Mini-implants are becoming increasingly popular in orthodontic practice. However, there is still controversy about the need for implant-site preparation. This article reviews the current literature to answer the question: is predrilling is necessary for orthodontic mini-implants?
Over the past years, orthodontic mini-implants have become a standard in modern orthodontic practice, and the ability to move teeth in a never-before fashion has been demonstrated in many articles. Therefore, it appears that there are great benefits to this new treatment approach.
However, an area where enthusiasm is not so great is the clinical success rates. Orthodontic mini-implants are lagging behind their prosthodontic counterparts, which excel with clinically high success rates of 98% to 99%. This might not come as a surprise, since temporary anchorage devices are, as the name indicates, intended for temporary use, and full osseointegration is not intended. The literature reports a wide range of overall success rates for temporary anchorage devices ranging from 70% to 91.6% depending on the study design. However, in the studies’ subgroups, an even greater spread can be observed, ranging from 60% to 100% depending on the factors investigated. Studies reporting the highest success rates (98.1%-100%) focused on the insertion torque (IT) of the orthodontic mini-implant. Therefore, it appears that IT has a strong impact on clinical success rates. Other factors such as bone quality, cortical-bone thickness, mini-implant design, and implant-site preparation (predrilling) can affect the IT of the mini-implant.
The marketplace offers drill-free and nondrill-free mini-implants. Whereas predrilling is always necessary for nondrill-free thread designs, it is technically not required for the drill-free design. Nevertheless, some authors claim that there might be a benefit to predrilling under certain circumstances, even with drill-free mini-implants.
The purpose of this article was to present a review of the literature to answer the question whether predrilling of the implant site is useful under certain circumstances and, if so, to issue guidelines for implant-site preparation. The important parameters are the following.
- 1.
Mini-implant IT. The amount of torque during the placement of an implant reflects the resistance the mini-implant encounters when advancing into the bone. This resistance is proportional to the amount of bone compression during placement and therefore increases with greater cortical-bone thickness. It can also serve as an indirect measure for the primary stability of the mini-implant.
- 2.
Primary stability. According to Melsen and Costa, primary stability is an important factor for mini-implant success. Primary stability expresses the initial stability of a recently placed implant. It is a function of the mechanical retention of the implant in the bone and is therefore greatly influenced by the design of the implant shank and the density and amount of the implant bed bone. Primary stability is important during the healing and remodeling period, especially when the implant is immediately loaded.
- 3.
Secondary stability. Secondary stability is the implant’s stability after the placement site has healed and is a consequence of bone formation and remodeling at the implant-bone interface and the surrounding bone. It therefore is a result of the host’s response to the implant and is determined by biologic reactions in addition to mechanical retention. Secondary stability is responsible for implant success after the healing period and is the determining factor for success during most of the loading period.
The goal of guidelines for implant-site preparation is to maximize clinical success rates of orthodontic mini-implants. For an implant to be successful, it must remain stable during the loading period; ie, it must have both adequate primary and secondary stability.
Primary stability is a mechanical factor that can be assessed indirectly by IT. The relationship is as follows: high IT results in high primary stability. In this respect, increased IT can be interpreted as favorable.
Secondary stability is a biologic factor that is greatly influenced by the host’s response to the implant. A positive response resulting in high secondary stability requires healthy hard and soft tissues surrounding the implant site. High IT carries the risk of mechanical damage to the peri-implant tissues. Excessive bone compression has been proven to cause cell death and necrosis, which can lead to peri-implant bone resorption. Soltesz et al and Huiskes and Nunamaker demonstrated a direct correlation between high-stressed regions in the bone and resorption. In light of this knowledge, excessively high IT should be regarded as unfavorable.
High IT increases primary stability and at the same time affects the tissues of the implant bed negatively, reducing secondary stability. Clinically, a mini-implant placed with excessive IT would have adequate primary stability but over time become loose and fail.
In an ideal world, one would search for a compromise, a specific torque range that would be great enough to provide sufficient primary stability to ensure good clinical success yet low enough to maintain the vitality of the surrounding tissues to generate a favorable host response and thus enhance secondary stability. Can such a torque range be identified? In a study by Motoyoshi et al, the overall success rate of the orthodontic mini-implants was 85.5%. The subgroups, however, had a significant difference. When mini-implants were placed with less than 5 Ncm of torque, the overall success rate dropped to 72.7%. When the IT was between 5 and 10 Ncm, the overall success rate increased to 96.2%. When the IT was greater than 10 Ncm, the overall success rate dropped to 60.9%. This study suggests that, if the IT is limited to 5 to 10 Ncm, significantly higher success rates can be expected. One explanation for the reported findings could be that, below 5 Ncm, mini-implants lack mechanical retention and primary stability; above 10 Ncm, sufficient trauma to the surrounding tissues is inflicted so that bone remodeling is adversely affected,. resulting in lack of secondary stability.
