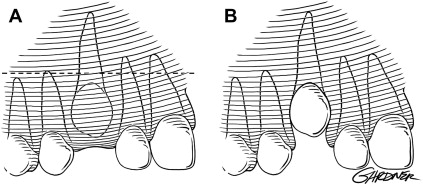
Palatal impactions are more common because there is more palatal space into which the canine drifts. This is caused by (1) excessive bone growth in the canine area, (2) agenesis or hypodevelopment of the lateral incisor, and (3) stimulated eruption of the lateral incisor or the first premolar. In approximately 13% of cases, the canine becomes labially displaced. This situation, however, probably does not represent a true impaction because these teeth have been shown to spontaneously erupt if given adequate space. Some foretelling signs of maxillary canine impaction include prolonged retention of the deciduous canine (beyond 14 years), presence of a palatal bulge or absence of a labial canine bulge beyond age 11, and abnormal lateral incisor shape or position. Ericson and Kurol found in a study of 505 children between the ages of 10 and 12 that only 5% had nonpalpable canines at age 11.
Treatment
In select cases, prevention of canine impaction can be accomplished by extraction of deciduous canines as early as 8 or 9 years of age. These cases are usually limited to dental class 1 patients without crowding. Ericson and Kurol found that the position of the ectopically erupting canine can be normalized in 91% of cases if the canine crown is distal to the midline of the lateral incisor. The success rate decreases to 64% when the canine crown is mesial to the midline of the lateral incisor.
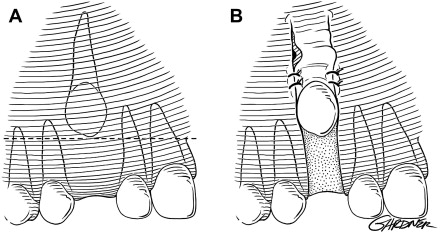
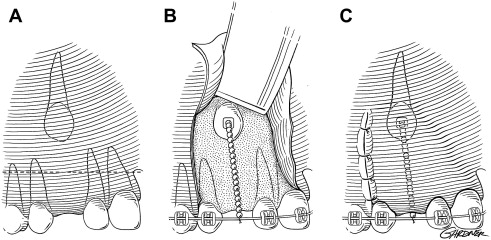
After clinically and radiographically determining the position of a canine, it can be exposed via (1) excisional uncovering, (2) apically positioned flap, or (3) closed eruption techniques. Tooth position and the amount of attached gingiva in the area help determine the correct procedure. Excisional uncovering is usually done after sufficient space is created for eruption of the permanent canine. The procedure is reserved for the palatally impacted canine; however, it can be performed on a labially positioned tooth if there is sufficient attached gingiva in the area to provide 2 mm to 3 mm of gingival cuff after eruption. Without an adequate gingival cuff, the erupting canine is predisposed to future periodontal problems. This procedure is performed when the majority of the crown is above the mucogingival line and there is little alveolar bone to remove. When the impacted tooth is vertically aligned and there is no obstruction, spontaneous eruption usually occurs. Excisional uncovering should not be attempted if the tooth is positioned within the center of the alveolus or apical to the mucogingival line. In this situation, a closed technique or apically positioned flap is indicated ( Fig. 6 ).
Exposure of a labially positioned canine is often accomplished using an apically positioned flap. This procedure is indicated if there is insufficient attached gingiva to provide a 2-mm to 3-mm cuff around the erupting tooth and should only be performed if the impacted tooth is near the alveolus. In high impaction cases, the use of an apically positioned flap can result in significant re-intrusion of the impacted tooth after orthodontic therapy. Before surgery, adequate arch space for eruption is usually obtained by an orthodontist. Vertical releasing incisions are made on each side of the edentulous space with the base wider than the apex. A horizontal incision is made over the edentulous alveolar ridge, connecting the 2 vertical incisions and incorporating attached gingiva. A full-thickness mucoperiosteal flap is then reflected apically past the level of the impacted tooth. Bone is removed as necessary from around the crown, and an orthodontic bracket and chain can be attached. The flap is then sutured apically to allow for simultaneous descent of the gingival tissue with the tooth during orthodontic traction ( Fig. 7 ).
The closed eruption technique is used for high palatal or labial impactions. In this situation, excisional uncovering or apically positioned flaps is difficult or results in periodontal compromise. The impacted tooth is exposed (in the manner described previously), an attachment with a chain is secured to the tooth, and the chain is sutured to the arch wire for later activation. The flap is replaced with the chain exiting near the alveolar ridge space where the tooth is expected to erupt. The orthodontist then uses the chain to apply traction on the impacted tooth ( Fig. 8 ). In a 30-patient study comparing labially impacted teeth treated with apically positioned flaps with those treated with the closed eruption technique, Vermette and colleagues found that more periodontal and esthetic disadvantages can be expected with the apically positioned flap technique. Those treated with apically positioned flaps were shown to have clinically increased crown lengths, gingival scarring, and intrusive relapse when compared with the closed eruption group.