Many factors can affect IT. One of the strongest correlations was demonstrated by Wilmes et al between cortical-bone thickness and IT. With the parameters defined in that study (1.6 × 8 mm self-drilling implant, predrill: diameter 1.0 mm; 3 mm depth), the ideal torque range of 5 to 10 Ncm was achieved only at sites where the cortical-bone thickness was approximately 0.5 to 1 mm thick. However, most placement sites provide greater cortical-bone thickness than that. Predrilling is an effective method of decreasing the resistance encountered during placement and thus reducing IT. Therefore, in areas of increased cortical-bone thickness, predrilling can be recommended if the objective is to remain in the ideal torque range. With self-drilling implants, the predrilling procedure does not need to extend into the bone the entire length of the implant. However, the farther the pilot hole extends into the bone, the greater the reduction of IT. Also, the larger the diameter of the pilot hole, the greater the reduction in IT. At a minimum, the width of the pilot hole should be 65% of the outer core diameter of the implant. It can be increased up to 85% without affecting the pull-out resistance of the mini-implant.
To implement the above recommendations, it is essential to understand how to gauge cortical-bone thickness.
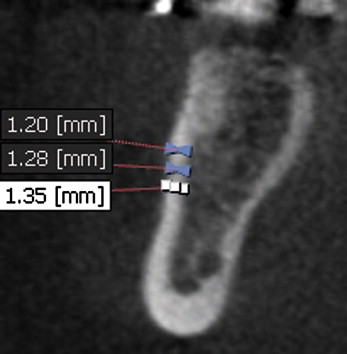
The most precise method for determining cortical-bone thickness is to use computed tomography or cone-beam computed tomography technology to image the region of interest and then generate direct measurements at the planned placement site ( Fig 1 ). Current 3-dimensional digital imaging systems, however, tend to slightly underestimate the actual size of the object. Although this is minimal, it might have an impact when measuring small objects.
Another alternative is to use average data as generated from a representative sample. Baumgaertel and Hans created a thickness chart for buccal cortical-bone thickness that gives a good general indication of the bone thickness to expect at buccal placement sites. Lim et al published similar findings, and Kim et al presented cortical-bone thicknesses for important placement sites.
A third alternative—the least precise and practicable, however—is to gauge cortical-bone thickness during the predrilling procedure because the dimensions of the drill are known, and one can feel when the cortical bone has been completely perforated.
Discussion
The clinical success of orthodontic mini-implants depends on many factors such as implant site, type of implant, and placement protocol. However, one of the most influential factors of clinical success appears to be IT.
The recommendations for implant-site preparation presented here were derived from a nonsystematic review of the literature aimed to identify the range of success rates reported (highest and lowest) and the factors that lead to achievement of the maximums. For this, a PubMed search was conducted ( http://www.ncbi.nlm.nih.gov/sites/entrez?db=pubmed ) by using the key words “mini-implant(s) + success” and “miniscrew(s) + success,” followed by a manual search for related articles in the reference citations of published articles. One problem, however, was that there is no uniform definition of clinical mini-implant success. Therefore, direct comparison of various studies was difficult. However, even though most studies also had different protocols, it was evident that studies focusing on IT had the highest success rates. Therefore, studies reporting on mini-implant IT were subsequently searched for.
The study by Motoyoshi et al used absence of mobility as the definition of success; this appears to be the best definition, since any mobility means lack of absolute anchorage. The large sample size, sound statistical approach, and significant differences between the subgroups gave this study high validity. To increase clinical success with mini-implants, the recommendation of placing them with a medium torque range should be followed. Wilmes et al pointed out the strong correlation between cortical-bone thickness and IT and the need for implant-site preparation; that study was carried out on porcine iliac crest bone. Therefore, the findings cannot be transferred directly into clinical guidelines for mini-implants in humans. Nevertheless, it is clear that cortical-bone thickness is an important factor in the magnitude of IT.
Thicker cortical bone increases primary stability but might decrease secondary stability due to excessive bone compression if the site is not adequately prepared. Predrilling is a proven and successful way to reduce the amount of cortical bone that will be penetrated by the implant, and thus it aids in reducing resistance and controlling IT. Based on the above explained principles and the cited evidence, but adapted to placement in human jaws, the following guidelines can be given ( Table ). They were specifically developed for self-drilling mini-implants with a 1.6-mm outer core diameter and a 6-mm length. They appear to work equally well in both jaws, since they are not based on specific sites but only on cortical-bone thickness, which can vary greatly even within a small area. Clinical implementation is simplest when using the average cortical-bone thicknesses as published by Deguchi et al, Baumgaertel and Hans, Lim et al, and Kim et al. These guidelines can and should be adapted if used with mini-implants of other specifications. For example, a longer implant might require a deeper pilot hole. An implant with a larger outer core diameter could require a pilot hole that is larger in diameter. An implant of smaller diameter might require a pilot hole with a reduced diameter. Caution should be used with mini-implants of smaller diameters, since they have a reduced yield strength and are more prone to fracture under torque load.