Premolars
Premolar impactions are more common in the mandible than maxilla. They occur more often in the center or lingual aspect of the alveolus. If the impactions are a result of an arch length discrepancy, consultation with an orthodontist should take place ( Fig. 9 ). When adequate space exists to accommodate moving the tooth into the arch, the impacted premolar can be treated with the same techniques as for the impacted canine (described previously).

Incisors
Impacted maxillary incisors commonly result from premature loss of the primary incisors or trauma. Radiographs are used to find the location of the impacted tooth and determine root development. If root development is not complete, soft and hard tissue removal is often adequate to promote spontaneous eruption. If root formation is complete or the inclination of the tooth is expected to prevent normal eruption, exposure should include bonding of an orthodontic bracket and chain to allow for orthodontic forces.
Molars
Impactions of permanent first and second molars are rare. If left untreated, the resulting periodontal defects, caries, and resorption can leave a patient without a functioning posterior dentition. Intervention before complete root formation is paramount to a successful outcome. Asymmetric first molar eruption patterns before age 7 should raise suspicion and warrant radiographic examination. After age 7, spontaneous first molar eruption is nearly impossible. Treatment options of unerupted molars include surgical exposure and uprighting, extraction with implant replacement, or a combined surgical and orthodontic correction. Orthodontic correction is often complicated because of limited access and insufficient anchorage, although with the current advances in orthodontic anchorage, this is becoming less of a problem. Patient compliance is also a concern because of the increased treatment time.
Surgical uprighting of a mesially inclined second molar provides a predictable answer if performed at the right time. This procedure is best accomplished when two-thirds of root formation has been completed. If performed after root development is completed, a restricted blood supply from the constricted apical foramen can result in pulpal necrosis. Complications of surgical uprighting include pulpal necrosis, root fracture, dilacerations, internal and external resorption, and periodontal complications. In Dessner’s retrospective study of 34 patients treated by surgical uprighting of mandibular second molars, however, 31 molars showed complete bony fill of the space previously occupied by the crown of the uprighted tooth. Only 12 of the 34 teeth showed pulpal changes, and there was no incidence of periapical pathology.
Extraction of Impacted Teeth
The decision to surgically remove an impacted tooth is considered when no other treatment is feasible. When considering removal of an impacted tooth, many factors should be considered, including patient age, associated pathology, severity of impaction, and morbidity associated with the procedure. Anterior teeth are approached from the surface to which they are most closely associated. A full-thickness flap without release is used to expose impacted teeth on the palate.
Extraction of impacted premolars can be challenging because of limited access, adjacent roots, the maxillary sinus, or the mental nerve in the mandible. Extraction of maxillary bicuspids is accomplished in a fashion similar to that of anterior maxillary teeth. Mandibular bicuspids are usually approached from the buccal surface. When access is limited as a result of a lingually impacted premolar, buccal and lingual flaps are used. The lingually impacted premolar is one of the most difficult extractions encountered.
Orthodontic Anchorage
Orthodontic treatment is a complex process that involves the transmission of constant forces to influence tooth movement with the goal of alignment within the alveolus. Anchorage is often the limiting factor when deciding to treat a case with orthodontics alone or in combination with surgery. Specifically, intrusion of posterior teeth to correct an anterior open bite and distal movement of posterior teeth to correct a class 2 or 3 malocclusion presents significant anchorage challenges.
To supplement orthodontic anchorage, various intraoral and extraoral appliances have been used with varying degrees of success. These include headgear, lip bumpers, Herbst appliances, magnets, and multiloop edgewise archwires. Unfortunately, these devices are cumbersome and become ineffective when patient cooperation fades. Surgical correction of skeletal malocclusions is often indicated for these patients with varying acceptance rates. Advances in skeletal orthodontic anchorage over the past 25 years have revealed other options for these patients.
Multiple skeletal anchorage systems exist. Their versatility in size and shape allow them to be placed in anterior and posterior locations of both arches. Common sites for placement include the maxillary buttress and anterior ramus areas. Ease of placement and removal is a clear advantage; however, many clinicians recommend a healing period for osseointegration before applying orthodontic forces. Examples of skeletal fixation for orthodontic anchorage include miniplates fashioned to the posterior mandible or maxilla, microimplants in interdental locations, and palatal implants for distalization of maxillary molars. Miniplates have been used in the posterior maxilla and mandible to intrude molars while closing anterior open bites. In a study by Sherwood and colleagues, anterior open bites were effectively treated by intrusion of maxillary molars using miniplates for anchorage. The miniplates used for fixation proved stable against orthodontic forces, which intruded maxillary molars between 1.45 and 3.32 mm. Miniplate anchorage has also proved effective in the distalization of maxillary and mandibular molars. By fixating miniplates to the anterior ramus, Sugawara and colleagues showed that mandibular molars could be distalized (average of 3.5 mm at the crown level and 1.8 mm at the root level) with minimal relapse (0.3 mm) at 1-year follow-up.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


